Translate this page into:
Small-for-gestational-age versus appropriate-for-gestational-age: Comparison of cord blood lipid profile & insulin levels in term newborns (SAGA-ACT study)
Reprint requests: Dr Limmy Loret Lobo, Department of Cardiology, Yashoda Hospital, Secunderabad 500 003, Telangana, India e-mail: limmy.cr89@gmail.com
-
Received: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
The genesis of atherosclerotic lesions, a major cardiovascular risk factor starts in the early stage of life. If the premature development of cardiovascular risk factors can be anticipated during childhood, cardiovascular events can be prevented effectively by taking appropriate measures. This study was carried out to assess the role of in utero malnutrition in cardiovascular disease development by comparing cord blood lipid profiles and serum insulin levels between small-for-gestational-age (SGA) and appropriate-for-gestational-age (AGA) term newborns.
Methods:
Consecutive full-term infants who were born between June 20 and August 19, 2013, at the Obstetric Unit of a Hospital at Secunderabad, India, were enrolled in this study. Participating newborns were divided into SGA group (n = 51; test group) and AGA group (n = 52; control group) based on their gestational age and body weight. Cord blood lipid profile and insulin levels were compared between these two groups.
Results:
As compared to the newborns in AGA group, SGA group of newborns had significantly (P<0.01) higher levels of cholesterol, triglyceride and low-density lipoprotein. No difference was observed between the groups for high-density lipoprotein and insulin levels. Mild and moderate anaemia was observed among mothers of both groups, while severe anaemia was seen in mothers of SGA group only.
Interpretation & conclusions:
SGA newborns exhibited elevated lipid profiles as compared to AGA newborns. Hence, SGA newborns should be closely monitored for cardiovascular morbidities during childhood, adolescence and early adult life.
Keywords
Appropriate-for-gestational-age
cardiovascular risk
cord blood
insulin
lipid
neonates
small-for-gestational-age
Atherosclerotic cardiovascular diseases, comprising coronary heart disease and cerebrovascular diseases, are the single largest cause of morbidity and mortality worldwide. The estimated prevalence of cardiovascular diseases ranges from 6-10 per cent among the Indian population. Further, cardiovascular diseases account for about 52 per cent of deaths among Indian individuals <70 yr of age1. Although sedentary lifestyle, fat-rich diet, obesity, smoking, alcohol, etc., are considered as the major predisposing factors of atherosclerotic cardiovascular diseases in adults, it has been identified that the genesis of atherosclerotic lesions starts much early in life2. Barker in 19953 had proposed a “foetal origin of cardiovascular disease” hypothesis, according to which the origin of the disease lies in utero where adaptations take place in the foetus who are undernourished during middle-to-late gestation. These adaptations can be seen in the form of cardiovascular, biochemical or endocrinological changes related to cholesterol metabolism, insulin responses to glucose and structural and functional alternations in the internal organs, leading to inappropriate foetus growth. The series of these events during the early phase of life may trigger the development of atherosclerotic heart diseases during adulthood3. The awareness and worldwide acknowledgment of this hypothesis highlighted the importance of lipid profile estimation in the paediatric age group. If the premature development of the disease can be anticipated during childhood, the cardiovascular events can be prevented effectively by taking appropriate measures.
It has been widely reported that hypercholesterolaemia, a significant risk factor of cardiovascular disease, can be diagnosed at the time of birth by an elevated level of cholesterol in umbilical cord blood245. Further, the estimation of cord blood lipid profile is feasible because of the ease with which cord blood can be collected at birth and availability of a simple method for detection of lipid and insulin levels from the samples2. The present study was conducted to estimate the significance of in utero malnutrition in the development of cardiovascular disease by comparing cord blood lipid profiles and serum insulin levels between small-for-gestational-age (SGA) and appropriate-for-gestational-age (AGA) term newborns.
