Translate this page into:
Role of computed tomography (CT) scan in staging of cervical carcinoma
Reprint requests: Dr S. Thulkar, Department of Radiology, Dr. B.R. Ambedkar Institute Rotary Cancer Hospital, All India Institute of Medical Sciences, Ansari Nagar, New Delhi 110 029, India e-mail: thulkar@hotmail.com
-
Received: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Staging of cervical carcinoma is done clinically using International Federation of Obstetrics and Gynecology (FIGO) guidelines. It is based on physical examination findings and also includes results of biopsy, endoscopy and conventional radiological tests like chest radiograph, intravenous urography and barium enema. These conventional radiological investigations have largely been replaced by computed tomography (CT) and magnetic resonance imaging (MRI) at present. FIGO staging system does not consider CT and MRI mandatory; however, use of these modalities are encouraged. This prospective study was conducted to determine the role of CT in staging work up in women diagnosed with cervical carcinoma.
Methods:
Fifty three women diagnosed with cervical carcinoma were evaluated with contrast enhanced CT scan of abdomen and pelvis. CT scan images were especially evaluated to determine tumour size, invasion of parmetrium, pelvic walls, rectum, urinary bladder and ureters, pelvic or retroperitoneal lymphadenopathy and distant metastases. CT findings were associated with clinical findings and staging, including findings from cystoscopy and sigmoidoscopy.
Results:
There was a poor agreement between clinical and CT staging of cervical carcinoma. Primary tumour was demonstrated on CT in 36 (70%) of 53 patients. CT underestimated the parametrial, vaginal and pelvic wall invasion when compared with physical examination. CT overestimated the urinary bladder and rectal invasion when compared with cysto-sigmoidoscopy, however, CT had 100 per cent negative predictive value (NPV) to exclude bladder and rectal involvement. CT detection of lymph node enlargement and lung metastases influenced the management.
Interpretation & conclusions:
Our findings show that CT scan does not reliably correlate with clinical FIGO staging of cervical cancer. However, it can detect urinary obstruction as well as nodal or distant metastases and thus improves the clinical FIGO staging
Keywords
CT scan
carcinoma cervix
FIGO staging
Staging and treatment decisions for cervical cancer are based on clinical FIGO (International Federation of Gynecology and Obstetrics) guidelines. The FIGO staging system uses findings from physical examination, colposcopy, lesion biopsy, radiologic studies [chest radiograph, intravenous urography (IVU), barium enema] and endoscopic studies (cystoscopy, sigmoidoscopy). When compared with surgical staging, FIGO clinical staging results in under or over staging in 20-40 per cent patients1. Major limitations of clinical evaluation are in the assessment of parametrial and pelvic side wall invasion, estimation of tumour size (especially in endocervical tumours) and the evaluation of lymph node and distant metastasis. In revised FIGO guidelines, the use of cross-sectional imaging techniques is encouraged but not considered as mandatory2.
Computerised tomography (CT) is widely used to improve clinical staging of cervical carcinoma. CT is useful in evaluating tumour size, parametrial invasion, lymph node status and distant metastasis which are all critical prognostic factors in cervical carcinoma1. Conventional techniques like IVU are been replaced by CT which can give details of the ureteral involvement and the functional status of kidneys. Our group has earlier shown that cystoscopy may not be required in patients without evidence of bladder invasion on CT3. The literature suggests that the CT does improve accuracy of clinical staging performed by FIGO guidelines456. Bipat et al7 conducted a meta-analysis on the diagnostic performance of CT and MRI (magnetic resonance imaging) in staging of cervical carcinoma. Sensitivity estimates for parametrial invasion were 55 per cent and for lymph node involvement 43 per cent for CT. For bladder and rectum invasion the sensitivities for CT were 71 per cent. The specificity in evaluating bladder invasion was 73 per cent7. Lymph node status is an important prognostic factor in cervical carcinoma. Both CT and MRI have similar accuracies in the evaluation of pelvic lymph nodes in patients with cervical carcinoma8. Overall, CT is valuable in evaluation of advanced cervical cancer9, and clinical examination is better than CT and MRI for evaluation of early cervical cancer10. However, there are no clear cut guidelines regarding the role of CT scan in improving the FIGO staging of cervical cancer. In 2009, the FIGO revised the staging of cervical cancer and emphasized the role of radiological imaging but did not state as to which imaging was mandatory3. The present prospective study was planned to evaluate the role of CT scan in the staging of cervical cancer in women attending a tertiary care cancer facility in north India.
Material & Methods
The present prospective study was carried out at a tertiary care cancer hospital Dr. B.R. Ambedkar Institute Rotary Cancer Hospital, All India Institute of Medical Sciences, New Delhi, India, after the study protocol was approved by the Ethics Committee. Women who were diagnosed with carcinoma of cervix by biopsy and referred for CT scan evaluation from Radiotherapy clinic were recruited. The study was carried out from September 2009 to April 2011 and during this period 53 consecutive patients who gave written informed consent were included in this study. A total of 100 patients who did not give consent and those who were on treatment or previously treated were excluded.
