Translate this page into:
The effect of warm liver ischaemia & reperfusion injury on circulating plasma lipid levels & lipolytic enzyme activity in rat & the impact of ischaemic preconditioning
Reprint requests: Dr Sophocles Lanitis, 14 Proairesiou st., Athens, 116 36, Greece e-mail: drlanitis@yahoo.com
-
Received: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Ischaemia/reperfusion (I/R) associated with major liver surgery compromises liver function. Ischaemic preconditioning (IPC) may be effective in minimizing hepatic I/R injury. This study aimed to investigate the impact of liver ischaemic manipulations on lipid metabolism in rat during the process of liver recovery after liver surgery.
Methods:
Sixty three male Wistar rats were assigned to three groups: the sham group, the I/R group which underwent warm ischaemia and reperfusion (I/R), and the IPC group. The animals were subdivided in 3 groups [1st, 3rdand 7th postoperative day (PO)]. Hepatic lipase (HL) and total lipase (TL) activity and the levels of aspartate and alanine transaminases (AST, ALT), triglycerides, HDL and cholesterol were measured in plasma.
Results:
There was no significant difference in the activity of HL and TL between the groups. Significant higher levels of HDL (P<0.0001) were observed in the IPC group when compared to the other groups on the 3rd PO day. Triglycerides (P<0.0001) and HDL (P=0.003) in the IPC group were higher than the sham group on the 7th PO day while HDL was also higher in the I/R group. Significantly higher cholesterol levels were found in the I/R and IPC groups on the 7th PO day, which were not observed in the sham group. There was a similar curve for triglycerides in the sham and IPC groups while there were significantly higher levels of triglycerides on day 7 for the I/R group. The levels of HDL in the IPC group were higher on the 3rd and 7th PO day, compared to day 1.
Interpretation & conclusion:
Warm ischaemia and I/R injury do not seem to affect lipolytic enzyme activity after the 1st PO day despite the effects on plasma lipids. IPC seems to prevent accumulation of triglycerides and cholesterol in plasma.
Keywords
Hepatic lipase
lipid metabolism
preconditioning
rat liver
warm ischaemia
During major hepatic surgery an episode of ischaemia/reperfusion (I/R) occurs frequently, leading to hepatocellular injury and compromised liver function12. This adversely affects post-operative recovery and overall outcome, leading to increased morbidity and mortality13–6. Ischaemic preconditioning (IPC) refers to the process during which a short period of ischaemia and reperfusion of an organ precedes a more sustained period of ischaemia aiming to prepare the organ and increase its tolerance to the anticipated ischaemic conditions and reperfusion injury127. The protective effects of IPC involve various mechanisms and have been considered effective in minimizing hepatic I/R injury8–11.
Since the significance of the involvement of lipids in ischaemic liver trauma and the impact of warm ischaemia on lipid metabolism are not adequately assessed, a study focusing on these could provide additional insight into the mechanisms that regulate hepatic recovery from ischaemic trauma. Moreover, the effect of IPC on plasma lipid levels needs to be addressed to identify possible associations which may eventually prove that lipids have a role in the protective effect of IPC. A proven association may lead to the development of novel strategies based on modulation of hepatic adipogenesis. This experimental study on Wistar rat was conducted to provide important information about the impact of liver ischaemic manipulations (I/R, IPC) on plasma lipid levels and on lipolytic enzyme activity during the process of liver recovery from these manipulations.
Material & Methods
The study was carried out in the experimental laboratory of the 2nd surgical department of the University of Athens in the Aretaieion Athens University Hospital and was approved by the ethical committee of Aretaieion Athens University Hospital, Greece. The study was performed in concordance with the European Union regulations for experimental animals. The animals received humane care in compliance with guidelines of National Institutes of Health (NIH)12.
In the study, 63 male Wistar rats (230-360 g body wt) from one colony (Institute Pasteur Hellenique) were used to exclude sex as a confounding factor. They were fed on a standard chow diet (65% carbohydrate, 18% protein, 3% fat, 5% fiber, 5% minerals and vitamins) and maintained in a 12 h light/12 h dark cycle with free access to food and water until 12 h before the operation. Body weight and the amount of food intake were determined for each animal at the beginning of the study and just before killing them. To minimize daytime variations of hepatic lipase (HL) and total lipase (TL) activity, all operations were performed between 08:00 and 10:00 h. For the induction of anaesthesia, 40 mg/kg ketamine (Ketalar 10 mg/ml) along with 1 mg/kg of atropine (atropine sulphate 1 mg/ml) were injected intramascularly. Midazolam at a dose of 5 mg/kg (Dormicum 15 mg/3 ml) diluted in 0.4 ml of sodium chloride (0.9%) was also injected on a different side to maintain long lasting anaesthesia.
