Translate this page into:
Transfusion trigger in the critically ill with sepsis or septic shock: A prospective study
For correspondence: Dr Dalim Kumar Baidya, Department of Anaesthesiology, Pain Medicine & Critical Care, All India Institute of Medical Sciences, New Delhi 110 029, India e-mail: dalimkumar.ab8@gmail.com
-
Received: ,
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Current practice around transfusion trigger in critically ill sepsis patients is not clear. Moreover, any association of haemoglobin trigger and other transfusion parameters such as age of red blood cells (RBCs) at transfusion and number of units of RBCs transfused with mortality and other adverse outcomes need further assessment.
Methods:
In this prospective study, patients aged 18-70 yr and admitted to intensive care with a diagnosis of sepsis were included (n=108). Baseline demographic, clinical and laboratory parameters were noted and various transfusion data, i.e., haemoglobin trigger, number of units of RBCs and the age of RBCs were recorded. Following outcome data were collected: 28 and 90 day mortality, duration of mechanical ventilation, vasopressor therapy, intensive care unit (ICU) and hospital stay and requirement of renal replacement therapy.
Results:
Of the total 108 participants, 78 (72.2%) survived till 28 days and 66 (61.1%) survived till 90 days. Transfusion trigger was 6.9 (6.7-7.1) g/dl [median (interquartile range)]. On multivariable logistic regression analysis, acute physiology and chronic health evaluation (APACHE) II [adjusted odds ratio (aOR) (95% confidence interval {CI}): 0.86 (0.78, 0.96); P=0.005], cumulative fluid balance (CFB) [aOR (95% CI): 0.99 (0.99, 0.99); P=0.005] and admission platelet count [aOR (95% CI): 1.69 (1.01, 2.84); P=0.043] were the predictors of 28 day mortality [model area under the receiver operating characteristics (AUROC) 0.81]. APACHE II [aOR (95% CI): 0.88 (0.81, 0.97); P=0.013], CFB [a OR (95% CI): 0.99977 (0.99962, 0.99993); P=0.044] and transfusion trigger [aOR (95% CI): 3 (1.07, 8.34); P=0.035] were the predictors of 90 day mortality (model AUROC: 0.82).
Interpretation & conclusions:
In sepsis, patients admitted to the ICU, current practice suggests transfusion trigger is below 7 g/dl and it does not affect any adverse outcome including 28 day mortality.
Keywords
Blood transfusion
haemoglobin
ICU
mortality
RBC
sepsis
An infection severe enough to jeopardize the host response and cause new onset organ dysfunction leads to sepsis1. Patients with sepsis or septic shock often need admission to the intensive care unit (ICU). Half of the patients admitted to ICU for a week or more may require transfusion of red blood cell (RBC) and a substantial majority of which may not be necessitated due to any bleeding2-4. RBC transfusion may be associated with immunosuppression, microcirculatory complications, concerns of safety, risk of infection and supply of blood and blood products5,6. While appropriate transfusion trigger is still debated, currently transfusion practices in ICU are slowly moving towards restrictive approach following publication of two large multicentric randomized control trials (RCTs), namely transfusion requirement in critical care (TRICC)7 and transfusion requirement in septic shock (TRISS)8. These trials did not find any significant difference between restrictive (RBC transfusion at haemoglobin <7 g/dl) and liberal transfusion strategy (RBC transfusion at haemoglobin 9-10 g/dl).
The causes of anaemia in ICU are multifactorial and are mostly due to shortened RBC life span, diminished production of RBCs and increased loss of blood. Decreased production may be due to blunted erythropoietin response during critical illness or due to deficiency of iron, folic acid and vitamin B12 and renal failure. Blood loss can be due to trauma, coagulopathy, haemolysis and iatrogenic losses due to diagnostic sampling, vascular cannulation, renal replacement therapy (RRT) and surgical procedures. Observational studies in critically ill patients, showed an average haemoglobin drop of 5.2 g/dl with largest decline observed in the first few days of admission to the ICU9.
