Translate this page into:
Unenhanced renal magnetic resonance angiography in patients with chronic kidney disease & suspected renovascular hypertension: Can it affect patient management?
Reprint requests: Dr J. Yamuna, Department of Radiology & Imaging Sciences, Sri Ramachandra Medical College & Research Institute, Chennai 600 116, Tamil Nadu, India e-mail: ammuz1221@gmail.com
-
Received: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Renal artery stenosis (RAS) is an important cause of severe hypertension in patients with chronic kidney disease (CKD). It is important to detect RAS early as it can reverse hypertension and stop rapid deterioration of renal function. The potential drawbacks of various imaging modalities used to detect RAS including contrast-related adverse effects associated with diagnostic angiography have led to increasing interest in unenhanced magnetic resonance (MR) renal angiography. The aim of this study was to detect and grade RAS in patients with CKD and suspected renovascular hypertension using unenhanced MR angiography (UMRA) and to identify patients with significant RAS (>70%) who would subsequently require further investigation and revascularization.
Methods:
Thirty five CKD patients with suspected RAS were subjected to UMRA using non-contrast MR angiography of ArTery and VEins 3D True fast imaging with steady state precession technique over a three year period. Patients with RAS >70 per cent on UMRA were subjected to digital subtraction angiography (DSA) with intervention if indicated.
Results:
In all, 76 renal arteries were evaluated using UMRA in 35 patients, of which 18 arteries showed stenosis and 11 were haemodynamically significant (eight patients). Seven patients (10 renal arteries) underwent DSA.
Interpretation & conclusions:
An association between UMRA and DSA findings was obtained in six patients (nine renal arteries), and these patients were stented. Post-procedure follow up showed good improvement in blood pressure and renal function. UMRA was found to be a useful non-invasive imaging modality to detect RAS in CKD patients. It can identify patients who require further invasive angiography and revascularization.
Keywords
Angiography
chronic renal failure
non-contrast magnetic resonance angiography
renal artery stenosis
Renovascular hypertension (RVH) is the most common type of secondary hypertension i.e. hypertension with a known cause, and accounts for 1-5 per cent of the general hypertensive population1. It is defined as the causal relationship between renal artery stenosis (RAS) and its clinical consequences2. RVH has a higher prevalence in patients with severe hypertension and end-stage renal disease3. The prevalence of RAS in chronic kidney disease (CKD) has been reported to be 5.5 per cent4. Dworkin and Cooper4 have shown the increased rates of CKD (25 vs 2%), coronary artery diseases (67 vs 2%) and stroke (37 vs. 12%) in patients with RAS as compared to the normal population, thus implying the importance of identifying this potentially reversible cause of hypertension. The causes of RAS include atherosclerosis, fibromuscular dysplasia (FMD) and other rare causes such as vasculitis, aortoarteritis, embolic disease, dissection and post-traumatic occlusion5. Of these, atherosclerosis accounts for about 90 per cent of lesions that cause RAS, with its prevalence increasing with advancing age. Atherosclerotic RAS characteristically involves the ostium and proximal one-third of the main renal artery5. FMD is typically seen in young women and involves the midsegment of the main renal artery. The various imaging modalities used for detecting RAS include Duplex ultrasonography, renal vein renin assay, nuclear scintigraphy, computed tomographic angiography (CTA), magnetic resonance angiography (MRA) and digital subtraction angiography (DSA).
Unenhanced MRA (UMRA) is a recent imaging MR technique which can demonstrate renal arteries in patients with impaired renal function. In view of the disadvantages of iodinated contrast as well as gadolinium-based contrast agents in patients with kidney disease, unenhanced renal MRA has gained widespread attention. The most common sequences used in UMRA are phase-contrast angiography and time-of-flight (TOF) angiography. Non-enhanced technique based on steady state-free precision (SSFP) sequences has shown good results in evaluating RAS6789. Arterial spin labelling (ASL)10, partial Fourier fast spin echo11 and phase contrast12 UMRA are other techniques, which have been described.
SSFP pulse sequence provides high-quality images using a short repetition time (TR) and is thus useful in providing images in UMRA of the renal and peripheral arteries. SSFP sequences characterized by an alternating flip angle between neighbouring excitations and an echo time (TE) equal to half of the TR are said to be balanced. Modified balanced-SSFP acquisitions can produce uniform fat-water separation without the use of magnetization preparation or fat saturation. Two images are produced in which fat and water are in-phase and opposed phase, respectively, by adjusting the centre frequency. Water-only images (i.e. fat-suppressed images) are generated by the addition of the in-phase and opposed-phase images. Conversely, fat-only images (i.e. water-suppressed images) are generated by the subtraction of the in-phase and opposed-phase images. The image contrast in the water-only images is based on the T2/T1 ratio, as per balanced-SSFP images. The arteries appear brighter than venous blood and muscle because arterial blood has a higher T2/T1 ratio than either of the other two tissue types.
