Translate this page into:
Socioeconomic determinants of the quality of life in boys suffering from Duchenne muscular dystrophy & their caregivers
For correspondence: Dr Renu Suthar, Department of Pediatrics, Pediatric Neurology Unit, Postgraduate Institute of Medical Education and Research, Chandigarh 160 012, India e-mail: drrenusuthar@gmail.com
-
Received: ,
Accepted: ,
Abstract
Background & objectives
Duchenne muscular dystrophy (DMD) is the most common childhood-onset muscular dystrophy, severely affecting the quality of life (QoL) of affected children and their caregivers. Socioeconomic status (SES) is directly correlated with QoL of many chronic and life-threatening diseases. This study aimed to understand the socioeconomic determinants of the QoL in boys affected with DMD and their caregivers.
Methods
The present paper analyses the cross-sectional data of a prospective study involving boys aged 5 to 15 yr with DMD and their caregivers. HrQoL of boys was assessed using EQ 5D-3L tool and PedsQL3.0 Neuromuscular Module, and overall global QoL of caregivers was assessed using World Health Organization Quality of Life-BREF (WHOQOL-BREF). SES was assessed using the OP Agrawal scale. EQ-5D utility index, using adult tariffs, was applied to the Indian paediatric population for the first time. The correlation and association between QoL and SES covariates were analysed with Spearman, linear, stratified analysis, and multiple linear regression.
Results
A total of 100 families of boys with DMD were enrolled [median age 9 yr (IQR: 7.0-9.0), 91% ambulatory]. HrQoL scores of children as mean (S.D) EQ 5D utility score and PedsQoL for physical health were 0.58±0.38 and 77.7±17.7, respectively. Both were inversely correlated with advancing age and clinical severity of disease. HrQoL of boys has no significant correlation with their socioeconomic status(r=0.04; P=0.708). The average QoL of caregivers was assessed as moderate to good across four domains of WHOQOL-BREF. The environment and social relationship domain of QoL caregivers was positively correlated to EQ 5D utility scores (r=0.22 P=0.028 and r=0.21 P=0.033). QoL of the caregiver’s environmental health, social relationship, and psychological health were directly correlated with SES on multiple linear regression after adjusting for socio-demographic and clinical predictors. The quality of physical health of caregivers was independent of any factor.
Interpretation & conclusions
Overall QoL of children with DMD and primary caregivers was found to below, and the QoL of children is not affected by SES. HrQoL of boys with DMD was inversely associated with the age/ progression of the disease but not with the socioeconomic status of the families. Lower socioeconomic status is inversely associated with the QoL of caregivers. Hence, QoL in boys can be addressed by accessible and effective therapeutic interventions, while tailored interventions and support programmes like patient-centered care that empower lower socioeconomic status can improve the QoL of caregivers.
Keywords
Caregivers
disease progression
EQ 5D utility score
muscular dystrophy
neuromuscular disorders
quality of life
socio-economic status
Quality of life (QoL) is an important outcome measure for any service or commodity that affects human well-being1. It is not only determined by economic factors but is also a subjective perception of one’s well-being in various domains, such as physical health, mental health, and social functioning. Hence, an objective quantification becomes difficult2,3. However, there are standardised tools that can offer a comparative assessment of QoL4 across different groups of people.
Duchenne and Becker’s muscular dystrophy are X-linked genetic conditions that are chronic, lifelong, with no definite cure, and require supportive therapy5,6. Affected children lose their ability to walk by the age of 10 yr and have a shorter life span. Advances in medical care and recently discovered gene therapy or exon skipping therapy have attenuated the severity of disease and extended life years with disabilities. QoL varies among boys with DMD, with some showing poor QoL and others comparable to healthy boys3,7. DMD is a debilitating illness that not only affects the individual but also has a significant impact on the physical, mental, and social well-being of their families, like other chronic diseases, such as, asthma, chronic kidney disease, type 1 diabetes mellitus, and epilepsy8,9. Caregivers of older boys report lower QoL as impairments and ageing heavily impact them10. Mothers’ perception of their sons’ QoL predicts their own QoL and emotional distress, affecting social activities, which are vital for stress management9. Research highlights the link between disease progression and caregiver burden11. An Egyptian study12 found that DMD imposes heavy economic burdens on families, leading to reduced care quality and QoL of children. Evaluating health-related quality of life (HRQoL) in individuals with rare diseases is crucial for understanding their unique health needs and assessing the impact of disease and treatment with disease progression13. QoL is vital for caregivers, as their well-being impacts their emotional resilience, ability to manage stress, and effectiveness in providing care to a person with a chronic disease14,15.
Low SES significantly impacts caregivers’ QoL in chronic diseases, as studies highlight its association with poor health outcomes, limited access to care, and increased isolation. A German study14 (n=11,177) found that adults with lower education reported more severe issues in HRQoL with chronic diseases. Low SES groups face double burden: increased levels of health impairments and lower levels of estimated HRQoL once health is impaired. Similarly, a Belgian qualitative study16 highlighted that low income, education, unemployment, and single parenthood contribute to poor QoL in parents of children with chronic diseases. In low- and middle-income countries like India, access to adequate health care may be limited. This may be evident through a lack of insurance coverage, inadequate transportation, unaffordable or unavailable medications and treatments, insufficient information or education about the disease and its management, poor communication or trust with healthcare providers, and a lack of continuity or coordination of care. As a result, it becomes difficult for children and caregivers to manage the challenges of living with a chronic disease. Barriers like limited access to care and unaffordable treatments worsen caregivers’ emotional distress. Improving QoL for individuals with rare disease and caregivers is a key goal of any healthcare interventions or multidisciplinary approach, as rare diseases impact the QoL of both affected individuals and caregivers13.