A midline abdominal incision was used to expose all liver lobes. In the sham-operated rats (sham, n=21), laparotomy, exposure and extensive manipulation of the liver for the same amount of time was performed without further interventions.
The 2nd group (I/R, n=21), underwent acute warm ischaemia of the liver for 30 min using a Pringle manoeuvre (i.e. clamping of the hepatoduodenal ligament). The 3rd group (IPC, n=21) underwent ischaemic preconditioning before a prolonged period of warm ischaemia. In this group, a single 5 min clamping of the porta hepatis with a 10 min reperfusion period preceded the 30 min clamping of the porta hepatis. We focused on the 30 min period of ischaemia since this is the most common time used in liver surgery. At the end of the procedure, 15 ml/kg of warm sodium chloride (0.9%) were inserted into the abdominal cavity to replenish fluid losses and prevent dehydration until complete recovery. After wound closure, the animals were kept in special boxes with free access to food and water under standard conditions of controlled temperature, humidity, and light exposure. The animals were re-operated on with the same anaesthetic procedure on post operative (PO) day 1 (Subgroup A), PO day 3 (Subgroup B) and PO day 7 (Subgroup C) when they were killed by acute exsanguination collect blood and liver specimens.
The outcomes of interest were the hepatic lipase (HL) and total lipase (TL) activity and the levels of aspartate and alanine transaminases (AST, ALT), triglycerides, HDL and cholesterol in plasma. For the quantitative analysis of the activity of lipases (TL, and HL) the CONFLUOLIP™ Continuous Fluorometric Lipase Test (Progen Biotechnik GmbH) was used following the four basic steps described by the manufacturer. Fluorescence intensity was measured with a LS-50B fluorometer (Perkin-Elmer, Shelton, CT, USA) at 342 nm excitation and 400 nm emission wavelength. The activity of the lipase in the assay was calculated as the ratio delta fluorescence/time. Distinct assay conditions (pH, NaCl and Triton X100 concentration) allow the selective determination of hepatic lipase with the PR 2004 kit (Buffer B: high ionic strength and pH 8.8) and total lipase with the PR 2003 kit (Buffer A: physiological salt concentration conditions and pH 8.2). Lipoprotein lipase (LPL) activity is almost completely inhibited under the conditions produced by buffer B.
Using the classical automatic methods for quantification of biochemical parameters in plasma in a recently calibrated biochemical analyzer (Hitachi 902 Automatic analyzer, Roche Diagnostics IN, USA) the following parameters were measured: HDL (mg/dl), triglycerides (TG mg/dl), alanine aminotransferase (ALT IU/l), aspartate aminotransferase (AST IU/l), and cholesterol (mg/dl).
Transaminases (ALT/AST) are indicators of liver injury since these increase after hepatocyte collapse. As a result of liver insults, the enzymes are released from the hepatocytes13. After major liver surgery, among other causes, liver ischaemia may increase the levels of these enzymes1314. In this study, ALT/AST levels were used as indicators of liver injury.
The histological specimens of the liver were immediately placed in buffered formalin and subsequently embedded in paraffin. Liver sections were stained with hematoxyline and eosine (H&E) using standard techniques. With a light microscope, the sections were seen independently by two pathologists using a semi-quantitative scoring system to assess and document the presence of mitotic activity, the presence of ischaemic changes, the number of mitoses if present, and the morphology of the liver, to correlate the status of the liver with the outcomes.
Statistical analysis: The statistical analysis was carried out using SPSS for Windows version 17 software package (Statistical Package for Social sciences; Inc, Chicago, IL). Since all comparisons involved more than two groups, analysis of variance (ANOVA) was applied to identify significant differences between the means of the outcome values of the groups followed by follow-up tests (post-hoc): the “Tukey's” and “Bonferron” post hoc tests. For categorical variables the Pearson Chi-square test and Fisher's exact test were used to assess differences in the frequencies between the groups. For the demonstration of the curves over time box plots were used where the range, 95% confidence intervals and median were clearly demonstrated at each time point and direct comparisons between the three groups could be made.