Phase-contrast angiography works by encoding motion into the MR signal, but it requires longer scanning times. TOF angiography saturates the stationary tissue continuously while unsaturated blood enters the image volume, although it is susceptible to signal loss in areas of decreased or in-plane (to the image slice) blood flow.
The aim of our study was to detect and grade RAS in patients with CKD and RVH using the UMRA technique of Non-contract MRA of ArTery and VEins (NATIVE) 3D True Fast Imaging with Steady State Precession (True FISP) sequence.
Material & Methods
This cross-sectional descriptive study was carried out in the department of Radiology and Imaging Sciences in Sri Ramachandra Medical College, Chennai, India. Thirty five patients with CKD and suspected RVH referred to the department during July 2012-June 2015 were studied. The study population comprised 25 men and 10 women, with a mean age of 49 ±16.67 yr (range: 23-75 yr). Clinical suspicion of RVH was raised in view of one or more of the following features: uncontrolled hypertension, unexplained worsening of renal function in the setting of hypertension, asymmetry in kidney size, recurrent pulmonary oedema, >30 per cent increase in creatinine after starting angiotensin-converting enzyme (ACE) inhibitors or angiotensin receptor blockers, and such patients with renal dysfunction were referred for UMRA. Exclusion criteria were patients who had contraindications to MR imaging (MRI) such as pacemakers and cochlear implants. All 35 patients had impaired renal function. The median follow up period following UMRA was 15 months. Institutional ethics committee approval was obtained, and written informed consent was secured from all patients.
Only, the initial three patients referred for UMRA had previous Duplex sonography done, which were reported as negative for RAS. However, due to the high clinical suspicion of RAS, these patients underwent UMRA (of these three patients, one patient had significant RAS and one patient had less than 70% stenosis). Subsequently, all patients were referred for UMRA without an initial duplex ultrasonography study as the renal arteries were well depicted on UMRA, and it was thought not to subject the patient to two imaging modalities. UMRA imaging was performed using 1.5 T superconductive system (Magnetom Avanto; Siemens, Erlangen, Germany) with an eight-element body matrix coil.
The patient was positioned supine with the feet first. Initial Fat Saturated FIESTA (Fast Imaging Employing Steady-state Acquisition) sequence of the upper abdomen was performed in the coronal and axial planes in the region of the kidneys to localize the imaging volume. Subsequently, free breathing respiratory-gated unenhanced NATIVE 3D TrueFISP sequence was done to visualize the renal arteries. Imaging parameters for the free-breathing respiratory-gated unenhanced 3D True FISP technique included TE=1.8 ms, TR=1314 ms, mean inversion time=1200 ms, and a flip angle of 70°. A slab of 100-110 contiguous fat-suppressed axial slices, each of 1.1 mm thickness, was obtained over the defined imaging volume with field of view=320 mm×75 mm. Average acquisition time for this sequence was 3-5 min. The entire study was completed over a period of 20-25 min.
The source data were analyzed on a post-processing workstation (Magnetic Resonance Satellite Console), and multiplanar MIP reformations were studied for the presence of RAS. Stenosis in DSA was calculated by interventional radiologist.
Seventy six renal arteries including six accessory renal arteries were studied. Percentage of stenosis was calculated using diameter at the level of stenosis and in the normal renal artery distal to the stenosis. Stenosis, if present, was graded as 0-50, 50-70 and >70 per cent. More than 70 per cent stenosis was considered haemodynamically significant, and such patients were referred for DSA followed by revascularization if indicated. The criteria for revascularization therapy, namely renal artery stenting were RAS >70 per cent and a pressure gradient between the pre-stenotic and post-stenotic segment >10 mm Hg. Non-ionic iodinated contrast was used for DSA in all but one patients (in a patient with FMD and single kidney, CO2 angiography was performed). Non-ionic iodinated contrast was preferred as compared to CO2 angiography by our interventional radiologist, because of better image resolution. Patients with <70 per cent stenosis were managed with medical therapy and followed up clinically over the duration of the study by monitoring their blood pressure, renal function test and pulmonary function test. Estimated glomerular filtration rate (GFR) was calculated by CKD-EPI equation using calculator from UpToDate (https://www.uptodate.com/contents/search). The formula used is:
GFR=141×min(Scr/κ,1)α×max(Scr/κ,1)−1.209× 0.993age×1.018 [if female]×1.159 [if black],
where Scr is serum creatinine (mg/dl), κ is 0.7 for females and 0.9 for males, α is −0.329 for females and −0.411 for males, min indicates the minimum of Scr/κ or 1 and max indicates the maximum of Scr/κ or 1.