Comprehensive management to alleviate symptoms and slow to the disease progression, and to enhance QoL is crucial for rare diseases lacking specific drug therapies. While SES impacts QoL in many conditions, its role in DMD remains understudied. This cross-sectional sub-analysis of a quasi-experimental study explored the relationship between socioeconomic determinants and QoL in boys with DMD and their caregivers. To evaluate the HRQoL in boys with DMD, the EuroQoL 5-Dimension questionnaire was used with Indian tariffs.
Materials & Methods
This study was undertaken at the department of Pediatric Neurology, Advanced Pediatric Center Postgraduate Institute of Medical Education and Research, Chandigarh. This study was approved by the Institutional Ethical Committee. The study protocol was registered with the Clinical Trials Registry India (CTRI/2021/06/034274), and the protocol is published with International Registered Report Identifier (IRRID; PRR1-10.2196/42491). Written informed consent/ assent was obtained from all the participants, maintaining confidentiality and autonomy of patient and their caregiver.
Study design, setting, and population
Cross-sectional analysis of baseline data of a prospective study was used to study the SES and its determinants. This is a sub-analysis of baseline data of a prospective non-randomised intervention clinical trial (quasi-experimental). This study was conducted in pre-intervention (phase 1) and post-intervention (phase 2). In phase 1, patients received standard care. The intervention was based on the patient-centred care (PCC) model and included a comprehensive DMD telecare component. This component featured teleconsultation as a key element in reducing in-person physicians’ visits to the health facility7. Boys with DMD (5-15 yr) and their primary caregivers were recruited from a public tertiary care centre in North India. Children with a genetically confirmed diagnosis of DMD were enrolled. The person who looked after the affected child in the hospital or at home (parents or family members) was considered as the primary caregiver. This excluded hospital staff and paid workers hired by the family. Participants were recruited consecutively from an outdoor clinic by the paediatric neurologist. Participants with any other coexisting medical or psychiatric illness or mental retardation were excluded.
Sample size & study period
DMD is a rare disease with an incidence of one in every 5000 boys. The sample selection in the trial/study in a manner like epidemiological studies is not possible. For such conditions, usually, convenience sampling is taken. The method was non-probability hospital-based sampling. For phase one, descriptive study, the study population comprised 100 children with DMD and their caregivers. Study enrolment started in June 2021 and was completed in March 2022 with a total of 100 children affected with DMD and their respective caregivers.
Data collection and tools used
Affected children and primary caregivers were interviewed regarding their social and demographic characteristics and QoL after obtaining an informed consent/assent.
Socioeconomic status was assessed using the OP Agrawal scale, a 22-item questionnaire evaluating income, education, occupation, assets, social participation, and living conditions, with scores ranging from 22 to 19817. Families were categorised as very high (>76), high (61-75), medium high (46-60), medium low (31-45), poor (16-30), or very poor (≤15). However, none of the participants fell into the very poor or very high categories. So, for better understanding and analysis, the data were transformed into three categories: high (very high and high, i.e., more than 75); medium (medium high, i.e., 46-60) and lower (medium low, poor and very poor, i.e., less than or equal to 45).
Two tools were used to assess the HRQoL of paediatric study population, while a generic tool was used to evaluate the QoL of their caregivers (parents/carers). EuroQoL 5-Dimension questionnaire with the Visual Analogue Scale (EQ-5D-3L & VAS) and neuromuscular module of QoL used for HRQoL in children. The EQ-5D-3L evaluates health across five elements: mobility, self-care, usual activities, pain, and anxiety), each element is graded on a 5-level scale, and the combination of responses forms a 5-digit health profile. Later this profile is converted to a single utility value using the Indian tariff set for adults, applied as a proxy for paediatric use ranging from 0-1, and a higher index represents better QoL. The Paediatric Quality of Life Inventory Neuromuscular Module was used as the second tool to assess the HRQoL18. This scale has 25 items and three domains: Neuromuscular disease (17 items focused to the disease-related symptoms), Communication (3 items addressing patient’s ability to communicate about their illness with healthcare providers and others), and Family Resources (5 items corresponding to family financial and social support systems). The scale used in this study ranges from 0 to 100, where higher scores mean a better QoL (HrQoL).
Overall QoL of caregivers was assessed using the World Health Organization Quality of Life-BREF (WHOQOL-BREF)19. The questionnaire has 26 items measuring an individual’s QoL across different cultures. This questionnaire covers four domains: physical health, social relationships, psychological health, and environment. It has two more items that measure overall QoL and general health. The items are rated on a 5-point scale from 1 (low) to 5 (high). Item 3 is reverse coded. The scale used in this study ranges from 0 to 100 higher score is indicative of better QoL.
Data management and analysis
Primary data were first entered in Epi Info software version 7.0 (https://www.cdc.gov/epiinfo/support/downloads.html), and data were analysed using both Epi Info 7 and SPSS software (version 23; IBM Corp). Spearman correlations, an additional application of post hoc Bonferroni correction was used to determine the relationship between HRQoL in children measured using EQ5D and PedsQoL NM, QoL of caregivers into four domains at the baseline with SES and progression of disease. A stratified analysis was also conducted to explore the relationship between SES and HRQoL. Multiple linear regressions were employed to examine the actual impact of SES on QoL while accounting for other covariates and controlling for the confounding effects of covariates. Education of the main caregiver, family structure, age of the affected child, family history, type of disease, ambulation status, and SES score were covariates studied.