Material & Methods
The Small-for-gestational-age versus Appropriate for Gestational Age: Analytical comparison of Cord blood lipid profiles and insulin levels in Term newborns (SAGA-ACT) study was a cross-sectional analysis to compare the cord blood lipid profiles and insulin levels between the SGA and AGA full-term newborns. The study was conducted at the Obstetric Unit of Gandhi Medical College and Hospital, Secunderabad, India, for two months from June 20, 2013. Enrolment was done when the woman included in the study reported to the antenatal ward in labour. Gestational age was calculated based on the last menstrual period and initial ultrasonography reports. The term SGA was used to categorize newborns whose weights were below the 10th percentile for their gestational age. The term AGA was used to categorize newborns whose birth weight was between the 10th and 90th percentile for gestational age. Birth weight percentile was calculated based on the growth curve derived by Alexander et al6 and Oken et al7.
The key inclusion criteria were: full-term pregnancy (37-42 wk) and APGAR (Appearance, Pulse, Grimace, Activity, Respiration) score89 of >6 at one min and 8-10 at five min of birth. The newborns were excluded if the labour was prolonged or medically induced, required resuscitation, the mothers had older gravida or complications such as gestational diabetes, cardiac disease, obesity, hypercholesterolaemia or dyslipidaemia during pregnancy, newborns with birth weight >4 kg or newborns with any major congenital anomaly. All consecutive newborns from mothers who qualified the inclusion criteria and agreed to participate in the study were enrolled to avoid the potential selection bias. Accordingly, a total of 103 newborns, 51 SGA and 52 AGA newborns, were enrolled in the study. The proposal was approved by the Institutional Ethics Committee. Informed written consent was obtained from all participating mothers at the time of enrolment.
Data collection: Cord blood lipid profiles and insulin levels were estimated in each newborn enrolled in the study. Cord blood sample (5 ml) was collected in sterile tubes from the placental side of the umbilical cord within 10 min of birth. The samples were allowed to clot for 10 min, were stored at 4-8°C and were transported to the central laboratory for biochemical analysis. Total cholesterol levels, the primary end-point of the study, were determined by the cholesterol oxidase/phenol + aminophenazone end-point enzymatic method. High-density lipoprotein (HDL) cholesterol levels were determined by detergent/bichromatic end-point method while triglyceride levels were determined by lipase/glycerokinase bichromatic end-point method. All kits were purchased from Siemens Healthcare Global, Germany. Low-density lipoprotein (LDL) cholesterol and very low-density lipoprotein (VLDL) levels were estimated according to the Friedewald's formula10. Total cholesterol/HDL cholesterol ratio was also calculated for each newborn. Apart from lipid profile, insulin levels were estimated from cord blood samples using chemiluminescence immunoassay (Siemens Healthcare Global, Germany). The presence and severity of maternal anaemia were estimated based on haemoglobin (Hb) cut-off criteria: Hb levels <7 g per cent being severe anaemia, 7-9.9 g per cent being moderate anaemia and 10-10.9 g per cent mild anaemia.
Statistical analysis: Z-test was used to determine the statistical difference between the groups. To prove that lipid levels were higher in the SGA newborns than those in the AGA newborns, one-sided (i.e., upper-tailed) statistical test was used. Spearman's rho correlation coefficient was computed to assess the relationship between maternal age and total cholesterol levels of neonates. Further, the SGA and AGA neonates were evaluated for their association with pregnancy-induced hypertension in mothers using the Chi-square test. Statistical analyses were performed using the Statistical Package for the Social Sciences (SPSS) software, version 15 (SPSS Inc., Chicago, IL, USA).
Results
The baseline characteristics of newborns enrolled in the study are described in Table I. The gender distribution was similar in both study groups with males constituting 57.7 per cent of neonates in the AGA group and 56.9 per cent of neonates in the SGA group. The mean gestational age was 38.42 ± 1.29 wk in the AGA group and 37.55 ± 1.04 in the SGA group. There was a significant difference between the AGA group and the SGA group in terms of mean birth weight of newborns (2.80 ± 0.26 vs. 2.05 ± 0.26 kg, P < 0.01); majority of these neonates were delivered vaginally, and the caesarean sections were reported in <10 per cent cases in both groups.