Results
A total of 21 animals from each group survived the procedure and completed the experiment on the predetermined post-operative day. To assess the heterogeneity between the experimental animals which were assigned to each subgroup (PO day), the initial weights of the animals were compared and no significant differences were found.
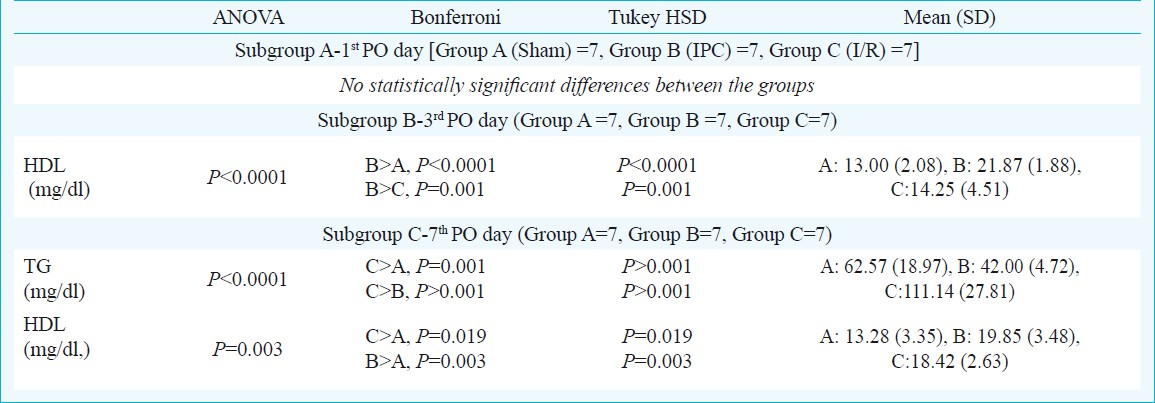
The outcome values of the groups were compared according to the PO day (i.e 1st, 3rd and 7th PO day) (Table I).
On the 1st PO day (subgroup A), two animals from the sham group (28.5%), and four from the I/R group (57%) while none from the IPC group were found to have pathologic findings compatible with liver ischaemia. The changes involved less than 5 per cent of the specimen. In the four affected animals of the I/R group, there were also areas of focal periportal ischaemic necrosis which was not observed in the other two groups. There was no difference in the occurence of ischaemia between the sham and I/R and between the sham and IPC while the difference was significant between the I/R and IPC groups (P<0.05).
The levels of AST and ALT, reflecting the hepatocyte injury or stress, were lower in the sham than in the other groups, but the difference was not significant at this time point (Fig.).
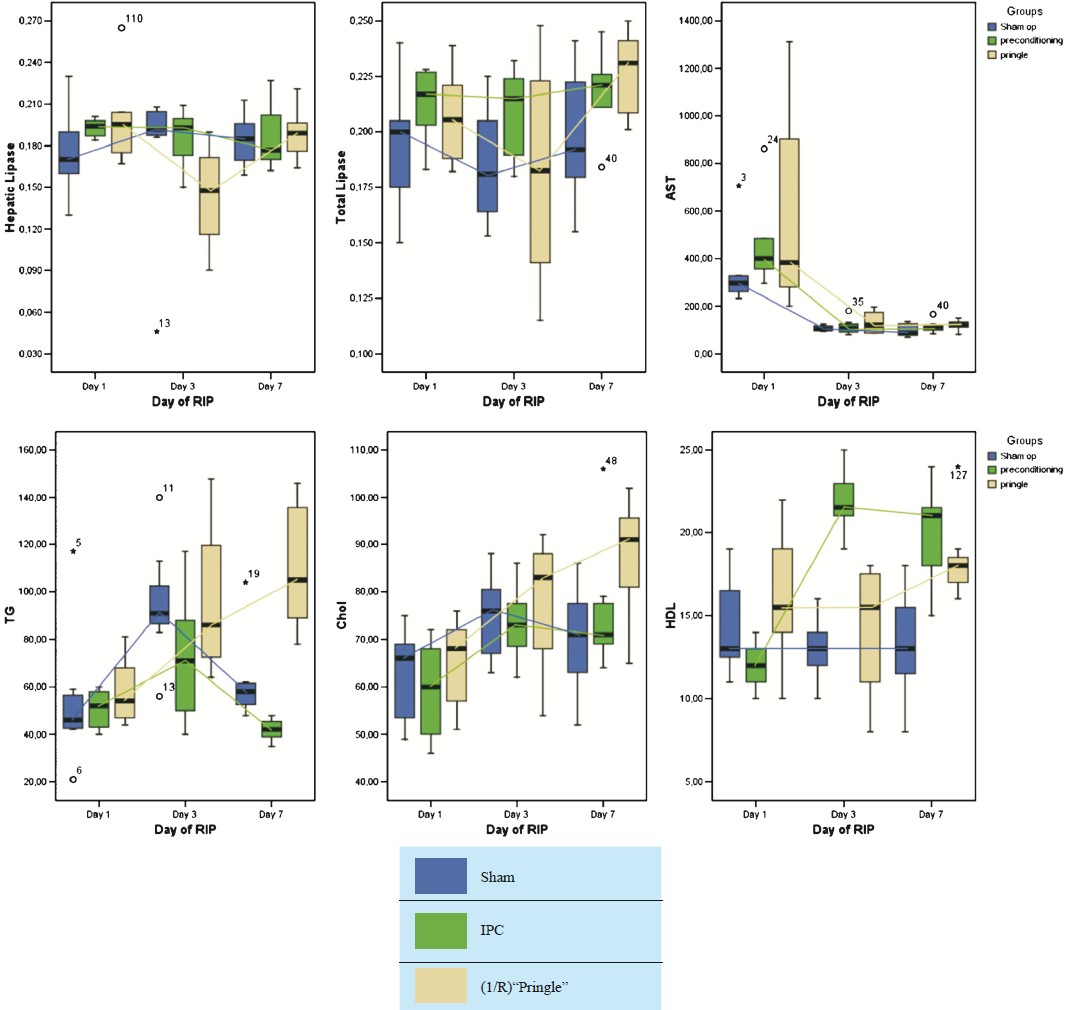
- Box plots for the two groups for the main outcomes (hepatic lipase, total lipase, AST, triglycerides, cholesterol and HDL). The box for each time point and for each group along with the resulting curve is displayed. Day of RIP = The day the animals died and the experiment was terminated.