In patients with RAS due to aortoarteritis, DSA and renal artery stenting were to be performed only during the quiescent phase, as assessed by the erythrocyte sedimentation rate (ESR). An ESR <20 mm/h was taken as the cut-off value for quiescent phase. There was only one patient with aortoarteritis.
Statistical analysis: The collected data were analyzed with IBM SPSS 23.0 version (IBM Corp., Armonk, NY, USA). To describe the data, descriptive statistics, frequency analysis and percentage analysis were used for categorical variables and the mean and standard deviation (S.D) were used for continuous variables. For multivariate analysis, Wilcoxon signed rank test and Mann-Whitney U test were used.
Results
UMRA using NATIVE True FISP sequence was performed in 35 patients with CKD and suspected RVH, which included 25 men (71.4%) and 10 women (28.5%). A total of 76 renal arteries were studied including three right and three left accessory renal arteries. Diagnostic quality images of the main renal arteries were obtained in all patients. The ‘diagnostic quality’ of the UMRA images of the main renal arteries up to their first branching points was subjectively assessed by the radiologist for vessel clarity taking into account signal to noise ratio and image contrast.
All 35 patients had elevated creatinine values ranging from 1.6 to 5.1 mg/dl with a mean of 2.5±0.86 mg/dl. Amongst the 13 patients who had RAS, the mean creatinine value was 3.1±1.0 mg/dl, whereas the patients with normal-appearing main renal arteries on UMRA had a mean creatinine value of 2.1±0.62 mg/dl (range: 1.6-3.1 mg/dl). It was observed that patients with haemodynamically significant RAS had a higher creatinine value, mean of 3.5±1.25 mg/dl (range: 2.5-5.1 mg/dl) in comparison with patients with RAS <70 per cent who had a mean creatinine value of 2.4±0.62 mg/dl (range: 1.5-3.4 mg/dl).
The pre-procedural and post-procedural creatinine values (3.4167±1.259 and 1.650±0.628 mg/dl, respectively) of patients with haemodynamically significant RAS were significantly different (P<0.05). For comparison of creatinine values (3.416±1.259 and 2.680±0.715 mg/dl, respectively) in patients with haemodynamically significant (>70%) and insignificant (<70%) RAS, Mann-Whitney test was used and showed no significant difference.
Normal-appearing 58 main renal arteries (76.3%) were seen in 22 patients (Fig. 1). Eighteen renal arteries (24%) in 13 patients were diagnosed to have stenosis. Of these, five patients had bilateral main RAS and eight had unilateral RAS.
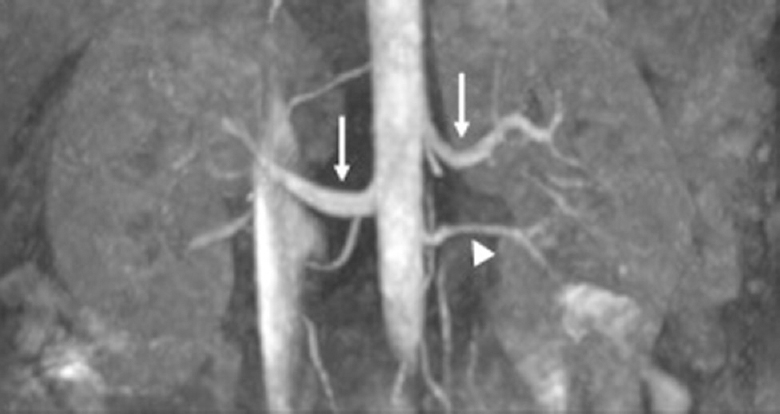
- Non-contrast magnetic resonance angiography of ArTery and VEins 3D True fast imaging with steady-state precession unenhanced magnetic resonance angiography in a 45 yr old hypertensive male with chronic kidney disease showing bilateral normal renal arteries (arrows). Left inferior accessory renal artery (arrowhead).