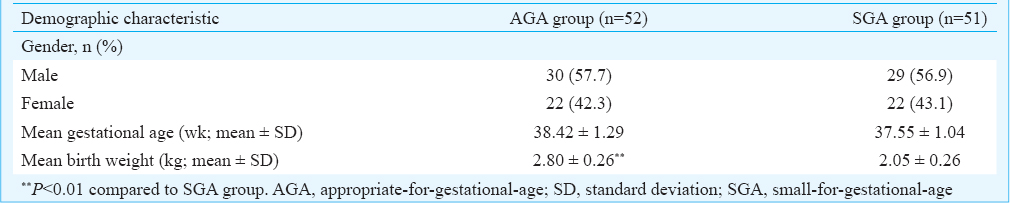
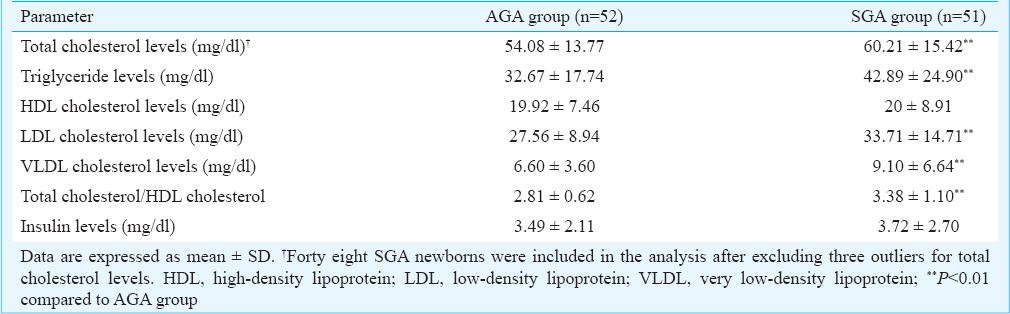
Cord blood lipid profile and insulin levels: Mean cholesterol levels, triglyceride levels, LDL cholesterol levels and VLDL levels were significantly higher in the SGA group than that in the AGA group (P < 0.01). The distribution of newborns according to their total cholesterol levels is depicted in Fig. 1. Twenty three newborns in the SGA group had total cholesterol level more than 60 mg/dl as compared to 13 in the AGA group. The total cholesterol/HDL cholesterol ratio was also significantly higher (P<0.01) in SGA group compared to AGA group. HDL cholesterol and insulin levels were comparable between the AGA and SGA groups (Table II).

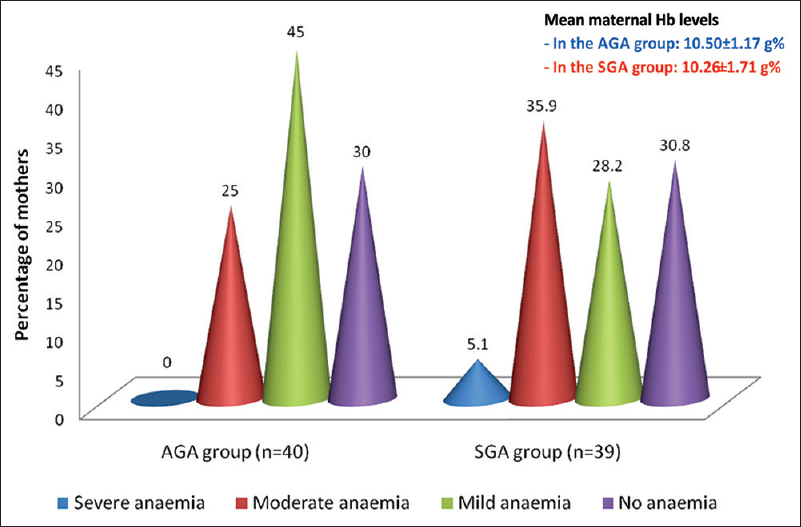
- Frequency distribution of maternal anaemia. AGA, appropriate-for-gestational-age; Hb, haemoglobin; SGA, small-for-gestational-age; Haemoglobin levels (in g%): severe anaemia, <7; moderate anaemia, 7–9.9; mild anaemia, 10-10.9; no anaemia, >11.
