Translate this page into:
Use of real-time ultrasound for locating tip position in neonates undergoing peripherally inserted central catheter insertion: A pilot study
Reprint requests: Dr Srinivas Murki, Department of Neonatology, Fernandez Hospital, Hyderabad 500 033, Telangana, India e-mail: srinivasmurki2001@gmail.com
-
Received: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Securing long-term venous access is an essential part of sick newborn care. The malposition of central line tip leads to several complications. There is a need for an easily available bedside investigating tool to diagnose these malpositions. This study was done to compare the effectiveness of real-time ultrasound (RTUS) with X-ray in identifying the peripherally inserted central catheter (PICC) line tip.
Methods:
This pilot observational study was conducted in a level III Neonatal Intensive Care Unit of a tertiary care hospital in India, from June 2012 to June 2013. A total of 33 PICC lines in 31 infants were included in the study. After insertion of PICC line, X-ray and RTUS were done to locate the tip of the PICC line.
Results:
In this study, PICC line tip could be identified by bedside RTUS in 94 per cent of line insertions. Standard X-ray identified the tip in all cases. RTUS has been shown to have good diagnostic utility in comparison with X-ray with sensitivity and specificity being 96.55 and 100 per cent, respectively. In our study, majority of malpositions were identified and manipulated by RTUS, thus second X-rays were avoided.
Interpretation & conclusions:
The result of this pilot study shows that RTUS may be a reliable and safe bedside tool for determining the tip of PICC lines. However, studies with large sample size need to be done to confirm these findings.
Keywords
Peripherally inserted central catheter
real-time ultrasound
X-ray
Peripherally inserted central catheter (PICC) is one of the novel approaches to gain long-term venous access in sick neonates1. Although fluoroscopy is the gold standard for locating PICC line tip, most of the neonates who undergo this procedure are sick and cannot be transported. The use of contrast while taking radiographs for the localization of long line position improves the likelihood that an observer can see a long line tip and reduces inter-observer variability, but in sick neonates with deranged renal parameters it may not be feasible and contrast may effect thyroid function also23. Position of PICC line can also be confirmed by various methods such as plain/digital/contrast radiography4, electrocardiogram567, echocardiography (ECHO)8 and ultrasound91011. A single anteroposterior chest radiograph is the most commonly used method to confirm appropriate PICC line position in sick neonates. In addition, a lateral chest radiograph may be utilized to further delineate the tip position. In many neonates, first-time insertions are often malpositioned, necessitating either removal or reposition and repeat X-ray exposures. Availability of bedside ultrasound in the Neonatal Intensive Care Units (NICUs) and its use for localizing the PICC or central line tip position may decrease the time taken for insertion, increase the success of line placement on the first attempt and reduce manipulations and X-ray exposure and overall complication rates1213. Previous studies reported 85-90 per cent specificity for identifying PICC line tip position in newborns141516. This pilot study was planned to look whether using real-time ultrasound (RTUS) instead of X-ray can reduce malposition rates and X-ray exposures. The primary objective of the study was to estimate the diagnostic utility of RTUS in detecting malposition of tip of central lines while taking X-ray as gold standard for identifying PICC tip position. Secondary objectives were to estimate the reduction in the number of X-ray exposures done solely for the purpose of locating the central line tips, to estimate failure rate of detecting the catheter tip using RTUS.
Material & Methods
This observational study was conducted in a level III NICU of Fernandez hospital, Hyderabad, India, from June 2012 to June 2013. All neonates undergoing peripherally inserted central venous line insertions were eligible for the study. Written informed consent was obtained from parents before enrolling the neonates in the study.
Experimental protocol: A total of 33 PICC lines in 31 infants, who were consecutively catheterized with PICC, were included in the study. Baseline data variables such as gestation, birth weight of the neonate, gestational age at insertion and indication for PICC were noted in a predesigned proforma. The decision to insert central line was as per the existing protocol of the unit. When the line was inserted in the upper limb, the length of insertion was a straight line measured from the point of insertion to the right sternoclavicular joint and then perpendicularly till manubrium sternum. For lower limb insertion, the length of insertion was a straight line measured from the point of insertion to the umbilicus. After insertion of PICC line, X-ray and RTUS were done to localize the line tip.
X-rays were taken by keeping the neonate in neutral position. X-rays were reported by a neonatologist who was not aware of the ultrasound findings. All the X-rays were reported in a pre-designed reporting form. X-ray was done as soon as possible after inserting PICC line.