Developing countries including India have a higher prevalence of anaemia10. Most of the large RCTs seeking transfusion trigger in critically ill patients have been conducted in developed countries where the baseline haemoglobin may be higher as compared to the developing countries such as India where patients are physiologically well adapted to lower haemoglobin concentration. Therefore, the transfusion trigger used for developed nation may not be generalized in a developing nation. Till now, no study examined the transfusion trigger in critically ill Indian population. Therefore, we planned to conduct a prospective analytical study in critically ill Indian patients with sepsis to identify current practice of transfusion trigger and any association of the haemoglobin trigger and other transfusion parameters (age of RBC units and number of units of transfusion) with mortality and other adverse outcomes.
Material & Methods
Study setting and design: This was a prospective analytical study conducted in the department of Anaesthesiology, Pain Medicine & Critical Care, All India Institute of Medical Sciences (AIIMS), New Delhi, between January 2018 and October 2019. The study was approved by the Institutional Ethics Committee and was registered in the clinical trial registry of India (CTRI/2018/04/013489). The study participants were enrolled from different intensive care units (ICUs) of the hospital. Informed written consent was obtained from patients or their legally acceptable representatives. Patient recruitment was done at the time of the first RBC transfusion and various parameters were noted.
Inclusion and exclusion criteria: Septic critically ill patients (as per sepsis 3 definitions1) of either sex aged 18-70 yr requiring RBC transfusion were included. The exclusion criteria were those with a history of sepsis or ICU stay within the past six months, known case of chronic anaemia requiring repeated blood transfusion, previous history of blood transfusion within two weeks before current admission, on-going bleeding and patients with known ischaemic heart disease (IHD) or ischaemic stroke. IHD was excluded based on suggestive history, electrocardiography and patient on antianginal or anti-platelet drugs.
Sample size calculation: We assumed that approximately 300 patients with sepsis would be admitted to ICU in the proposed study period of 18-20 months. A prior study from India reported a mortality rate of 12.08 per cent in such patients11. Considering a finite population of 300, hypothesized percentage of outcome factor in the population 12.08±5 per cent and 95 per cent confidence interval (CI), 106 individuals were required12.
Study protocol:
Baseline parameters: Diagnosis at the time of admission, source of infection, antibiotic use, baseline demographics, comorbidities, admission APACHE II (acute physiology and chronic health evaluation II) and sequential organ failure assessment (SOFA) scores, haemodynamic parameters, haematological, biochemical and other investigations were recorded.
Study parameters: The haemoglobin at which the decision of RBC transfusion was taken was noted. The total number of RBC units transfused during ICU stay, other blood products transfused and age of the RBC unit was recorded.
Outcome parameters: The outcome parameters such as daily APACHE II, SOFA scores, sedation and Glasgow coma scale (GCS) scores, vasopressor requirement (dose and number of vasopressors), the requirement of mechanical ventilation and renal replacement therapy (RRT), duration of ICU and hospital stay were recorded. Each patient was followed up till discharge or death or 28 days whichever was earlier. An independent outcome assessor, who was not a part of ICU management of the patients, collected all the data from the patients’ file/records and subsequently by telephonic interview till 90 days.
Safety parameters: Any incidence of an allergic reaction, transfusion associated circulatory overload, transfusion related acute lung injury, haemolysis and ischaemic event/thrombotic event was noted.
Statistical analysis: Each recruited participant had a separate case record form for data collection. All the data were tabulated into a Microsoft Excel spreadsheet (Microsoft Office version 2016, Microsoft Corp., WA, USA) and were subjected to statistical analysis by Stata version 13.0 for Mac OS (Stata Corp. TX, USA).
After data compilation was complete, the entire study population was divided into two groups based on 28 day mortality: survivors and non-survivors. The differences in the categorical variables between non-survivors and survivors were estimated by applying Fisher’s exact test or Chi-square test and Mann-Whitney U test was used for continuous variables. Clinical variables with significant association in univariable analysis (P<0.05) were considered for multivariable analysis; the approach helped in limiting the number of independent variables included in the logistic regression model. As this was a relatively small, single-centre study, greater number of variables could have increased the probability of alpha error. Patients’ age was also included in the model as advanced age was found to be associated with poor outcome in critically ill patients. Goodness-of-fit of the multivariable model was assessed by the Hosmer-Lemeshow test.
