Translate this page into:
Spotted fever rickettsiosis in Uttar Pradesh
*For correspondence: drmastansingh@rediffmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
Rickettsiosis consists of a spectrum of vector borne diseases caused by small Gram-negative obligate intracellular bacteria which includes epidemic typhus, scrub typhus and spotted fever. Rickettsial diseases have been reported from various parts of India namely Jammu and Kashmir, Uttarakhand, Maharashtra, Kerala, Tamil Nadu, Assam and West Bengal123. Cases described here were admitted in Paediatrics ward of King George's Medical University, Lucknow, Uttar Pradesh, India, in November 2013, and referred to the department of Microbiology for investigations. There were four confirmed cases belonging to ‘’spotted fever’’ group which includes tick borne agents Rickettsia rickettsii, R. conorii and mite transmitted R. akari. All were from rural areas within 100 km of Lucknow (district- Hardoi, Raebareli, Sultanpur and Sitapur). Information related to demography, clinical presentation, vital parameters and routine haemogram done at the time of admission, is given in Table I. Inoculation eschar was not noted in any of the patients. None reported pallor, cyanosis or icterus, and central nervous system examination was within normal limits. The institutional ethics committee approved the study.
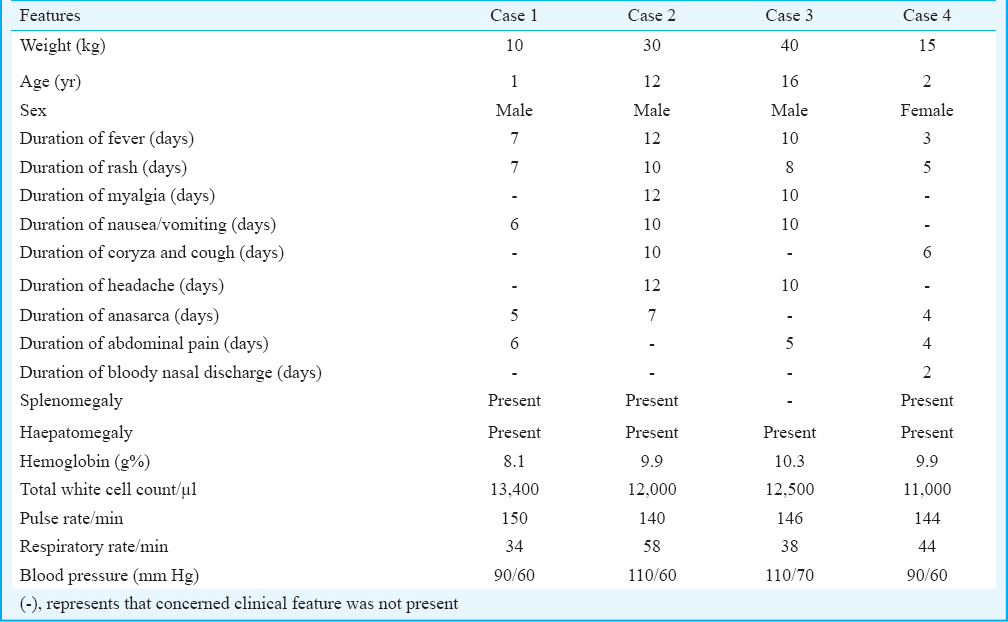
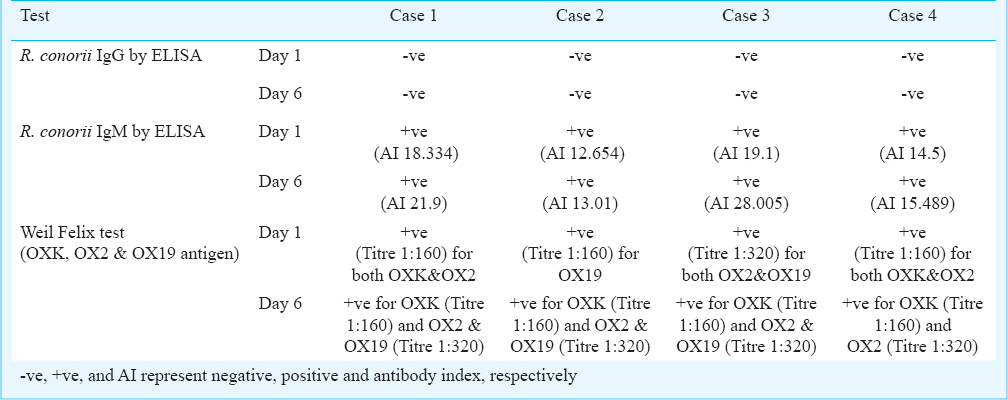
Serology for typhoid (Typhidot, AB Diagnopath Manufacturing Pvt. Ltd, New Delhi, India; Widal; in-house), malaria (antigen detection, Optimal, Bio-Rad Laboratories India Pvt. Ltd., Gurgaon, Haryana, India) and dengue (NS1 antigen, Microlisa, J. Mitra & Co. Pvt. Ltd., New Delhi, India) was negative and blood cultures were sterile even after seven days of aerobic incubation. Blood (4 ml) was drawn from each patient on days one and six of admission and serum was separated. Serum samples were tested for R. conorii IgG and IgM by ELISA (Vircell Microbiologists, Spain); antibody index (AI) was calculated as per the manufacturer's instructions. Further, serum samples were also tested for Weil Felix test (Tulip Diagnostics, Goa, India). All serological tests for rickettsiosis were done in paired samples (i.e. on days 1 and 6 of admission); results are presented in Table II.
All patients were empirically treated with injection ceftriaxone and amikacin. Once serology reports were available on day two, patients were also given oral doxycycline 5 mg/kg/day in two divided doses for 5-7 days. There was rapid improvement in patient's condition and all became afebrile within 24-48 h and were discharged within next 7-9 days.
The disease spectrum of rickettsiosis is wide. In most patients it is mild; however, serious complications and fatalities have also been reported45. Establishing the aetiological diagnosis is difficult during the acute stage of illness and the clinical features may be confused with atypical measles, dengue, malaria, sepsis, meningococcaemia, leptospirosis and vasculitis syndromes. These were ruled out clinically and by investigations in our patients. Definitive diagnosis usually requires heightened clinical suspicion and examination of paired serum samples for serological evidence6. Many cases of rickettsial infection are believed to go undiagnosed due to lack of diagnostic facilities1245.
Here, we reported four confirmed cases of spotted fever group infection; where clinical suspicion followed by examination of paired serum samples for serological evidence, confirmed the diagnosis and prompt treatment led to recovery in all patients.
Acknowledgment
This work is done as part of an ongoing “Rickettsial Serosurveillance” Project with support from ICMR at the department of Microbiology, KGMU, Lucknow.
References
- Rickettsial diseases in Haryana: not an uncommon entity. J Assoc Physicians India. 2009;57:334-7.
- [Google Scholar]
- Tick-borne rickettsioses around the world: emerging diseases challenging old concepts. Clin Microbiol Rev. 2005;18:719-56.
- [Google Scholar]
- Diagnosis and management of tickborne rickettsial diseases: Rocky Mountain spotted fever, ehrlichioses, and anaplasmosis - United States: a practical guide for physicians and other health-care and public health professionals. MMWR Recomm Rep. 2006;55(RR-4):1-27.
- [Google Scholar]
- Rickettsial diseases. In: Longo DL, Fauci AS, Kasper DL, Hauser SL, Jameson JL, Loscalzo J, eds. Harrison's principles of internal medicine (18th ed). New York: McGraw-Hill; 2012. p. :1407-17.
- [Google Scholar]