Of the 18 renal arteries with stenosis, 11 renal arteries (11/18=61%) in eight patients showed haemodynamically significant stenosis i.e. >70 per cent, whereas the stenosis in the remaining seven arteries was deemed haemodynamically insignificant (six renal arteries showed 0-50% stenosis and one showed 50-70% stenosis). Of these, seven patients (with haemodynamically significant stenosis in 10 arteries) underwent DSA. A 24 yr old female patient with significant RAS due to aortoarteritis did not undergo immediate DSA as her ESR was elevated. She was put on steroids (Fig. 2).
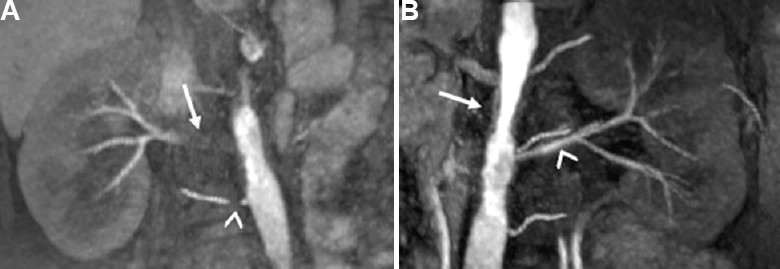
- A 24 yr old hypertensive female patient with chronic kidney disease and aortoarteritis. Non-contrast magnetic resonance angiography of ArTery and VEins 3D True fast imaging with steady-state precession reformatted coronal magnetic resonance angiography images (A) 90-95 per cent stenosis with wall thickening in right main renal artery (arrow) and 80-90 per cent stenosis in right accessory renal artery (arrowhead). (B) Irregularity of aorta with wall thickening (arrow) and normal left renal artery (arrowhead).
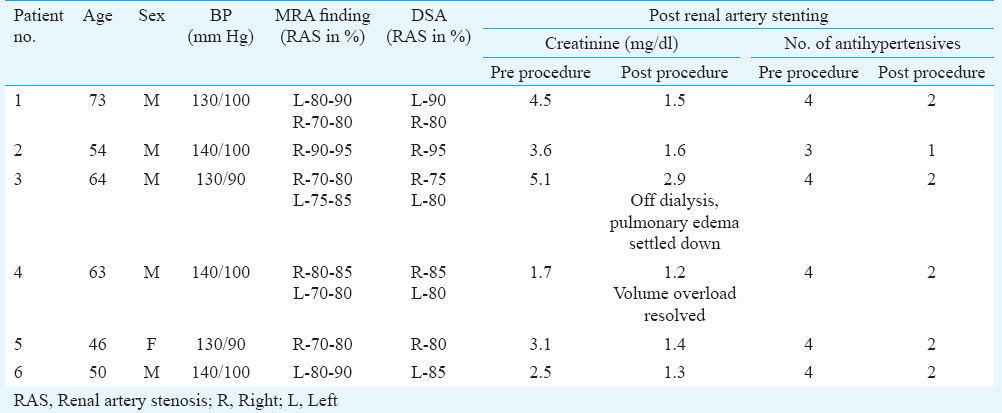
Nine renal arteries (with significant RAS) in six patients, which fulfilled the criteria for revascularization, underwent renal artery stenting (Fig. 3). Unenhanced renal MRA findings were correlated with DSA findings. An association was observed between the presence of RAS and grading of stenosis (Table I). Post-procedure and on follow up, these patients showed improvement in blood pressure as evident by decrease in the requirement of blood pressure medication. Renal function improved in five patients and one patient was off dialysis (Table II).