Results
Of the total 108 participants enrolled, 78 (72.2%; 95% CI: 63.1, 79.8) survived and 30 (27.8%; 95% CI: 20.2, 36.9) died by 28 days of ICU admission. Sixty six participants (61.1%) survived till 90 days.
A total of 65 (60.19%) patients were admitted from the emergency department (ED) and 43 (39.81%) were admitted from the ward. Among the survivors, 47 (60.26%) were admitted from ED and 31 (39.74%) were admitted from ward and among non-survivors, 18 (60%) were admitted from ED and 12 (40%) were admitted from ward (P=0.981). Admission diagnoses of the patients are provided in Figure 1.
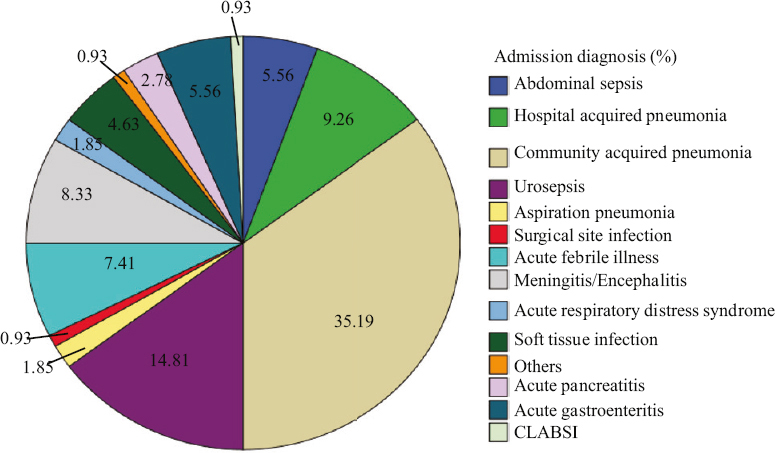
- Distribution of admission diagnosis in recruited patients (%).
Demographic characteristics were comparable between survivors and non-survivors. Non-survivors had significantly higher SOFA and APACHE II scores, lactate, blood urea nitrogen and cumulative fluid balance (CFB) and low GCS score and low platelet count at admission. Non-survivors had increased vasopressor and ventilator days, decreased hospital length of stay (LOS) and similar ICU LOS and RRT requirement compared to survivors (Table I).
| Parameter | All (n=108) | Survivors (n=78) | Non-survivors (n=30) | P |
|---|---|---|---|---|
| Age (yr) | 35 (23-56.5) | 35 (22-57) | 40 (25-54) | 0.7@ |
| Gender (n), male/female | 50/58 | 36/42 | 14/16 | 0.962$ |
| SOFA | 8 (5-10) | 7 (4-9) | 10.5 (8-13) | <0.001@ |
| APACHE II | 15.5 (11.5-24) | 13.5 (10-19) | 22.5 (15-28) | 0.001@ |
| GCS | 13 (10-14) | 13 (11-14) | 11 (8-13) | 0.014@ |
| RASS | 1 (0.2) | 1 (0.2) | 1.5 (−2.2) | 0.553@ |
| CFB (ml) | 2504 (776-5380.5) | 1848.5 (630-4465) | 3783.5 (1780-7456) | 0.001@ |
| TLC (cells/mm3) | 12700 (7900-19000) | 12500 (7900-18200) | 13050 (7900-20200) | 0.918@ |
| Platelets (lakhs/mm3) | 1.65 (0.995-2.555) | 1.8 (1.32-2.6) | 1.11 (0.43-2.05) | 0.009@ |
| Haemoglobin (g/dl) | 9.5 (7.85-11.3) | 9.7 (8.2-11.4) | 8.7 (7.2-10.6) | 0.184@ |
| BUN (mg/dl) | 44 (27-126.5) | 35 (23-91) | 67 (45-159) | 0.0035@ |
| Creatinine (mg/dl) | 1.4 (0.7-3.55) | 1.1 (0.7-3.2) | 2.1 (0.9-5.3) | 0.058@ |
| Lactate (mmol/l) | 1.4 (0.8-2.3) | 1.1 (0.7-2.2) | 2.15 (1.3-2.8) | 0.001@ |