On the 1st PO day, there was no significant difference in the activity of TL and HL between the three groups. The same was true of the plasma levels of TG, HDL and cholesterol.
On the 3rd PO day (subgroup B), two sham animals (28.5%), two from the I/R group (28.5%) and one from the IPC group (14%) had pathologic findings compatible with liver ischaemia. The changes affected less than 5 per cent of the specimen. None of these differences were found to be significant.
A significant drop in the enzymes, especially AST (P<0.001), was observed at this time point for all 3 groups (Fig.). The levels of both enzymes were similar between the groups. The activity of TL and HL was similar between the groups as were the plasma levels of TG and cholesterol. On the other hand, higher plasma levels of HDL were observed in the IPC group when compared with the sham group (P<0.001) and with the I/R group (P=0.001) while no significant difference was observed between the sham and the I/R group (Fig.).
On the 7th PO day (subgroup C), none of the animals had signs of ischaemia. The levels of AST and ALT were similar between the groups. The activities of TL and HL were not different between the groups as were the plasma levels of cholesterol. Significantly higher levels of TG were observed in the I/R group when compared with the sham (P=0.001) and the IPC group (P<0.001). In the I/R and IPC groups, the plasma levels of HDL were significantly higher than those of the sham group (P=0.019 and P=0.003, respectively) (Fig.).
The outcomes of the 1st, 3rd and 7th PO days were further compared for each group thus having 3 more comparisons (Table II).