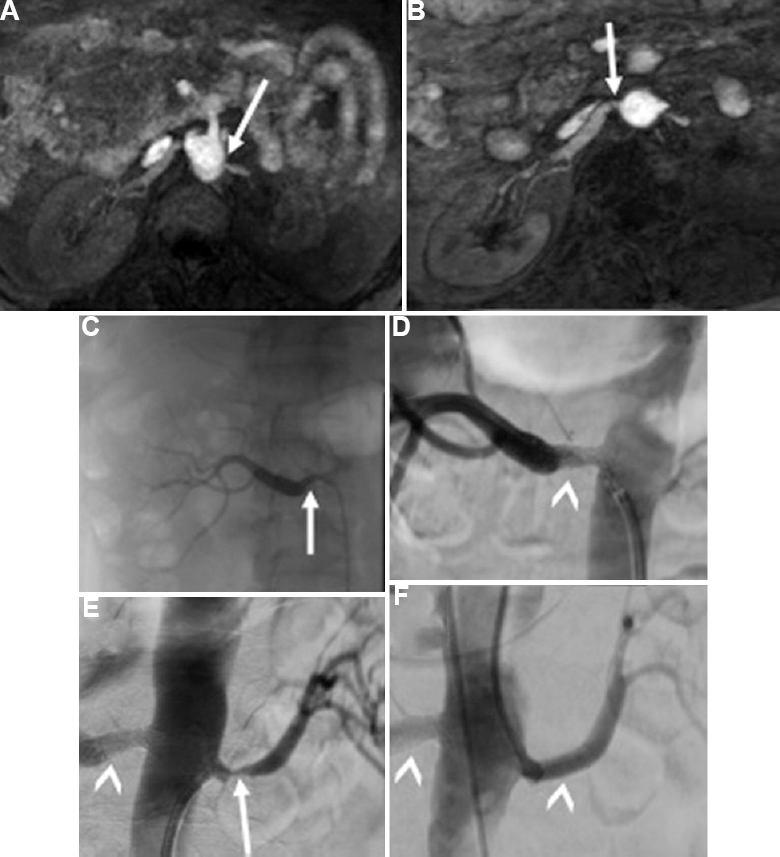
- (A and B) Bilateral severe renal artery stenosis in an elderly hypertensive male with chronic kidney disease detected on unenhanced renal magnetic resonance angiography study, 80-90 per cent stenosis in the left main renal artery and 70-80 per cent stenosis in right main renal artery (arrows). (C-F) Findings confirmed on digital subtraction angiography, 90 per cent - right renal artery stenosis and 80 per cent left renal artery stenosis (arrows), and bilateral renal artery stenting done (arrowheads).
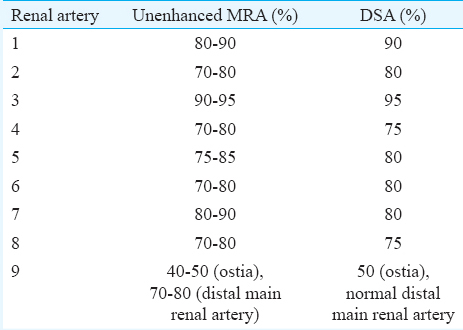
A 23 yr old female patient, a known case of FMD with history of right nephrectomy and left renal artery stenting, presented with CKD and uncontrolled hypertension. UMRA revealed two-short segment narrowing, 50-60 per cent at the ostia and >80 per cent in the distal left main renal artery. It was not possible to distinguish stenosis from signal loss due to stent placement in the distal left main renal artery, and hence, DSA was performed. DSA confirmed the presence and grading of the stenosis at the ostia but revealed the distal main renal artery to be normal (Fig. 4).
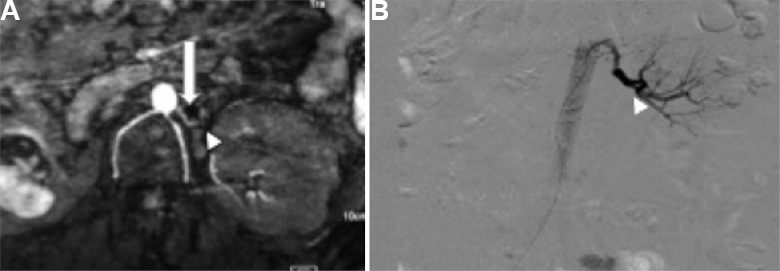
- Unenhanced magnetic resonance angiography (A) of 23 yr old female patient, a known case of fibromuscular dysplasia with history of right nephrectomy and left renal artery stenting revealed 50-60 per cent at the ostia (arrow) and >80 per cent in the distal left main renal artery (arrowhead). (B) Digital subtraction angiography confirmed stenosis at the ostia but revealed normal distal main renal artery to be normal (arrowhead).
Discussion
It is important to identify RAS at the earliest as it is a reversible cause of secondary hypertension. A higher risk of RAS in CKD has been described4. Imaging modalities to detect RAS include Duplex ultrasonography, renal vein renin assay, nuclear scintigraphy, CTA, MRA and DSA.