| Admission type (medical/surgical) (n/n) | 87/21 | 61/17 | 26/04 | 0.32$ |
| Antibiotic# | 98 (90.74) | 68 (87.17) | 30 (100) | 0.04$ |
| Admission source (ED/WARD) | 65/43 | 47/31 | 18/12 | 0.981$ |
| Transfusion trigger (g/dl) | 6.9 (6.7-7.1) | 6.9 (6.8-7.1) | 6.9 (6.7-7.1) | 0.62@ |
| Age of RBC (days) | 6 (4.25-9) | 6 (4.5-9) | 5.75 (4-8) | 0.576@ |
| Length of ICU stay (ICU LOS) | 4 (2-6.5) | 4 (3-6) | 3.5 (2-8) | 0.376@ |
| Hospital LOS | 14 (8-21.5) | 16.5 (10-28) | 8 (6-12) | <0.001@ |
| Mechanical ventilation days | 3 (1-6) | 2 (1-5) | 4 (2-8) | 0.013@ |
| Vasopressor days | 2 (0-3) | 1 (0-2) | 3 (2-6) | <0.001@ |
| RRT requirement | 0 (0-0.5) | 0 (0-0) | 0 (0-1) | 0.458@ |
Data presented as median (IQR) or n (%). #Antibiotic received before ICU admission; @Mann-Whitney U test; $Pearson Chi-square test. IQR, interquartile range; CFB, cumulative fluid balance; APACHE, acute physiology and chronic health evaluation score; GCS, Glasgow coma score; ED, emergency department; BUN, blood urea nitrogen; ICU, intensive care unit; SOFA, sequential organ failure assessment, RBC, red blood cell; LOS, length of stay; RRT, renal replacement therapy; TLC, total leucocyte count; RASS, Richmond agitation-sedation scale
The median [interquartile range (IQR)] haemoglobin at admission in all patients was 9.5 g/dl (7.85-11.3) and was comparable between survivors and non-survivors [9.7 g/dl (8.2-11.4) vs. 8.7 g/dl (7.2-10.6); P=0.184]. The median (IQR) haemoglobin at first RBC transfusion (transfusion trigger) in all patients was 6.9 g/dl (6.7-7.1) and was comparable between the groups. The age of RBC transfused in all participants was six (4.5-9) days [median (IQR)] and this was also similar between the groups (Table I).
Primary outcome: A multivariable logistic regression analysis was performed with age, admission APACHE II, GCS, platelet count, creatinine, lactate, CFB and transfusion trigger as independent variables to identify any association with 28 day mortality. It was observed that only APACHE II, platelet count and CFB were significant predictors of 28 day mortality (P=0.47 for goodness of fit for the model; Table II). As a whole this logistic regression model had good discriminatory ability [area under the receiver operating characteristic (AUROC) 0.81; Fig. 2A].