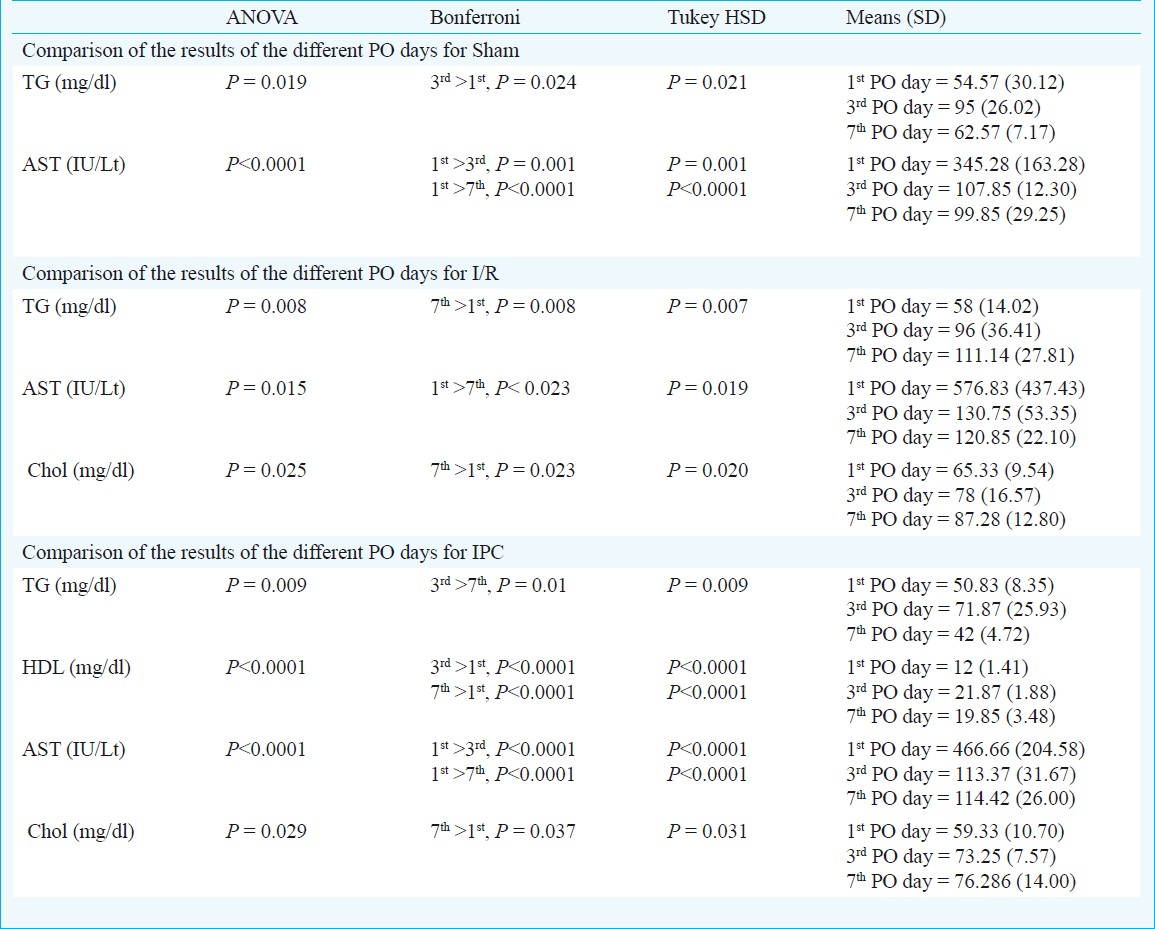
Sham group had no significant fluctuation in the activity levels of TL, HL and plasma levels of ALT, HDL and cholesterol. Significant higher levels of TG (P= 0.024) were observed on the 3rd PO day compared to the other two days creating a peak at this time point.
No significant fluctuations of the activity levels of TL, and plasma levels of ALT and HDL were observed in I/R group. HL activity decreased significantly the 3rd PO day but partly recovered by day 7 (P=0.035). Moreover, cholesterol and TG levels progressively increased from day 1, to reach significant higher levels by day 7 (P= 0.023 and P= 0.008, respectively).
In, IPC group, the activity of TL and HL did not fluctuate over time. There was a peak of the levels of TG on day 3 before a significant decline by day 7 (P= 0.01). HDL levels increased on the 3rd PO day at significantly higher levels than day1 (P<0.0001) and remained high until day 7 (P<0.0001). From PO days 1 to 7, cholesterol increased progressively reach at significantly high levels on day 7 (P= 0.037) compared to days 1 and 3.
Discussion
The severity and extent of cellular damage during liver ischaemia depends on the duration and type of ischaemia as well as the pre-existing condition of the liver. Short periods (60 min) of warm ischaemia are associated with reversible cell damage while extended periods (120-180 min) lead to permanent cellular death15. It has been shown in studies with longer animals, warm liver ischaemia (37°C) mostly affects liver parenchymal cells15–17. On the other hand, cold ischaemia (4°C) affects more the sinusoidal endothelial cells (SECs)151819.