Presence of maternal anaemia: Data on maternal haemoglobin levels were available for 40 mothers in the AGA group and 39 mothers in the SGA group (Fig. 2). Accordingly, the mean maternal haemoglobin level was 10.5 ± 1.17 g per cent (range: 8-13 g%) in the AGA group and 10.26 ± 1.71 g per cent (range: 5.5-14 g%) in the SGA group. In the AGA group, 18 (45%) mothers had mild anaemia and 10 (25%) had moderate anaemia. Severe anaemia was not reported among mothers in the AGA group. On the contrary, two (5.1%) mothers in the SGA group had severe anaemia. Further, mild and moderate anaemia were found in 11 (28.2%) and 14 (35.9%) mothers in the SGA group, respectively. Twelve mothers each from both study groups (30.8% of mothers in the SGA group and 30 per cent of mothers in the AGA group) reported haemoglobin levels ≥11 g per cent.
- Total cholesterol levels in newborns. Forty eight SGA newborns were included in the analysis after excluding three outliers for total cholesterol levels. AGA, appropriate-for-gestational-age; SGA, small-for-gestational-age.
Effect of other factors: The maternal age was comparable between the two groups (22.58 ± 2.34 vs. 24.04 ± 3.35). A weak positive correlation was observed between maternal age and total cholesterol levels of all neonates (correlation coefficient r = 0.16, P = 0.11). In particular, the correlation coefficient for maternal age versus cholesterol levels of neonates in the SGA group was 0.21 (P = 0.16), while that of neonates in the AGA group was 0.04 (P = 0.78). The association between the presence of pregnancy-induced hypertension and SGA/AGA outcome in newborns was not significant.
Discussion
Studies have affirmed that low birth weight and intrauterine growth restriction are linked to atherogenic and insulinogenic risk factors, particularly in SGA neonates1112. A study of 1502 pregnancies by Mattioli et al13 reported a 16 per cent occurrence of neonates being SGA. Considering the high prevalence and a high risk of cardiovascular events in SGA newborns, the present study was aimed to identify the cardiovascular risk factors in the earliest stage.
The cord blood lipid profile of newborns investigated in the present study was in line with the findings of other studies done in India or other parts of the world1415. Comparison of study groups revealed that the total cholesterol, triglyceride and LDL cholesterol levels were significantly higher in the SGA group of newborns as compared to the AGA group of newborns. However, the insulin levels were comparable between the two groups. This indicates that inappropriate foetus growth has a significant role in altering lipid metabolism. Further, it can be anticipated that the SGA newborns are at high risk of cardiovascular disease during their adulthood.
There have been discrepancies in reporting the cord blood lipid levels in SGA newborns. Kumar et al11 have reported no association between the cord blood cholesterol levels and birth weight of newborns but demonstrated elevated cord blood triglyceride levels in newborns with growth retardation. Singh et al2 have reported a significant correlation between the cord blood lipid profile and the birth weight of neonate. On the contrary, Elizabeth et al16 reported that neonates with low birth weight had lower levels of cholesterol and triglycerides as compared to controls. Nayak et al15 reported that the triglyceride levels were significantly higher in the SGA newborns as compared to the AGA newborns. Restricted intrauterine growth might be the possible explanation for elevated lipid profile in SGA newborns in the present study. Maternal anaemia could have played a role in the intrauterine growth of these neonates.
Anaemia during pregnancy is a significant health concern worldwide. The health of the mother as well as the foetus is largely influenced by anaemia. A significant association has been reported between maternal anaemia and risk of preterm deliveries, low birth weights, morbidity and perinatal mortality17. A meta-analysis of 12 studies has reported that moderate-to-severe maternal anaemia is associated with >50 per cent increase in the risk of newborn being SGA18. Several biological mechanisms have been proposed including (i) oxidative stress due to low levels of haemoglobin, and (ii) increased production of norepinephrine followed by stimulation of corticotropin-releasing hormone due to iron deficiency leading to intrauterine growth restriction18.
In the present study, about 70 per cent of mothers in both study groups had anaemia during pregnancy. The proportion of maternal anaemia observed in the present study was in line with the World Health Organization report19, which suggested nearly 65-75 per cent prevalence of anaemia among pregnant Indian women. This finding directs that the management and control of anaemia during pregnancy should be enhanced to improve the health of the foetus as well as that of the mother. Further, the occurrence of moderate-to-severe anaemia was higher in the mothers of the SGA group as compared to the AGA group. Overall, 41 per cent of mothers in the SGA group reported haemoglobin levels <10 g per cent as compared to the 25 per cent in the AGA group. These observations indicate that maternal anaemia has a significant role in foetal growth. Further, delivery of SGA neonate is reported to be a significant cardiovascular risk factor for mothers20. Further studies are required to clarify the relationship between maternal anaemia and SGA foetus and to determine whether healthcare during pregnancy has the potential to avoid the maternal and foetal complications.