| Parameters | OR | 95% CI | P |
|---|---|---|---|
| Age | 1.009 | 0.98-1.04 | 0.575 |
| APACHE II | 0.863 | 0.78-0.96 | 0.005 |
| GCS | 0.915 | 0.76-1.1 | 0.337 |
| Platelets | 1.699 | 1.01-2.84 | 0.043 |
| Creatinine | 1.087 | 0.93-1.27 | 0.298 |
| Lactate | 0.87 | 0.65-1.16 | 0.35 |
| CFB | 0.99977 | 0.99962-0.99993 | 0.005 |
| Transfusion trigger | 2.229 | 0.83-5.94 | 0.109 |
P<0.05 was considered as significant. OR, odds ratio; CI, confidence interval; CFB, cumulative fluid balance
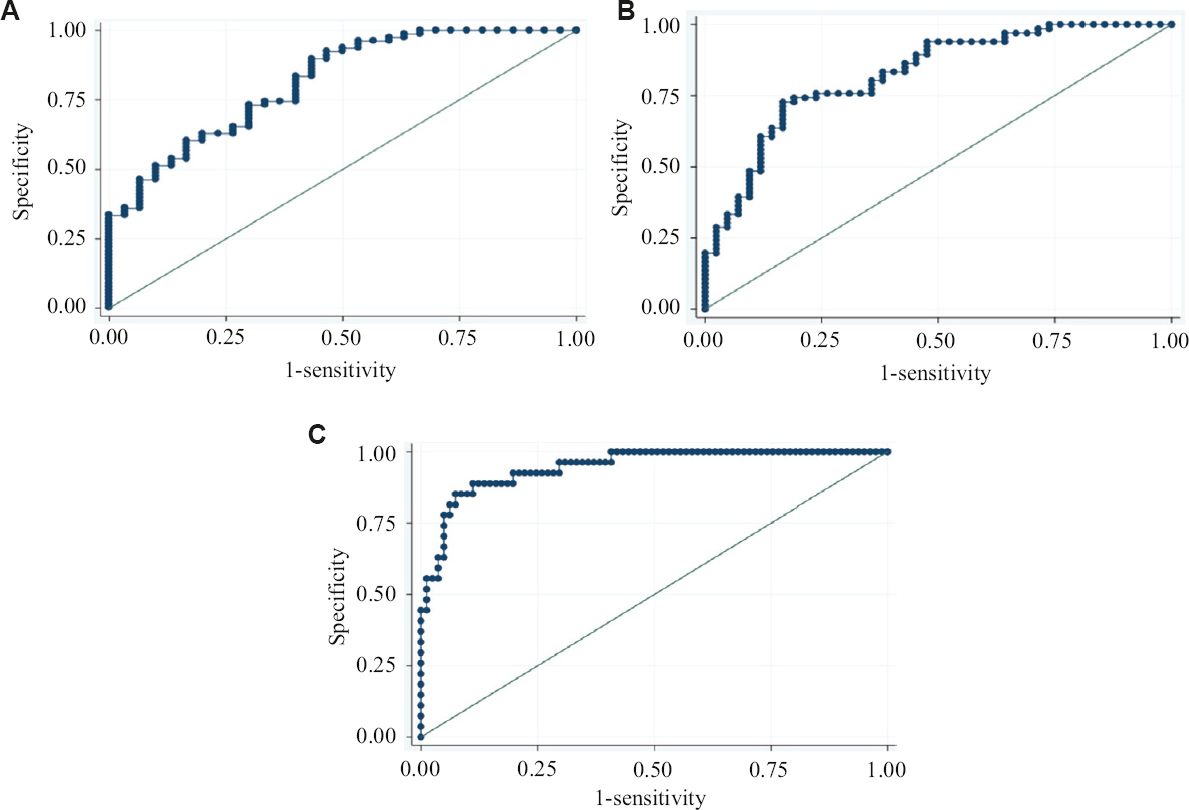
- ROC curve of multivariable analysis model of (A) 28 day survival (B) 90 day survival and (C) RRT. ROC, receiver operating characteristics; RRT, renal replacement therapy
Secondary outcomes: A multivariable logistic regression analysis was performed with age, admission APACHE II, GCS, platelet count, creatinine, lactate, CFB and transfusion trigger as independent variables to identify parameters associated with 90 day survival. APACHE II [adjusted odds ratio (AOR) (95% CI): 0.88 (0.81, 0.97); P=0.013], CFB [0.99 (0.99, 0.99); P=0.044] and transfusion trigger [3 (1.07, 8.34); P=0.035] were found to be significant predictors of 90 day survival (P=0.43 for goodness of fit for the model). As a whole this logistic regression model had good discriminatory ability (AUROC 0.82; Fig. 2B).
A total of 27 participants required RRT and the rest 81 did not. Logistic regression analysis was performed with age, APACHE II, admission creatinine, admission TLC and transfusion trigger as independent variables to identify parameters associated with the requirement of RRT. Only the creatinine level [aOR (95% CI): 1.88 (1.36, 2.6); P<0.0001] at admission was found to be significantly associated with the requirement of RRT (P=0.96 for goodness of fit for the model). No association was found between transfusion trigger and requirement of RRT [aOR (95% CI): 0.58 (0.13, 2.5); P=0.472]. As a whole, this logistic regression model had an excellent discriminatory ability (AUROC 0.94; Fig. 2C).