Result
A total of 100 boys with DMD (mean age: 8.32 ± 2 yr) were enrolled, mostly ambulatory, with some wheelchair-bound (mean age: 8.22 ± 1.9 yr). Participants were primarily from the middle SES (Supplementary Table I), rural areas, and nuclear families, and cared for by matriculate caregivers, with mothers being the main caregivers. Most of the participants were from Punjab, though many travelled from distant or challenging terrains. Symptoms typically appeared between ages 3–8 yr, with frequent falls as the most common initial sign. A family history of DMD was noted in a few cases, and symptoms were mainly identified by family members, followed by school staff or incidental laboratory findings. Many parents had no prior knowledge of DMD at the time of diagnosis (57%) (Table I).
| Baseline characteristic | Clinical severity | P value | |||
|---|---|---|---|---|---|
| Total, n (%) | Ambulatory, n (%) | Non-ambulatory, n (%) | |||
| SES status | Upper | 7 (7) | 5 (71.4) | 2 (28.6) | 0.120 |
| Middle | 51 (51) | 46 (90.2) | 5 (9.8) | ||
| Lower | 42 (42) | 40 (95.2) | 2 (4.8) | ||
| Education status of the main caregiver | At least graduate | 24 (24) | 19 (79.2) | 5 (20.8) | 0.009 |
| Matriculation | 46 (46) | 46 (100) | 0 (0) | ||
| Less than matriculation | 30 (30) | 26 (86.7) | 4 (13.3) | ||
| Family structure | Nuclear | 54 (54) | 49 (90.7) | 5 (9.3) | 0.602 |
| Joint | 46 (46) | 42 (91.3) | 4 (8.7) | ||
| Locality | Urban | 28 (28) | 27 (96.4) | 1 (3.6) | 0.731 |
| Rural | 72 (72) | 64 (88.9) | 8 (11.1) | ||
| Distances of provinces to the health facility | Nearby travel | 58 (58) | 54 (9) | 4 (6.9) | 0.595 |
| Nearby difficult travel | 21 (21) | 29 (90.6) | 2 (9.5) | ||
| Farthest travel | 21 (21) | 16(94.1) | 3 (14.3) | ||
| Respondent at baseline | Mother | 58 (58) | 53 (91.4) | 5 (8.6) | 0.0048 |
| Father | 38 (38) | 34 (89.5) | 4 (10.5) | ||
| Others | 4 (4) | 3 (75) | 1 (25) | ||
| Patients age in yr | Mean ±SD | 8.32±2 | 8.22±1.9 | 9.3±2.1 | 0.153 |
SES, socioeconomic status
The EQ-5D-3L utility index scores for children’s HrQoL were computed using the recently developed adult tariff value set for India, which was taken as a proxy for the paediatric age group20. The mean EQ-5D utility score at baseline (recruitment) was 0.58±0.38, while the patients’ self-rated health assessed using the EQ-VAS, was 71.3±20.4 (Table II). In addition to the EQ-5D-5L, the neuromuscular module of PedsQL questionnaire was used to assess HrQoL in affected boys. Children aged 8–12 yr and teenagers aged 13–18 yr completed the questionnaire themselves, while for younger children under eight yr, parents or guardians provided responses as proxies. The average scores from the PedsQL™ were: physical health: 77.7±17.7, communication: 39.3±31.0, and family resources: 30.2±32.8 (Table III).
| Quality of life (N=100) | Scales |
Mean score±SD (Overall) |
Clinical Severity | P value | Post Hoc (Bonferroni) | ||||
|---|---|---|---|---|---|---|---|---|---|
| I | II | III | IV | V | |||||
| HrQoL in children | EQ 5D-3L utility index for Children score (0-1) | 0.58±0.35 | 0.98±0.02 | 0.78±0.22 | 0.50±0.35 | 0.19±0.24 | 0 | 0.00 | I>III (single tailed); I>IV; II>III and IV; III>IV (single tailed) |
| EQ-VAS (0-100) | 71.74±19.93 | 91.67±2.89 | 78.91±14.79 | 68.07±20.87 | 61.25±23.11 | 25 | 0.002 | II>III (single tailed) | |
|
PedsQLTM 3.0 Neuromuscular Module. (Physical Health) Score (0-100) |
77.7±17.7 | 99.0±1.7 | 84.9±11 | 74.4±19.3 | 68.7±13.0 | 41.2 | 0.03 | I>III (single tailed); I>IV; II>III; II> IV (single tailed) | |
|
PedsQLTM 3.0 Neuromuscular Module. (Communication) Score (0-100) |
39.3±31 (0-100) |
- | 47.6 ± 42.8 | 36.0±26.6 | 41.6±27.4 | - | 0.48 | NS | |
|
PedsQLTM 3.0 Neuromuscular Module. (Family Resources) Score (0-100) |
56.8±33.7 (0-100) |
- | 63.6±40.4 | 56.2 ±32.3 | 45.0±26.4 | - | 0.52 | NS | |
|
QoL of caregivers (WHOBREEF) |
Overall quality of life Score (0-100) |
29.7±26 | 16.7 ±28.9 | 34.4 ±31.6 | 29±23.2 | 25.0±18.9 | 0 | 0.503 | NS |
|
Overall health Score (0-100) |
53.0±34.7 | 99.7 ±14.4 | 46.9 ±34.0 | 55.3 ±34.7 | 53.1±31.1 | 0 | 0.11 | NS | |
|
Physical domain Score (0-100) |
50.6±14.4 | 46.0±19.3 | 51.7±12.0 | 49.2±15.4 | 49.6±13.6 | 31 | 0.62 | NS | |
|
Psychological (N=100) Score (0-100) |