Our study had certain limitations. A clear differentiation between SGA and intrauterine growth restriction could not be performed in our study. Many mothers were not on regular periodic antenatal monitoring, which impeded the accuracy of several variables such as body mass index, maternal weight gain, haemoglobin levels, placental histopathology, foetal middle cerebral arterial Doppler assessment and symmetric versus asymmetric pattern of intrauterine growth restriction in SGA newborns. Taking into account the financial and time constraints, the sample size was restricted to 100 with 1:1 ratio in both study and control groups. The selection bias was reduced by enrolling consecutive mothers admitted to the hospital. Another major limitation of our study was its inability to determine the cut-off lipid levels for cardiovascular risk stratification. In this context, a large longitudinal study is recommended to find out the clinical significance of higher lipid levels in SGA newborns and to estimate a cut-off level of lipids in neonates for categorization into higher, lower and no-risk levels for developing cardiac diseases in their adult life.
In conclusion, significantly higher cord blood levels of total cholesterol, triglycerides and LDL cholesterol were evident in the SGA group of newborns as compared to the AGA group of newborns. Hence, SGA neonates should be followed up regularly during their adolescence and adulthood to institute timely interventions to prevent rapid development of cardiovascular disease.
Conflicts of Interest: None.
References
- Cardiovascular disease risk factors in Asian Indian population: A systematic review. J Cardiovasc Dis Res. 2013;4:222-8.
- [Google Scholar]
- Cord blood cholesterol in term and preterm newborns. Indian Pediatr. 1994;31:1278-81.
- [Google Scholar]
- Birth weight, cord blood lipoprotein and apolipoprotein levels in Indian newborns. Int J Prev Med. 2010;1:29-33.
- [Google Scholar]
- Ethnic variation of cord plasma apolipoprotein levels in relation to coronary risk level: a study in three ethnic groups of Singapore. Acta Paediatr. 1996;85:1476-82.
- [Google Scholar]
- A United States national reference for fetal growth. Obstet Gynecol. 1996;87:163-8.
- [Google Scholar]
- A nearly continuous measure of birth weight for gestational age using a United States national reference. BMC Pediatr. 2003;3:6.
- [Google Scholar]
- A proposal for a new method of evaluation of the newborn infant. Curr Res Anesth Analg. 1953;32:260-7.
- [Google Scholar]
- Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18:499-502.
- [Google Scholar]
- Cord blood lipid levels in low birth weight newborns. Indian Pediatr. 1989;26:571-4.
- [Google Scholar]
- Is small for gestational age status associated with an increased risk of atherogenesis? Maedica (Buchar). 2013;8:315-20.
- [Google Scholar]
- Inadequate identification of small-for-gestational-age fetuses at an urban teaching hospital. Int J Gynaecol Obstet. 2010;109:140-3.
- [Google Scholar]
- Cord blood lipid profile and associated factors: baseline data of a birth cohort study. Paediatr Perinat Epidemiol. 2007;21:518-24.
- [Google Scholar]
- Correlation of cord blood lipid heterogeneity in neonates with their anthropometry at birth. Indian J Clin Biochem. 2013;28:152-7.
- [Google Scholar]
- Umbilical cord blood nutrients in low birth weight babies in relation to birth weight & gestational age. Indian J Med Res. 2008;128:128-33.
- [Google Scholar]
- Anaemia in pregnancy: a survey of pregnant women in Abeokuta, Nigeria. Afr Health Sci. 2005;5:295-9.
- [Google Scholar]
- Moderate to severe, but not mild, maternal anemia is associated with increased risk of small-for-gestational-age outcomes. J Nutr. 2012;142:358-62.
- [Google Scholar]
- Association between delivery of a small-for-gestational-age neonate and long-term maternal cardiovascular morbidity. Int J Gynaecol Obstet. 2013;123:68-71.
- [Google Scholar]