Duplex ultrasonography has advantages of easy availability, low cost and above all its usefulness in patients with deranged renal function. However, its disadvantages such as operator dependability, variable examination time and low efficacy in detecting pathologies such as FMD and accessory renal arteries have limited its use in detecting RAS13. Captopril scintigraphy helps in assessing renal perfusion and function. However, its decreased sensitivity and specificity in cases of bilateral RAS and impaired renal function have made it less useful in evaluating RAS14. Studies have shown higher rate of false negative and false positive results with renal vein renin assay1516. This along with misleading results obtained due to patient hydration status and sample mishandling has limited the role of renal vein renin assay in RVH. CT renal angiography has high sensitivity and specificity in detecting RAS171819. The potential nephrotoxicity of iodinated contrast medium used in CTA restricts its use in patients with deranged renal function.
Another investigation, which has got high sensitivity and specificity in evaluating RAS, is contrast-enhanced (CE) MRA678. Gadolinium, which is being used in CE MRA, was considered to be safe in patients with deranged renal function and thus it replaced CTA. Later, in 1997, the first case of severe complication, namely nephrogenic systemic fibrosis (NSF), was reported in San Diego, CA, USA20. In 2006, the causal relationship between gadolinium and NSF was established21. NSF was seen to occur exclusively in patients with reduced renal function.
DSA is the gold standard for RAS13, but the threat of contrast-induced nephropathy remains in patients with impaired renal function. Carbon dioxide angiography is considered safe in patients with renal insufficiency. However, it normally does not produce good angiographic images because of its inability to fill the distal vessels and low resolution. Moreover, both are invasive procedures22.
The disadvantages of CE CTA, MRA and DSA led to increasing interest in UMRA techniques for demonstrating RAS. SSFP is a gradient echo-based sequence which has short acquisition time and high signal to noise ratio, but its susceptibility to field heterogeneities and background signals which interfere with detection of vessels is a limitation23. Hence, additional preparatory pulses such as ASL are required to selectively enhance the arteries24. ASL in combination with SSFP is also known as NATIVE True FISP (SIEMENS), Time-SLIP (TOSHIBA), Inhance inflow inversion recovery (GE) or B-TRANCE (PHILIPS)24. The phase-contrast sequence reliably provides angiographic images of segmental renal arteries25.
Wyttenbach et al8 in their study comparing non-enhanced SSFP MRA with CE MRA reported sensitivity, specificity, accuracy, and negative predictive value (NPV) of non-enhanced SSFP MRA for RAS detection as 100, 93, 94 and 100 per cent, respectively, for observer 1 and 95, 95, 95 and 99 per cent, respectively, for observer 2. Mohrs et al26 compared SSFP technique MRA with contrast-enhanced MRA in 45 patients and found sensitivity, specificity, positive predictive value and NPV of 75, 99, 75 and 99 per cent, respectively, for detecting RAS >50 per cent.
In our study, we concentrated on the detection of stenosis in the main renal arteries as the most common cause of RAS i.e. atherosclerosis conventionally involves the ostia and proximal two-thirds of the main renal artery27. The second most common cause, FMD typically involves midsegment of the main renal artery. The basic aim of our study was to broadly categorise patients with main RAS into two; the first category of patients with RAS <70 per cent was managed conservatively with medical therapy, whereas patients in the second category i.e. with haemodynamically significant RAS >70 per cent were subjected to invasive procedure, namely DSA with revascularization, if indicated.
A major limitation of our study was the less number of patients who had RAS (13 of 35), and amongst them, only seven patients who had significant RAS underwent DSA for further confirmation and revascularization if needed. With the data of limited subgroup of patients who underwent DSA for confirmation, there was a concordance with the results of UMRA (Table I). Another limitation was the fact that patients with normal-appearing renal arteries or those with less than 70 per cent stenosis were managed conservatively and did not undergo DSA. This could potentially compromise the specificity and sensitivity of UMRA.
Fujihara et al28 assessed the clinical outcome of renal artery stenting in 108 CKD patients with atherosclerotic RAS. They stated that renal artery stenting helped in stabilization of renal function in patients with CKD. Wolak et al29 studied 32 patients who underwent percutaneous transluminal angioplasty and stent implantation and stated it as an effective procedure in attaining blood pressure control in patients with atherosclerotic RAS and resistant hypertension. In our study, the clinical outcomes showed that renal artery stenting was an effective procedure in controlling blood pressure and maintaining renal function in patients with atherosclerotic RAS (Tables II and III).