49.8±16.8 | 50.0±27.1 | 54.8±14.7 | 46.8±16.6 | 54.7±14.74 | 19 | 0.43 | NS | |
|
Social relationship (N=100) Score (0-100) |
54.7±26.9 | 77.0±6.9 | 57.0±26.0 | 54.0±27.5 | 48.5±24.4 | 0 | 0.16 | NS | |
|
Environmental (N=100) Score (0-100) |
45.6±24.7 | 60.7±23.9 | 48.2±24.7 | 42.5±24.3 | 57.2±21.6 | 0 | 0.83 | NS | |
HrQoL: Health-related Quality of Life; NS, not significant; WHOBREEF, World Health Organization Quality of Life-BREF
|
Dependent variables of QoL (N=100) |
Predictors standardized coefficients (P value) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| SES | Education status of main caregiver | Family structure | Locality | Distances of provinces to the health facility | Respondent at baseline | Age in yr at baseline | DF | Parent’s knowledge of DMD | Clinical Severity | CHE | EQ 5D-3L utility index | ||
| HrQoL in children | EQ 5D-3L utility index for Children Score (0-1) |
0.11 (0.41) |
0.1 (0.46) |
-0.10 (0.29) |
-0.13 (0.17) |
0.20 (0.04) |
-0.01 (0.88) |
-0.42 (0.00) |
- |
0.06 (0.51) |
-0.29 (0.001) |
- | - |
| PedsQL 3.0 Neuromuscular Module. (physical health) Score (0-100) |
-0.02 (0.88) |
-0.06 (0.67) |
-0.08 (0.42) |
0.10 (0.32) |
0.20 (0.048) |
-0.06 (0.53) |
-0.45 (0.00) |
- |
-0.01 (0.95) |
-0.18 (0.056) |
- | - | |
|
QoL of caregivers (WHOBREEF) |
Overall quality of life score (0-100) |
0.32 (0.002) |
- | - |
-0.01 (0.89) |
-0.03 (0.74) |
- | - | - | - | 0.13 (0.21) | - |
-0.06 (0.55) |
| Overall health score (0-100) | - | - | - | - | - | - | - | - | - | - | - | - | |
| Physical domain score(0-100) | - | - | - | - | - | - | - | - | - | - | - | - | |
| Psychological score (0-100) |
0.31 (0.048) |
-0.05 (0.74) |
-0.16 (0.13) |
-0.02 (0.84) |
- | - |
0.18 (0.09) |
- |
0.02 (0.83) |
- |
0.09 (0.41) |
||
| Social relationship score (0-100) |
0.42 (0.004) |
-0.06 (0.65) |
-0.09 (0.37) |
0.15 (0.14) |
-0.02 (0.86) |
0.09 (0.32) |
-0.04 (0.70) |
0.11 (0.25) |
-0.13 (0.20) |
-0.03 (0.79) |
0.13 (0.24) |
||
| Environmental score (0-100) |
0.49 (0.00) |
-0.12 (0.36) |
-0.124 (0.16) |
-0.06 (0.49) |
-0.15 (0.11) |
-0.07 (0.38) |
0.01 (0.91) |
- |
0.02 (0.85) |
0.133 (0.12) |
0.03 (0.77) |
0.25 (0.01) |
|
SES, socioeconomic status; CHE, catastrophic health expenditure; DF, distress financing; NB: A hyphen (-) indicates that the predictor was not included in the respective regression model
The EQ-5D index demonstrated a significant positive correlation with the Physical Health and Family Resources modules of PedsQL (r=0.59; P< 0.001). However, no correlation was observed with the communication scores. Post hoc analysis using the Bonferroni correction revealed that the EQ-5D utility index scores at stages I and II were significantly higher than those at stage IV. Additionally, scores at stage II were significantly higher than in stage III. A single-tailed comparison showed that stage I scores were higher than stage III, and stage III scores were higher than stage IV (Table II).
Caregivers rated their overall QoL considerably worse than their HrQoL, indicating that additional aspects of their lives were negatively affected. This required further exploration. The WHOBREEF scale examined four domains: physical, psychological, social, and environmental factors (Table II). Caregivers reported good physical QoL across all stages except at stage V, where it was moderate. However, as stage V included only one child, conclusions for this stage remain limited. The psychological health of the parents was compromised across all disease stages but did not show significant variation with the disease progression. Stage I showed lower psychological health, likely due to the emotional impact of the initial diagnosis. Social health declined with disease severity, though this trend was not statistically significant (ANOVA P=0.16). Caregivers reported excellent social relationships in stage I, which declined moderately with disease progression. Environmental health remained good across all stages, suggesting that caregivers felt health-related facilities were accessible regardless of disease severity. The study found that HRQoL (EQ-5D-3L utility index and PedsQoL scores) in boys with DMD decreased significantly with disease severity and age. Linear regression revealed that EQ-5D utility scores changed by 18.9 per cent with every six-month increase in age (Figure).