Reperfusion injury refers to the phenomenon where the restoration of oxygen supply to an ischaemic organ accentuates the cellular damage caused by the primary insult15. During liver resection there may be a need for temporary (intermittent or continuous) vascular occlusion to the liver in order to minimize blood loss which inevitably leads to reperfusion. During transplantation, following a period of cold ischaemia, the organ is also subjected to a smaller period of warm ischaemia and reperfusion injury2. In cases of I/R injury, the mechanism of cell death involves both apoptosis20 and necrosis, a term recently called “necrapop-tosis”615,21.
It has been shown that during I/R, sinusoidal cells die only via apoptosis while hepatocytes may die in both ways (necrosis and apoptosis). In sinusoidal cells, apoptosis occurs earlier and at a higher level than in hepatocytes but the differences in the extent of the apoptosis between these cells tend to ameliorate after prolonged reperfusion period6.
The protective effects of IPC have been shown in various studies2. The reduction of the I/R injury has been associated with the decreased serum aminotransferase levels22, a finding which has also been confirmed in human models especially in younger population23. Studies have shown that IPC protects the liver by inhibiting SEC apoptosis11.
A good model of I/R injury and IPC involves a single 5-10 min period of IPC before a 40 min ischaemic event since a more extended period of warm ischaemia (60 min) is associated with severe I/R injury in rats622. Moreover, it has been shown that 5 min of ischaemia followed by 10 min of reperfusion protects the liver even after 90 min of ischaemia24. In all these studies a selective occlusion (partial liver ischaemia) was used as opposed to our study.
In this experiment a small number of mitoses was found only in the I/R group while there were variable rates of ischaemic changes over time. The ischaemic areas were characterized by a decrease in the hepatocellular continuity, cytoplasmic homogenization, hepatocellular shrinkage, nuclear instability and ill-defined nuclei. During the 1st PO day ischaemic changes were observed in a significantly higher percentage of the sham and I/R than the IPC group animals. The manipulations on the liver, the operative stress as well as the anaesthesia may have contributed, to a degree, in explaining the findings in sham animals. In I/R group, warm ischaemia clearly led to focal periportal ischaemic necrosis, a finding observed only in this group. These results indicated that the liver was well protected from both surgical stress and ischaemia in the IPC group during the first 24 post-operative hours. Despite the fact that on the 3rd PO day some ischaemic changes were also observed in the sham and I/R groups and none in the IPC group, the differences were not significant.
TG and cholesterol had similar curves over time for the sham and IPC groups, characterized by a peak on day 3 and a drop by day 7. In the I/R group there was a progressive rise in the levels of both lipids over time. Eventually, on day 7 significantly higher levels of TG and cholestrol were observed in the I/R group when compared to other groups. This indicated that the recovery duration was longer in the I/R group or that the binding capacity of the liver for lipids was adversely affected by ischaemia, hence impairing lipid clearance. A similar pattern was observed between the sham and IPC groups, indicating that IPC may affect the lipid metabolism no more than sham operation does. The fact that IPC protects better steatotic livers may be related to this finding.
Hepatic lipase (HL) can be found in the liver of most mammals, where it plays a central role in lipoprotein metabolism25. The hydrolytic action of HL allows free cholesterol from HDL surface to be delivered to hepatic cells, where it is converted into biliary salts25. Lack of HL leads to high plasma levels of LDL, HDL, VLDL, triacylglycerole and chylomicrons since their clearance is impaired25.
In the sham and IPC groups, both TL and HL were unaffected by the manipulations while in the I/R group the levels of the 2 enzymes decreased on day 3 (though not significantly) before these recovered by day 7. This may explain the higher levels of circulating lipids on day 7.
In the I/R group, HDL increased significantly by day 3 and the high levels were maintained until day 7 as opposed to the other groups where the HDL levels remained low and did not significantly alter over time. This pattern of HDL plasma levels over time in the IPC group may be involved in the protective mechanism of IPC, since the main function of HDL is to carry circulating lipids to the liver for excretion or re-utilization, and to other organs for steroidognesis. Moreover, HDL has been shown to inhibit oxidation, inflammation, activation of the endothelium, coagulation, and platelet aggregation26.