On linear regression analysis, no association was found between transfusion trigger and length of ICU and hospital stay, duration of mechanical ventilation and vasopressor therapy (Table III).
| Outcome | Correlation coefficient (95% CI) | P | Adjusted R2 |
|---|---|---|---|
| LOS (ICU) | 0.4 (−1.01-1.82) | 0.57 | −0.0064 |
| Days on MV | −0.09 (−1.76-1.58) | 0.92 | −0.0093 |
| Days on vasopressor | 0.32 (−0.62-1.25) | 0.51 | −0.0052 |
| Hospital LOS | 3.78 (−2.26-9.83) | 0.22 | 0.005 |
LOS, length of stay; MV, mechanical ventilation
The total number of RBC units transfused in survivors was 106 and in non-survivors 46. Fifty seven (73.1%) participants who survived at 28 day received one unit of RBC and 21 (26.9%) received two or more RBC units during the ICU stay, whereas 20 (66.67%) participants who died on day 28 received a single unit of RBC and 10 (33.33%) patients received two or more units of RBC transfusion during ICU stay. No association was observed between the number of units of RBC transfused and 28 (P=0.074) or 90 day mortality (P=0.097). The number of patients requiring two or more units of transfusion was similar between survivors and non-survivors at day 28 [21 patients (26.9%) vs. 10 patients (33.3%); P=0.07]. The number of patients requiring two or more units of transfusion was similar between survivors and non-survivors at day 90 [16 patients (24.2%) vs. 15 patients (35.7%); P=0.09].
Of the 27 participants, who required RRT, 13 (48.2%) had two or more units of RBC transfusion. On the other hand, among the 81 participants who did not require RRT, only 18 (22.2%) had two or more units of RBC transfusion (P=0.014).
Only 17 out of 108 participants received other blood products (57 units of random donor platelets and 39 units of fresh frozen plasma), and therefore, no statistical analysis was performed. No transfusion related adverse event was noted in any of the participants.
Discussion
In this prospective study in critically ill patients with sepsis requiring blood transfusion, we observed that 28 day mortality was 27.78 per cent (n=30) and 90 day mortality was 38.89 per cent (n=42). The mean transfusion trigger in all patients was 6.9±0.51 g/dl. Neither the transfusion trigger nor the number of RBC units transfused or age of RBC was associated with mortality and other secondary outcomes. However, transfusion above the transfusion trigger was associated with better 90 day survival.
Mortality has gradually decreased in sepsis patients13. Rivers et al14 reported 33.3% 28 day mortality in 2001, whereas in 2015, Mouncey et al15 in protocolled management in sepsis trial reported 29 per cent 90 day mortality. In the Indian scenario as high as 62 per cent, 28 day mortality was reported in sepsis patients in a study conducted between 2006 and 201116. The estimated mortality rate in the current study is comparable to international literature and reflects global standard of improvement in sepsis care and survival.
Surviving sepsis guidelines17 recommend restrictive transfusion strategy in adult sepsis patients except in patients with acute bleeding or severe hypoxia or myocardial ischaemia, based on available evidence. Hirano et al18 in a systematic review and meta-analysis found no difference in 28 day mortality between liberal and restrictive transfusion strategies. Our findings also confirm that the transfusion trigger does not predict 28 day mortality. A median haemoglobin trigger of 6.9 g/dl suggested that essentially we followed a restrictive transfusion strategy commensurate with the existing guidelines. However, we were intrigued by the fact that better 90 day survival was noted when patients were transfused above the transfusion trigger. This requires further exploration. Various studies have demonstrated that anaemia leads to increased mortality in patients with pneumonia with sepsis8,19. In the current study, pneumonia was the cause of sepsis in as many as 46.3 per cent participants. Rahimi-Levene et al20 found that high neutrophil count and lower transfusion trigger were associated with increased mortality in hospitalized pneumonia patients. In community-acquired pneumonia, Reade et al21 found that anaemia was associated with increased 90 day mortality. On the contrary, in the TRISS trial, 90 day mortality was not different between liberal and restrictive transfusion strategies although more than half of the patients had pneumonia. However, all the patients recruited in TRISS trial were in shock with high severity of illness (median SOFA 10) and faced high mortality (43-45%)8. TRICC trial did not assess 90 day mortality7. While transfusion strategy in sepsis patients with pneumonia can be assessed in large subsequent trials, evidence emerging from RCTs conducted in critically ill cancer patients with sepsis indicates that liberal strategy (trigger haemoglobin 9 g/dl) might be associated with increased 90 day survival19.