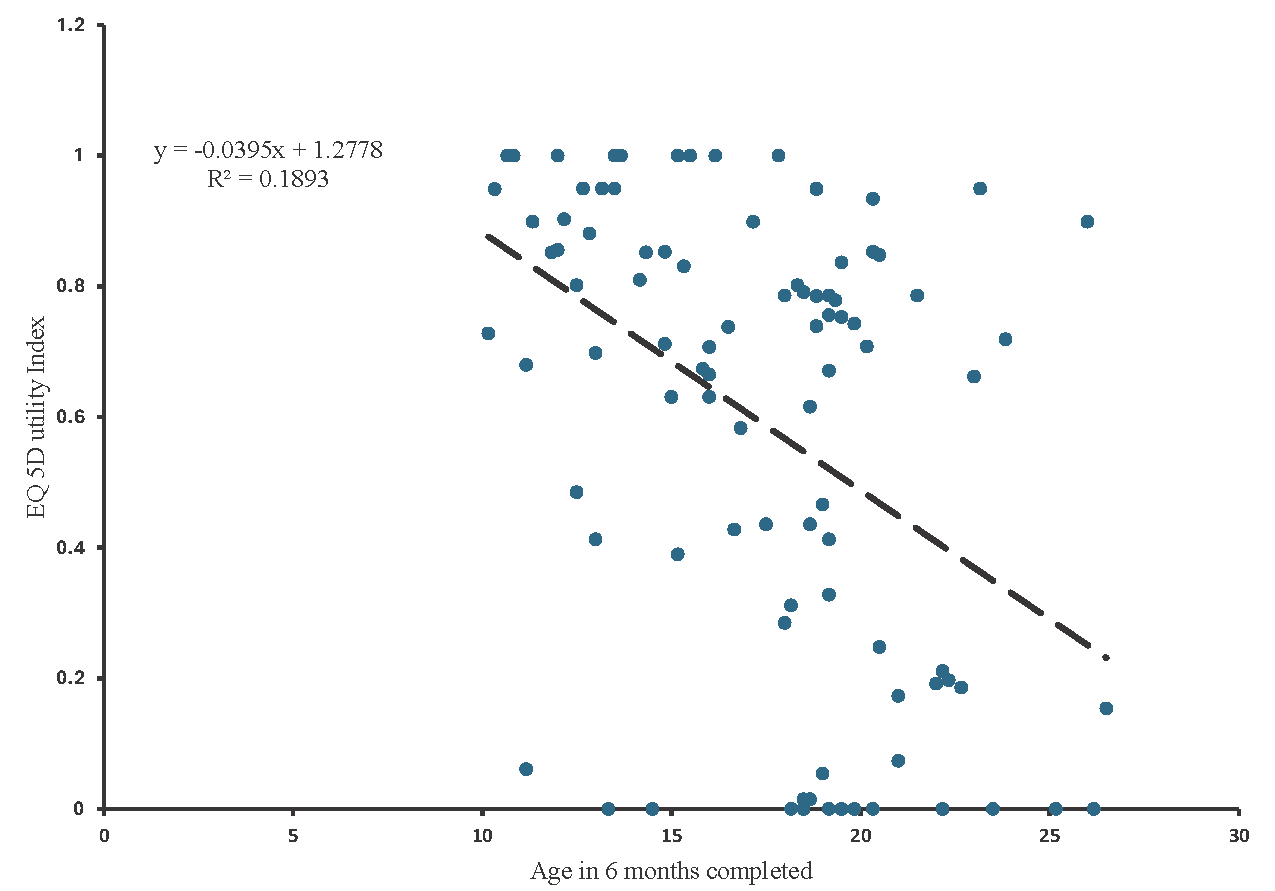
- EQ 5D-3L utility index scores inversely associated with advancing age: Linear regression.
HRQoL scores (EQ-5D and PedsQoL) of children were not significantly associated with the socioeconomic status (SES) (r=0.04; P=0.708) (Supplementary Table II). Stratified analysis showed no significant difference in EQ-5D utility scores across SES groups (0.60, 0.57, and 0.59 for high, middle, and low SES, respectively) (Supplementary Table III). However, utility scores significantly differed across clinical severity groups: 0.8 for Pre/Early Ambulation, 0.50 for Late Ambulation, and 0.17 for Non-Ambulatory (Supplementary Table IV).
The environmental and social relationship domains of caregiver QoL were positively correlated with EQ-5D utility scores (r=0.22, P=0.028; r=0.21, P=0.033), but not with PedsQoL scores of children (r=0.17, P=0.086; r=0.18, P=0.066). The psychological and physical health of caregivers were independent of children’s HRQoL. Caregiver QoL was significantly correlated with socioeconomic status across all domains, suggesting that caregivers’ well-being is influenced by their socioeconomic status. Additionally, the environmental and social relationship domains of caregiver QoL were also influenced by children’s HRQoL. The unit change in EQ 5D-3L utility index scores changed the mean environmental health and social relationship changes by 15.7 and 17.0, respectively. All four domains of QoL in caregivers were directly associated with SES. The model fit was significant. Linear regression analysis revealed that caregiver QoL domains – psychological, social relationships, and environment – changed by 6.5, 19 and 35.3 per cent, respectively, with each single-unit change in socioeconomic status (SES).