In summary, warm ischaemia and I/R injury did not seem to affect lipolytic enzyme activity after the 1st PO day despite the effects on plasma lipids. IPC seems to prevent accumulation of triglycerides and cholesterol in plasma while it causes increased levels of HDL. Considering this, the protective effects of IPC may partly be attributed to the modification of lipid metabolism. Further studies on humans and experimental studies targeting on the underlying mechanism are necessary to confirm these associations.
References
- Ischemic preconditioning impairs liver regeneration in extended reduced-size livers. Ann Surg. 2005;241:477-84.
- [Google Scholar]
- Ischaemic preconditioning in transplantation and major resection of the liver. Br J Surg. 2005;92:528-38.
- [Google Scholar]
- Continuous versus intermittent portal triad clamping for liver resection: a controlled study. Ann Surg. 1999;229:369-75.
- [Google Scholar]
- Hepatic resection with ischemia of the liver exceeding one hour. J Am Coll Surg. 1994;178:454-8.
- [Google Scholar]
- Reperfusion injury to donor livers stored for transplantation. Liver Transpl Surg. 1995;1:124-38.
- [Google Scholar]
- Endothelial cell and hepatocyte deaths occur by apoptosis after ischemia-reperfusion injury in the rat liver. Transplantation. 1999;67:1099-105.
- [Google Scholar]
- Preconditioning with ischemia: a delay of lethal cell injury in ischemic myocardium. Circulation. 1986;74:1124-36.
- [Google Scholar]
- Effects of ischemic preconditioning on regenerative capacity of hepatocyte in the ischemically damaged rat livers. J Surg Res. 2005;125:42-8.
- [Google Scholar]
- Effects of ischemic preconditioning on cyclinD1 expression during early ischemic reperfusion in rats. World J Gastroenterol. 2006;12:2936-40.
- [Google Scholar]
- Ischemic preconditioning attenuates the oxidant-dependent mechanisms of reperfusion cell damage and death in rat liver. Liver Transpl. 2002;8:990-9.
- [Google Scholar]
- Ischemic preconditioning attenuates morphological and biochemical changes in hepatic ischemia/reperfusion in rats. Pathobiology. 2010;77:136-46.
- [Google Scholar]
- NAS. In: Guide for the care and use of laboratory animals. Washington, DC: National Academic Press; 1996.
- [Google Scholar]
- Serum lipid and lipoprotein alterations represent recovery of liver function after hepatectomy. Liver Int. 2006;26:203-10.
- [Google Scholar]
- Comparison of liver function tests after hepatic lobectomy and hepatic wedge resection. Am Surg. 1998;64:408-14.
- [Google Scholar]
- Ischemic injury in liver transplantation: difference in injury sites between warm and cold ischemia in rats. Hepatology. 1992;16:454-61.
- [Google Scholar]
- Warm liver ischemia in experiment and lysosomal markers. Bratisl Lek Listy. 2009;110:587-91.
- [Google Scholar]
- Sinusoidal lining cell damage: the critical injury in cold preservation of liver allografts in the rat. Transplantation. 1988;46:178-91.
- [Google Scholar]
- Reperfusion injury to endothelial cells following cold ischemic storage of rat livers. Hepatology. 1989;10:292-9.
- [Google Scholar]
- Activation of apoptosis during the reperfusion phase after rat liver ischemia. Transplant Proc. 1996;28:1908-9.
- [Google Scholar]
- Apoptosis versus oncotic necrosis in hepatic ischemia/reperfusion injury. Gastroenterology. 2003;125:1246-57.
- [Google Scholar]
- Amelioration of liver injury by ischaemic preconditioning. Br J Surg. 1998;85:1636-40.
- [Google Scholar]
- Protective effects of ischemic preconditioning for liver resection performed under inflow occlusion in humans. Ann Surg. 2000;232:155-62.
- [Google Scholar]
- Preconditioning: effect upon lesion modulation in warm liver ischemia. Transplant Proc. 1993;25:3303-4.
- [Google Scholar]
- Hepatic lipase is localized at the parenchymal cell microvilli in rat liver. Biochem J. 1997;321:425-30.
- [Google Scholar]
- The metabolic pathways of high-density lipoprotein, low-density lipoprotein, and triglycerides: a current review. Am J Cardiol. 2000;86:5L-10L.
- [Google Scholar]