RTUS was done immediately after the X-ray, using an Esaota ultrasound machine (Italy) and a sector probe which has frequency range of 5-12 Hz (the machine changes frequency by itself as per the image clarity). The neonates were evaluated for PICC line position with vena caval views and also confirmed in other views. All the images were stored for quality review by a senior consultant neonatologist. If the tip was away from the desired position, catheter was repositioned accordingly till it came to lie in the desired position. If the tip was not visualized properly, 2-3 ml of normal saline was injected and bubbling at the tip was noted.
Ideal tip positions:
Upper limbs: The tip of the line at the junction between superior vena cava and right atrium.
Lower limbs: The tip of the line at the junction between inferior vena cava and right atrium.
Tip not in ideal position was defined as malposition.
Statistical analysis: All categorical variables were expressed in proportions while continuous variable were expressed in either mean±standard deviation or median (interquartile range). Sensitivity, specificity, positive and negative predictive values and likelihood ratios were calculated for RTUS.
Results
The mean gestational age was 30.63±3.4 wk and the mean birth weight was 1352.4±562g (n=31). Fifty per cent of the enrolled neonates were male; 86 per cent were delivered by caesarean section. Nineteen infants were on mechanical ventilation and nine infants were on bubble continuous positive airway pressure at the time of PICC line insertion. Thirty one infants received total parenteral nutrition through the PICC line. PICC line was inserted in the upper limb in 10 infants (28.5%) and in the lower limb in the remaining.
Using RTUS, PICC line position and tip were identified in 21 and in additional 10 lines; the position and tip were localized after a saline bolus. Thus, RTUS was able to identify the PICC line tip in 31 out of 33 line insertions (94% of PICC line insertions). In one infant, PICC line tip identification was precluded due to gaseous abdomen, and in another infant, it was located in the common iliac vein. Both the lines not identified on the RTUS could be localized on the abdominal X-ray. We assumed non-identified PICC positions on RTUS as malposition. All the normally positioned lines on the X-ray were also in normal position as seen by RTUS. X-ray showed malposition of lines in four infants, and of these, three malpositions were identified on the RTUS with line positions adjusted (Table). Of the four infants with malposition of the lines on the X-ray, one was in subclavian vein, one in right atrium, one in right brachiocephalic and one in the common iliac vein. Three of the four malpositions were manipulated under ultrasound guidance avoiding a repeat X-ray.
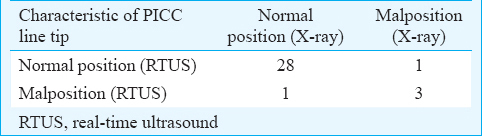
The calculated sensitivity, specificity, positive and negative predictive values are 96.55 [95% confidence interval (CI): 82.17-99.42%], 100 (95% CI: 30.48-100.00%), 100 (95% CI: 87.54-100.00%), and 75 per cent (95% CI: 20.34-95.88%), respectively. The positive likelihood ratio was not calculated as specificity was 100 per cent while negative likelihood ratio was 0.03 (95% CI: 0.01-0.240) and the area under the curve being 0.85 (95% CI: 0.63-1.00) (Figure).

- Area under receiver operating characteristic curve with ultrasound as surrogate and X-ray as gold standard.
The mean duration of the PICC line was 7±2.14 days. Line-related complications were observed in eight (24%) of the 33 PICC line insertions. Thrombosis in three infants, limb swelling in three infants and redness along the line insertion were the main complications. One infant developed bilateral pleural effusion on the third day of line insertion. The overall failure rate of RTUS in identifying PICC position was only six per cent.
Discussion
In this pilot study, PICC line position could be identified by the bedside RTUS in 94 per cent of line insertions, though majority of the line insertions were in the lower limb. Plain X-ray identified the lines in all newborns, and in four infants, the line was malpositioned. RTUS identified three of these four malpositions. However, unlike many other studies14151617, all normal positions on the X-ray were found to be on normal positions on the ultrasound. RTUS appears to be a good bedside tool in the identification of PICC line positions. If appropriately used, it can prevent many X-ray exposures of the neonates.
Unlike our study, in the study by Jain et al17, concordance between radiographs and neonatal-targeted ECHO for PICC line tip position occurred in 59 per cent infants. Sensitivity of radiographs in determining malpositions was 64 per cent with a specificity of 55 per cent. Three infants were incorrectly identified to have deep lines and two infants were incorrectly identified to have short lines. In nine infants (41%), a second radiograph was avoided following line manipulation17. In our study, second radiograph was avoided in three of the four malpositions identified on the X-ray. Saline was used to see the bubbles on RTUS. This might have helped us in better detection of PICC tip position.