Multiple linear regression analysis was conducted to account for potential confounders (Table III). After adjustment, children’s HRQoL was significantly inversely associated with age and disease severity and directly associated with distance to health facilities. Caregiver’s overall QoL, psychological, social relationships, and environmental QoL were directly linked to SES, while environmental QoL was associated with children’s HRQoL. The caregivers ‘physical health QoL was independent of these factors. Analysis of variance for the multiple regressions related to QoL has been given in supplementary table V.
Discussion
This study explored the HRQoL of children and caregivers of children with DMD. The results have shown that HRQoL of boys with DMD was significantly associated with age and clinical severity but did not correlate with SES. Unlike for boys, the global QoL of caregivers was associated with SES. After adjusting for all the risk factors, the age and clinical severity (ambulation status) were significantly associated with a decrease in HRQoL of affected boys. Distance of provinces to the health centre was found to be directly associated with the HRQoL of boys. On the other hand, adjusted QoL of caregivers was found to be significantly associated with the socioeconomic status of the family, but HRQoL of children did not follow the same. Caregiver’s environmental health was found to worsen with deterioration in their child’s HRQoL.
Despite the challenges of the child’s illness, caregivers’ physical and overall QoL remained largely unaffected. These findings highlight the differing impacts of the disease on children and caregivers, emphasising the need to address their distinct needs through targeted interventions to improve overall well-being.
QoL of affected children
The neuromuscular module of PedsQoL, being more disease-specific, provides deeper insights into this condition. The EQ-5D index showed a significant positive correlation with the physical health domain, highlighting its effectiveness as a generic HRQoL measure comparable to the disease-specific PedsQoL neuromuscular module. Both tools demonstrated a strong correlation, affirming EQ-5D-5L’s reliability in reflecting paediatric HRQoL. Moreover, unlike PedsQoL, EQ-5D-5L enables quality-adjusted life year (QALY) estimation.EQ-5D summarises HRQoL into a single value, making it particularly valuable for economic evaluations and cost-effectiveness assessments of emerging therapies21. Summarisation of QoL into a single number makes it easier to compare different countries, time-periods, and diseases21. Findings on the quality of life in boys with DMD are mixed; while some studies indicate it is lower compared to healthy peers, others report no significant difference22,23. However, it is possible that the findings of such studies were influenced by how QoL was measured within the studies themselves. This potential benefit gives the EQ-5D an edge over other instruments, though its suitability for use in rare conditions remains underexplored. It is essential to assess whether this generic HRQoL measure is meaningful, applicable, and easily understood by individuals living with rare conditions.
In a multicentric cross-sectional study from the US and UK with about 200 responses, QoL was assessed using self- or proxy-reported EQ-5D-3L for individuals with DMD aged 1 to 48 yr. EQ-5D index was higher in ambulatory than non-ambulatory patients (0.6 vs. 0.3, P< 0.001), the same as reported in the present study (0.62 vs. 0.17, P=0.08). A study24 from Germany using the PedsQL™ Neuromuscular Disorders Module (Version 3.0) found that HRQoL decreased with disease progression, with the most significant decline observed between stages II and III. Similarly, in the present study, HRQoL measured by PedsQL™ showed comparable trends, while EQ-5D highlighted the most pronounced decline from stage III to IV, corresponding to the transition from ambulatory to non-ambulatory status. The decline in HRQoL from ambulatory to non-ambulatory patients was more in the present study as compared to the US and UK. In developed countries, the available comprehensive care (medical home) and a strong multidisciplinary support system (inclusive society) provide a better QoL even in patients with advanced stages of the disease25. In a multicentric longitudinal study with a 12-month follow up period mean self-reported PeadsQoL score was 64.4, while in the present study, it was 71.5. The QoL scores were higher in this cohort, as only 91 per cent were ambulatory26. In contrast, self-rated health (EQ-VAS) by children showed no significant decline across disease stages (Table II). However, these scores were notably lower compared to those reported in a U.S. study of DMD males aged 12-40 yr27.
Previous literature indicates a direct correlation between SES and the HRQoL for individuals with chronic conditions. The study from Germany, which evaluated the HrQoL of 11,177 individuals affected by six common chronic diseases using the EQ-5D-3L instrument, revealed that those in lower SES brackets experience a dual burden. They not only suffer more from health issues but also have a reduced HRQoL14. In contrast to previous research, the present study presents a divergent outcome, indicating no correlation between SES and HRQoL in children. This may be due to the fact that the studied disease is rare, and the study population was children.
QoL of caregiver with affected children
WHOQOL-BREF tool is a more generic questionnaire analysing the QoL in a general context, regardless of how the disease affects the family, so it is more comparable28,29. In a study conducted to explore the burden of social and professional support in families of individuals with muscular dystrophies (MDs) in Italy, the maximum respondents were females, and 77 per cent reported feeling of loss, 74 per cent felt sad, and 54 per cent felt constrained in leisure activities. About 3.2 per cent of caregivers always felt depressed, while only a small percentage (3.6%) reported facing economic challenges in this regard30. The present study was almost like the cohort from Italy majority of respondents as caregivers were females, and a similar percentage (53%) of caregivers found a great deal of difficulty in getting an opportunity for leisure activities. However, a much higher percentage (32%) felt depressed. Comprehensive care management should prioritise psychological support for caregivers, as they play a vital role in the well-being of individuals with muscular dystrophy. Ensuring caregivers have access to mental health resources can help improve their QoL. About the same proportion of caregivers were informed regarding the disease. Scores of QoL of social relationships at baseline for caregivers suggest that moderate social support from relatives and friends was available (the psychological burden was directly related to the severity of the disease in the Italian study). In the present study QoL of psychological health of caregivers and baseline was moderate and no association with the severity of disease was ascertained. Only 44 per cent of caregivers felt safe in their day-to-day life.