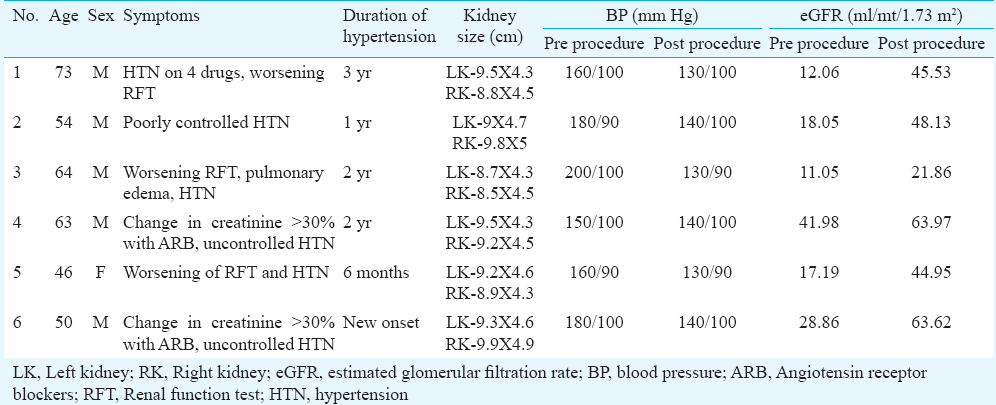
A randomized control trial CORAL (Cardiovascular Outcomes in Renal Atherosclerotic Lesions) stated that the first choice of treatment for patients with RAS and hypertension was medical therapy. However, a major limitation of their study was that they did not evaluate those patients whose diseases were not controlled with medical therapy30. An algorithm was proposed by us for the investigation and management of RAS utilizing UMRA findings (Fig. 5).
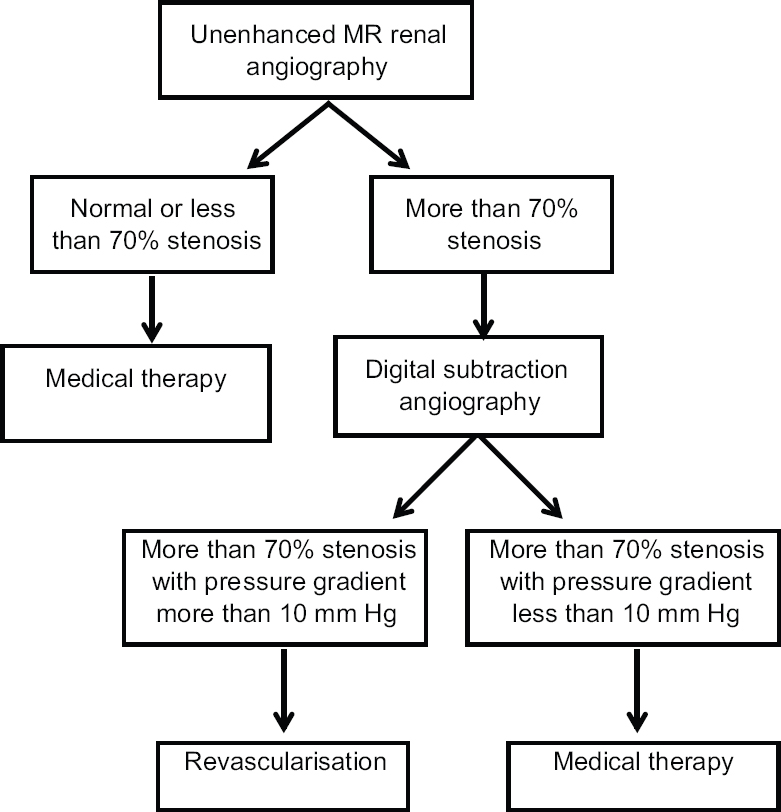
- Management of renal artery stenosis based on unenhanced renal magnetic resonance angiography findings.
In conclusion, unenhanced renal MRA using 3D NATIVE True FISP sequence is a useful non-invasive imaging modality to detect RAS in patients with RVH and impaired renal function. It can help in identifying the subset of patients with haemodynamically significant RAS who need to undergo further invasive procedure and possible intervention namely DSA with revascularization. Normal-appearing renal arteries on UMRA study can effectively exclude stenosis.
Conflicts of Interest: None.
References
- Detection of renovascular hypertension. State of the art: 1992. Ann Intern Med. 1992;117:845-53.
- [Google Scholar]
- Imaging of renovascular hypertension: Respective values of renal scintigraphy, renal Doppler US, and MR angiography. Radiographics. 2000;20:1355-68.
- [Google Scholar]
- Apparent prevalence of curable hypertension in the Hypertension Detection and Follow-up Program. Arch Intern Med. 1985;145:424-7.
- [Google Scholar]
- Atherosclerotic renal artery stenosis – diagnosis and treatment. Mayo Clin Proc. 2011;86:649-57.