In the linear regression model, no association was found between transfusion trigger and various secondary outcomes such as length of ICU and hospital stay, duration of mechanical ventilation and vasopressor therapy. We also did not find any association between transfusion trigger and RRT in the multivariable logistic regression model. Our findings are similar to TRICC7 and TRISS8 trials where the length of ICU or hospital stay, need for vasopressor or mechanical ventilation and requirement of RRT were comparable in patients with restrictive versus liberal transfusion strategy. Bergamin et al19 in oncologic septic shock patients also found no difference in the secondary outcomes such as length of ICU or hospital stay, need for inotropic agents or mechanical ventilation and requirement of RRT. In our study, patients requiring RRT had more frequent transfusions than those not requiring RRT. However, this may be an association rather than causation as the transfusion trigger was not different and failed to predict the requirement of RRT in our cohort. This could reflect the general practice of transfusion during RRT in most patients with anaemia.
A variety of metabolic, biochemical and mechanical changes may occur in RBCs in vitro due to storage (commonly known as storage lesions) and these may reduce oxygen delivery to tissues. Common storage lesion is depletion of cellular 2,3-diphosphoglycerate, which reduces oxygen affinity of haemoglobin, dysfunction of sodium-potassium pump leading to leakage of potassium, and depletion of nitric oxide leading to vasoconstriction, which in turn impair tissue blood flow and oxygenation. Koch et al22 in a retrospective analysis of 6002 postcardiac surgery patients observed that patients who received more than two weeks’ old RBCs were found to have prolonged ventilation, increased sepsis, renal failure and in-hospital mortality. Similarly, Shivhare et al23 observed higher mortality in critically ill patients who received RBCs stored for ≥21 days compared to those receiving RBCs of ≤14 days. However, other important RCTs such as Informing Fresh versus Old Red Cell Management (INFORM) trial24, the age of blood evaluation (ABLE) trial25 and Standard Issue Transfusion vs. Fresher Red Cell Use in Intensive Care (TRANSFUSE)26 trials did not find any difference in mortality between fresh vs. older RBCs. In the current study, we also did not find any association between the age of RBC transfused with 28 or 90 day survival and the requirement of RRT. This was probably because relatively fresh RBCs were used with a median (IQR) age of six (4.25-9) days.
Several studies have demonstrated increased ICU mortality with cumulative positive fluid balance within the first 72 h. Vasopressin and septic shock trial (VASST)27 showed that cumulative positive fluid balance at both 12 and 96 h was associated with 28 day mortality. Neyra et al28 found that higher positive fluid balance at 72 h was associated with hospital mortality irrespective of the presence of acute kidney injury and chronic kidney disease in patients with severe sepsis and septic shock. Similarly, Koonrangsesomboon and Khwannimit29 found increased mortality and prolonged ICU stay with positive fluid balance in a retrospective study from medical ICUs in Thailand. The observations of the current study CFBs independently predicted 28 and 90 day mortality reiterates the same.
Although this was a single centre study, it was conducted in multiple ICUs of the institute under different departments (medicine, pulmonary medicine and anaesthesiology) with independent administrative control, admission pattern, management strategies and discharge criteria. Futhermore, there was no dropout or data loss and all the participants were completely followed up till 90 days. The outcome assessor who noted all the outcome parameters was blinded to the transfusion trigger and the number of units and age of RBC transfused, all contributing to the strengths of this study. However, there were a few limitations. There was no group with higher levels of transfusion; also transfusion was not given as per the underlying pathology and pathogenesis. Individuals with chronic anaemia, IHD, stroke and those who required blood transfusion within two weeks before admission were excluded from the study. Moreover, tissue oxygenation data before and after transfusion were not considered; hence, the results cannot be generalized. As our study was observational in nature with a small sample size, the findings merit critical examination through large randomized controlled trials in future.