Like any other genetic disease, DMD has an impact on several aspects of life, ranging from lifelong dependency, associated social stigma and economic burden31. A cross-sectional study from Southern Karnataka, India, assessed the QoL and mental health of caregivers of genetic disease patients using the WHOQOL-BREF scale. The median QoL scores for physical health, psychological, social relationships, and environmental health were 81, 69, 75, and 69, respectively, with psychosocial, environmental, and social domains being most affected32. In the present study, caregivers of DMD patients reported lower median scores of 56, 56, 56, and 50 for these domains, indicating a greater QoL impact. Similarly, a study from Brazil assessing caregivers of children with asthma using the WHOQOL-BREF reported mean scores of 63.03 (physical), 63.66 (psychological), 63.74 (social), and 55.38 (environmental), highlighting the comparatively severe burden on caregivers of DMD patients29. The most affected domain was environmental health. Environmental health encompasses financial resources, safety, access to health and social services, quality of living conditions, educational opportunities, recreational facilities, general environmental factors, and transportation availability. Most family resources such as material support and caregiving assistance – as well as challenges like concerns about the future, are potentially modifiable. These aspects can be targeted through practical interventions to enhance the quality of life of family members29. Psychological support that encourages caregivers to recognize their efforts and reframe stressful situations in a more positive light can enhance coping strategies and contribute to better QoL29.
A web-based survey was conducted by Schwartz et al33 on caregivers with and without DMD stratified by subject age group. The impact of disease was measured in terms of QoL, resilience, caregiver impact, financial strain, stressful life events, out-of-pocket expenditures, work productivity, and unrealised ambitions. Caregivers of children with DMD reported good physical health but poor mental health, with caregiving for teenagers posing the greatest challenges. Many caregivers sacrificed education and careers to meet caregiving demands and faced hidden costs affecting health and finances. Despite these challenges, DMD caregivers exhibited notable resilience and positivity33. Similarly, in the present study, caregiver QoL across physical, psychological, social, and environmental domains remained stable despite disease progression. To enhance the QoL across a population, it is essential to prioritise the improvement of QoL for individuals situated at the lower spectrum of the socioeconomic scale. This approach ensures that progress in QoL is inclusive and equitable, leading to significant advancements at the broader population level34. Caregiver’s environmental health and social relationship are also directly associated with the HRQoL of their child. Social relationship is the connection and interactions an individual has with others, including family, friends, colleagues, and the broader community. These relationships influence social support and emotional well-being and can impact physical health.
Our study is not without limitations. One significant limitation was that most of the boys in the study were from moderate to low SES, with only a few from higher socioeconomic backgrounds. Another limitation is that most of the participants were ambulatory boys visiting the health facility, primarily within the age group of 5 to 12 yr. The non-ambulatory stage of the disease (Stage V) has limited representation in the study population. Lastly, we did not account for the scales of QoL as reported by the children themselves or by their caregivers as proxies.
In conclusion, the QoL of DMD patients is closely linked to disease progression, while caregiver QoL is primarily influenced by family SES. The study highlights that children’s QoL is solely influenced by disease progression, not SES, and can only improve through therapeutic interventions targeting disease progression. The lack of association between HRQoL and SES in DMD, unlike other chronic diseases, may be due to inadequate education and awareness among patients and caregivers regarding the rehabilitation requirement of a rare disease. While access to rehabilitation facilities, orthotic devices, wheelchairs, and therapeutic medications is typically influenced by SES, these factors showed no strong correlation with QoL in our findings. Policies like the Rare Disease Policy have not effectively reached to community level, with provisions for orthotic devices and wheelchairs often unavailable. Limited awareness also hinders demand for rehabilitation services and end-of-life care, even at Centres of Excellence, leading to inadequate policy implementation and unmet needs, ultimately diminishing the impact on perceived QoL.
The high variance in QoL data across different disease stages due to stratification highlights the need for longitudinal studies to assess actual changes in QoL over time. Interventions for families of lower SES are essential to improve caregivers’ QoL, an often-overlooked aspect. Interventions and measures for families belonging to lower SES are required to improve QoL in caregivers, which is often overlooked. It is essential to address the diverse experiences of caregivers across different socioeconomic and educational backgrounds. Tailored, patient-centred interventions and support programmes may be designed to meet the specific needs associated with caregiver’s SES and education levels.
Financial support & sponsorship
None.
Conflicts of Interest
None.
Use of Artificial Intelligence (AI)-Assisted Technology for manuscript preparation
The authors confirm that there was no use of AI-assisted technology for assisting in the writing of the manuscript and no images were manipulated using AI.
References
- Quality of life in a broader perspective: Does ASCOT reflect the capability approach? Qual Life Res. 2018;27:1181-9.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- What factors influence parents’ perception of the quality of life of children and adolescents with neurocardiogenic syncope? Health Qual Life Outcomes. 2016;14:79.
- [PubMed] [Google Scholar]
- A review of quality of life themes in Duchenne muscular dystrophy for patients and carers. Health Qual Life Outcomes. 2018;16:237.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Quality of life of patients with Duchenne muscular dystrophy: From adolescence to young men. Disabil Rehabil. 2017;39:1408-13.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnosis and management of Duchenne muscular dystrophy, part 1: Diagnosis, and pharmacological and psychosocial management. Lancet Neurol. 2010;9:77-93.