Madar and Deshpande14 in their pilot study on 28 infants for the evaluation of ultrasound for identifying the position of neonatal central catheters showed that RTUS was successful in localizing the tips of central catheters and showed their precise relation to the cardiac chambers and major aortic branch vessels. After the placement of a central catheter, its position was checked by a plain X-ray with simultaneous ultrasound assessment of the catheter position. A total of 40 central catheters were inserted in these infants. The RTUS was not able to identify only two catheters, one infant had a very tender abdomen, making the examination difficult; in the other infant, the catheter tip was situated high in the superior vena cava14. In our study, in one infant, PICC line tip identification was precluded due to gaseous abdomen, and in another infant, it was located in common iliac vein.
Katheria et al18 in a randomized controlled trial comparing ultrasound-guided PICCs with standard radiographs in neonates reported that RTUS use significantly decreased the time of line placement by 30 min (P=0.034) and decreased the median number of manipulations (0 vs. 1, P=0.032) and radiographs (1 vs. 2, P=0.001) to place the catheters. They concluded that early identification of the PICC by RTUS was possible in all cases and would have saved an additional 38 min if radiographs were not required18. In our study, we did not calculate the reduction in time of line placement, manipulations and radiograph.
In conclusion, our study indicates good positive predictive value for RTUS and it may guide the clinician in emergency situations for starting fluids and medications earlier. The main limitations of the study were a small sample size and an inability to record the timings. Due to the small sample size, the specificity and negative predictive values showed wide confidence intervals. Hence, the results need to be verified by a study with adequate sample size.
Conflicts of Interest: None.
References
- Therapeutic techniques: Peripherally inserted central catheters in neonates. Neoreviews. 2004;5:e60-2.
- [Google Scholar]
- Does radio-opaque contrast improve radiographic localisation of percutaneous central venous lines? Arch Dis Child Fetal Neonatal Ed. 2004;89:F41-3.
- [Google Scholar]
- Digital imaging does not improve localization of percutaneously inserted central lines in neonates. J Paediatr Child Health. 2005;41:256-9.
- [Google Scholar]
- Are supine chest and abdominal radiographs the best way to confirm PICC placement in neonates? Neonatal Netw. 2010;29:23-35.
- [Google Scholar]
- Serendipitous ECG guided PICC insertion using the guidewire as intra-cardiac electrode. J Vasc Access. 2010;11:72.
- [Google Scholar]
- Intravenous electrocardiographic guidance for placement of peripherally inserted central catheters. J Electrocardiol. 2010;43:274-8.
- [Google Scholar]
- Endovascular electrocardiography to guide placement of totally implanTable central venous catheters in oncologic patients. J Vasc Access. 2011;12:348-53.
- [Google Scholar]
- Echocardiography allows more accurate placement of peripherally inserted central catheters in low birthweight infants. Acta Paediatr. 2013;102:703-6.
- [Google Scholar]
- Pediatric peripherally inserted central catheter placement: Application of ultrasound technology. J Infus Nurs. 2007;30:351-6.
- [Google Scholar]
- Placement of peripherally inserted central catheters in children guided by ultrasound: A prospective randomized, and controlled trial. Pediatr Crit Care Med. 2012;13:e282-7.
- [Google Scholar]
- Effect of using static ultrasound technique on peripherally inserted central catheters'insertion success rate in neonates in a Neonatal Intensive Care Unit. Iran J Nurs Midwifery Res. 2014;19:643-6.
- [Google Scholar]
- Ultrasound-guided umbilical catheter insertion in neonates. J Perinatol. 2011;31:344-9.
- [Google Scholar]
- Placement of umbilical venous catheters with use of bedside real-time ultrasonography. J Pediatr. 1995;126:633-5.
- [Google Scholar]
- Reappraisal of ultrasound imaging of neonatal intravascular catheters. Arch Dis Child Fetal Neonatal Ed. 1996;75:F62-4.
- [Google Scholar]
- Percutaneous central venous catheterization via the great saphenous vein in neonates. Acta Paediatr Jpn. 1997;39:312-6.
- [Google Scholar]
- Central venous silastic catheters in newborns: Localization by sonography and radiology. Pediatr Radiol. 1987;17:15-7.
- [Google Scholar]
- The use of targeted neonatal echocardiography to confirm placement of peripherally inserted central catheters in neonates. Am J Perinatol. 2012;29:101-6.
- [Google Scholar]
- A randomized controlled trial of ultrasound-guided peripherally inserted central catheters compared with standard radiograph in neonates. J Perinatol. 2013;33:791-4.
- [Google Scholar]