Overall, in sepsis patients admitted to ICU, the current practice suggests transfusion trigger is below 7 g/dl and it does not affect any adverse outcome including 28 day mortality.
Financial support and sponsorship
None.
Conflicts of interest
This study was presented at the European Society of Intensive Care Medicine Annual Conference held in October 2022 in Paris and the abstract was published in Intensive Care Med Exp 2022; 10 (Suppl 2) : 000434.
References
- The third international consensus definitions for sepsis and septic shock (sepsis-3) JAMA. 2016;315:801-10.
- [Google Scholar]
- The CRIT study:Anemia and blood transfusion in the critically ill –Current clinical practice in the United States. Crit Care Med. 2004;32:39-52.
- [Google Scholar]
- A multicenter, randomized, controlled clinical trial of transfusion requirements in critical care. Transfusion requirements in critical care investigators, Canadian critical care trials group. N Engl J Med. 1999;340:409-17.
- [Google Scholar]
- Lower versus higher hemoglobin threshold for transfusion in septic shock. N Engl J Med. 2014;371:1381-91.
- [Google Scholar]
- Time course of hemoglobin concentrations in nonbleeding intensive care unit patients. Crit Care Med. 2003;31:406-10.
- [Google Scholar]
- Prevalence and severity of anaemia stratified by age and gender in rural India. Anemia. 2014;2014:176182.
- [Google Scholar]
- Epidemiology of severe sepsis in India:An update. Crit Care. 2010;14((Suppl 1)):P382.
- [Google Scholar]
- Elementary survey sampling (4th ed). Belmont, California: Duxbury Press; 1990.
- Epidemiology of adult-population sepsis in India:A single center 5 year experience. Indian J Crit Care Med. 2017;21:573-7.
- [Google Scholar]
- Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345:1368-77.
- [Google Scholar]
- Trial of early, goal-directed resuscitation for septic shock. N Engl J Med. 2015;372:1301-11.
- [Google Scholar]
- Trends in sepsis mortality over time in randomised sepsis trials:A systematic literature review and meta-analysis of mortality in the control arm, 2002-2016. Crit Care. 2019;23:241.
- [Google Scholar]
- Surviving sepsis campaign:International guidelines for management of sepsis and septic shock:2016. Intensive Care Med. 2017;43:304-77.
- [Google Scholar]
- Liberal versus restrictive red blood cell transfusion strategy in sepsis or septic shock:A systematic review and meta-analysis of randomized trials. Crit Care. 2019;23:262.
- [Google Scholar]
- Liberal versus restrictive transfusion strategy in critically ill oncologic patients:The transfusion requirements in critically ill oncologic patients randomized controlled trial. Crit Care Med. 2017;45:766-73.
- [Google Scholar]
- Lower hemoglobin transfusion trigger is associated with higher mortality in patients hospitalized with pneumonia. Medicine (Baltimore). 2018;97:e0192.
- [Google Scholar]
- The prevalence of anemia and its association with 90-day mortality in hospitalized community-acquired pneumonia. BMC Pulm Med. 2010;10:15.
- [Google Scholar]
- Duration of red-cell storage and complications after cardiac surgery. N Engl J Med. 2008;358:1229-39.
- [Google Scholar]
- Impact of stored red cells on clinical outcome in critically ill. Asian J Transfus Sci. 2019;13:17-22.
- [Google Scholar]
- Effect of short-term versus. Long-term blood storage on mortality after transfusion. N Engl J Med. 2016;375:1937-45.
- [Google Scholar]
- Age of red cells for transfusion and outcomes in critically ill adults. N Engl J Med. 2017;377:1858-67.
- [Google Scholar]
- Vasopressin versus norepinephrine infusion in patients with septic shock. N Engl J Med. 2008;358:877-87.
- [Google Scholar]
- Cumulative fluid balance and mortality in septic patients with or without acute kidney injury and chronic kidney disease. Crit Care Med. 2016;44:1891-900.
- [Google Scholar]
- Impact of positive fluid balance on mortality and length of stay in septic shock patients. Indian J Crit Care Med. 2015;19:708-13.
- [Google Scholar]