- [CrossRef] [Google Scholar]
- Duchenne muscular dystrophy: A practice update. Indian J Pediatr. 2018;85:276-81.
- [CrossRef] [PubMed] [Google Scholar]
- Development and economic evaluation of a patient-centered care model for children with Duchenne muscular dystrophy: Protocol for a quasi-experimental study. JMIR Res Protoc. 2023;12:e42491.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Chronic illness management: What is the role of primary care? Ann Intern Med. 2003;138:256-61.
- [CrossRef] [PubMed] [Google Scholar]
- Health-related quality of life and emotional distress among mothers of sons with muscular dystrophy as compared to sex- and age group-matched controls. J Child Neurol. 2021;36:177-85.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The respiratory management of patients with Duchenne muscular dystrophy: A DMD care considerations working group specialty article. Pediatric Pulmonology. 2010;45:739-48.
- [CrossRef] [PubMed] [Google Scholar]
- The burden of Duchenne muscular dystrophy. Neurology. 2014;83:529-36.
- [CrossRef] [PubMed] [Google Scholar]
- Estimating societal cost of illness and patients’ quality of life of Duchenne muscular dystrophy in Egypt. Value Health Reg Issues. 2023;33:10-16.
- [CrossRef] [PubMed] [Google Scholar]
- Quality of life and rare diseases. Adv Exp Med Biol. 2010;686:251-72.
- [CrossRef] [PubMed] [Google Scholar]
- Health-related quality of life and socioeconomic status: Inequalities among adults with a chronic disease. Health Qual Life Outcomes. 2014;12:58.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Assessment of quality of life with the WHOQOL-BREF in a group of Turkish psychiatric patients compared with diabetic and healthy subjects. Psychiatry Clin Neurosci. 2006;60:693-9.
- [CrossRef] [PubMed] [Google Scholar]
- Living with a chronic disease: Insights from patients with a low socioeconomic status. BMC Fam Pract. 2021;22:233.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- A new instrument (scale) for measuring the socioeconomic status of a family: Preliminary study. Indian J Commun Med. 2005;30:111-4.
- [Google Scholar]
- The PedsQL in pediatric patients with Spinal Muscular Atrophy: feasibility, reliability, and validity of the Pediatric Quality of Life Inventory Generic Core Scales and Neuromuscular Module. Neuromuscul Disord. 2009;19:805-12.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- WHOQOL-Hindi: A questionnaire for assessing quality of life in health care settings in India. World Health Organization Quality of Life. Natl Med J India. 1998;11:160-5.
- [PubMed] [Google Scholar]
- Development of an EQ-5D value set for India using an extended design (DEVINE) study: The Indian 5-level version EQ-5D value set. Value Health. 2022;25:1218-26.
- [CrossRef] [PubMed] [Google Scholar]
- The development of the EQ-5D-5L and its value sets. In: Devlin N, Roudijk B, Ludwig K, eds. Value Sets for EQ-5D-5L: A compendium, comparative review & user guide. Cham (CH): Springer; 2022. p. :1-12.
- [Google Scholar]
- Evaluation of the quality of life of children with Duchenne’s progressive muscular dystrophy. Rev Neurol. 2007;45:81-7.
- [PubMed] [Google Scholar]
- Quality of life, physical disability, and respiratory impairment in Duchenne muscular dystrophy. Am J Respir Crit Care Med. 2005;172:1032-6.
- [CrossRef] [PubMed] [Google Scholar]
- Comparative cost of illness analysis and assessment of health care burden of Duchenne and Becker muscular dystrophies in Germany. Orphanet J Rare Dis. 2014;9:210.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Assessing the appropriateness of the EQ-5D for Duchenne muscular dystrophy: A patient-centered study. Med Decis Making. 2021;41:209-21.
- [CrossRef] [PubMed] [Google Scholar]
- Health-related quality of life and functional changes in DMD: A 12-month longitudinal cohort study. Neuromuscul Disord. 2016;26:189-96.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Estimating health state utilities in Duchenne muscular dystrophy using the health utilities index and EQ-5D-5L. J Patient Rep Outcomes. 2023;7:132.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Measuring carer quality of life in Duchenne muscular dystrophy: A systematic review of the reliability and validity of self-report instruments using COSMIN. Health Qual Life Outcomes. 2022;20:57.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Usefulness of the WHOQOL-BREF questionnaire in assessing the quality of life of parents of children with asthma. Revista Paulista de Pediatria (English Edition). 2015;33:267-73.
- [CrossRef] [Google Scholar]
- Burden, professional support, and social network in families of children and young adults with muscular dystrophies. Muscle Nerve. 2015;52:13-21.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Factors associated with the health-related quality of life among people with Duchenne muscular dystrophy: A study using the health utilities index (HUI) Health Qual Life Outcomes. 2022;20:93.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Quality of life and mental health status among the caregivers of genetic disease patients in Southern Karnataka, India. Clinical Epidemiol Global Health. 2021;11:100795.
- [CrossRef] [Google Scholar]
- Characterizing the quality-of-life impact of Duchenne muscular dystrophy on caregivers: A case-control investigation. J Patient Rep Outcomes. 2021;5:124.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Socioeconomic status and age variations in health-related quality of life: Results from the national health measurement study. J Gerontol B Psychol Sci Soc Sci. 2009;64:378-89.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]