- [Google Scholar]
- Free-breathing renal magnetic resonance angiography with steady-state free-precession and slab-selective spin inversion combined with radial k-space sampling and water-selective excitation. Magn Reson Med. 2005;53:1228-33.
- [Google Scholar]
- Renal arteries: Comparison of steady-state free precession MR angiography and contrast-enhanced MR angiography. Radiology. 2006;239:263-8.
- [Google Scholar]
- Renal artery assessment with nonenhanced steady-state free precession versus contrast-enhanced MR angiography. Radiology. 2007;245:186-95.
- [Google Scholar]
- Navigator-gated MR angiography of the renal arteries: A potential screening tool for renal artery stenosis. AJR Am J Roentgenol. 2007;188:W540-6.
- [Google Scholar]
- Renal arteries: Navigator-gated balanced fast field-echo projection MR angiography with aortic spin labeling: Initial experience. Radiology. 2002;225:589-96.
- [Google Scholar]
- Non-contrast-enhanced MR angiography using 3D ECG-synchronized half-Fourier fast spin echo. J Magn Reson Imaging. 2000;12:776-83.
- [Google Scholar]
- Renal artery stenosis: Grading of hemodynamic changes with cine phase-contrast MR blood flow measurements. Radiology. 1997;203:45-53.
- [Google Scholar]
- Renal arterial stenosis: Prospective comparison of color Doppler US and breath-hold, three-dimensional, dynamic, gadolinium-enhanced MR angiography. Radiology. 2000;214:373-80.
- [Google Scholar]
- Gadodiamide-associated nephrogenic systemic fibrosis: Why radiologists should be concerned. AJR Am J Roentgenol. 2007;188:586-92.
- [Google Scholar]
- Renal vein renin studies in renovascular hypertension - Do they really help? J Hypertens. 1985;3:177-81.
- [Google Scholar]
- The value of tests predicting renovascular hypertension in patients with renal artery stenosis treated by angioplasty. Arch Intern Med. 1991;151:1531-5.
- [Google Scholar]
- Radiologic evaluation of suspected renovascular hypertension. Am Fam Physician. 2009;80:273-9.
- [Google Scholar]
- Imaging modalities for renal artery stenosis in suspected renovascular hypertension: Prospective intraindividual comparison of color Doppler US, CT angiography, GD-enhanced MR angiography, and digital substraction angiography. Ren Fail. 2007;29:295-302.
- [Google Scholar]
- A prospective comparison of duplex ultrasonography, captopril renography, MRA, and CTA in assessing renal artery stenosis. Acta Radiol. 2006;47:764-74.
- [Google Scholar]
- Scleromyxoedema-like cutaneous diseases in renal-dialysis patients. Lancet. 2000;356:1000-1.
- [Google Scholar]
- Gadolinium - A specific trigger for the development of nephrogenic fibrosing dermopathy and nephrogenic systemic fibrosis? Nephrol Dial Transplant. 2006;21:1104-8.
- [Google Scholar]
- CO2 digital angiography: A safer contrast agent for renal vascular imaging? Am J Kidney Dis. 1994;24:685-94.
- [Google Scholar]
- Principles and applications of balanced SSFP techniques. Eur Radiol. 2003;13:2409-18.
- [Google Scholar]
- Renal arteries: Isotropic, high-spatial-resolution, unenhanced MR angiography with three-dimensional radial phase contrast. Radiology. 2011;258:254-60.
- [Google Scholar]
- High-resolution 3D unenhanced ECG-gated respiratory-navigated MR angiography of the renal arteries: Comparison with contrast-enhanced MR angiography. AJR Am J Roentgenol. 2010;195:1423-8.
- [Google Scholar]
- Atherosclerotic renal artery stenosis: Ostial or truncal? Radiology. 1996;199:637-40.
- [Google Scholar]
- Clinical outcome of renal artery stenting for hypertension and chronic kidney disease up to 12 months in the J-RAS study – Prospective, single-arm, multicenter clinical study. Circ J. 2015;79:351-9.
- [Google Scholar]
- Does percutaneous transluminal renal artery angioplasty improve blood pressure control and renal function in patients with atherosclerotic renal artery stenosis? Isr Med Assoc J. 2011;13:619-24.
- [Google Scholar]
- Stent revascularization for the prevention of cardiovascular and renal events among patients with renal artery stenosis and systolic hypertension: Rationale and design of the CORAL trial. Am Heart J. 2006;152:59-66.
- [Google Scholar]