Detailed medical history was taken and staging of the carcinoma of cervix was done by the senior gynaecologist using revised FIGO staging2. CT evaluation of all the patients was performed and the relevant findings were documented. The findings of CT were compared and correlated with the clinical findings. The final staging using CT was compared with FIGO staging. All patients were stage II or higher and hence correlation with operative findings was not possible.
Computed tomography: All patients underwent contrast enhanced CT of abdomen and pelvis on 4 row multi-detector CT scanner (Volume Zoom, Siemens, Erlangen, Germany) as per the standard protocol11; 120 kV and 160 mAs were used. Patients were given one litre of water soluble oral contrast one hour before the scan. Scanning was done immediately after intravenous hand injection of bolus of 80 ml of contrast; either Iohexol (Omnipaque 350, GE Healthcare, USA) or Iopamidol (Iomeron 400, Bracco, Italy) covering diaphragm up to symphysis pubis. Images were reconstructed with 5 mm thickness at 5 mm interval. Delayed scans of pelvis were taken in relevant cases. Bone windows and MPR (Multi-planar reformatted) reconstructions were made in selective cases.
Analysis of images: The CT images were interpreted by two radiologists having experience in gynaecological imaging. Primary tumour was demonstrated as hypo-enhancing mass within the normally enhancing cervical stroma or as non specific bulky enlargement of the cervix without well demarcated, measurable tumour mass while in others, no demonstrable cervical abnormality was seen on CT.
Irregular cervical margin, parametrial soft tissue stranding, obliteration of periureteral fat planes or an eccentric parametrial mass were taken as signs of parametrial invasion. Ureteral involvement in the form of encasement with or without urinary obstruction and dilation was noted. Extension of tumour to within 3 mm of the pelvic side wall, encasement of iliac vessels, enlargement of obturator or pyriformis muscles were the signs of pelvic wall involvement1. Obstructive hydronephrosis on CT was considered as stage 3b disease. Adjacent organs (bladder or rectum) were considered not involved when fat plane was maintained between tumour and these structures. It was considered as suspicious for invasion when there was wall thickening of rectum or urinary bladder with loss of fat planes between them. Intraluminal extension of tumour was taken as a definite evidence of the involvement.
Presence or absence of enlarged pelvic and retroperitoneal lymph nodes was noted. Short axis nodal diameter of more than one cm and/or evidence of central necrosis on CT were considered as signs of nodal metastasis.
Statistical analysis: The difference between clinical staging and CT staging was determined using McNemar test. For sensitivity/specificities 95% confidence intervals were calculated (http://www.vassarstats.net/clin1.html)12, and for other comparisons kappa statistics were derived using SPSS version 1713.
Results
Fifty three patients with biopsy proven cervical carcinoma who had not received any treatment were included in this study. Age of patients ranged from 33 to 78 yr (median 51 yr). To correlate FIGO staging and CT scan staging for analytical ease stage 3a and 3b were clubbed together similarly 4a and 4b also were clubbed (Table I). The difference between FIGO and CT staging was significant (P < 0.001). Absolute agreement between the modalities in staging was analyzed and was found to be 28.30 per cent, with kappa value of 0.08 ±0.06; suggesting poor agreement between the two staging modalities.

Tumour was clinically palpable in all 53 women, but it was visible on CT scan in 36 (70%) of them. As none of our patients underwent surgery, tumour size and its local extent on CT was associated with clinical examination and cystoscopy/sigmoidoscopy findings only, and CT agreement was determined. Tumour size was assessed clinically by per vaginal examination in all the patients. Tumour size varied from 2 to 10 cm (mean = 4.6 ± 1.2 cm) on clinical assessment and between 2.5 to 9 cm (mean= 5.6 ± 1.4 cm) on CT. The difference was not significant.
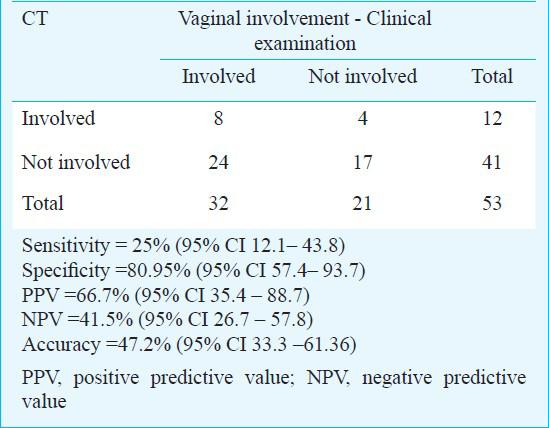
Of the 53 patients, 32 (61.5%) showed vaginal involvement on clinical examination. The sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and accuracy of CT in assessment of invasion of vagina by cervical cancer was 25, 80.95, 66.7, 41.5 and 47.2 per cent, respectively when compared with clinical examination (Table II).
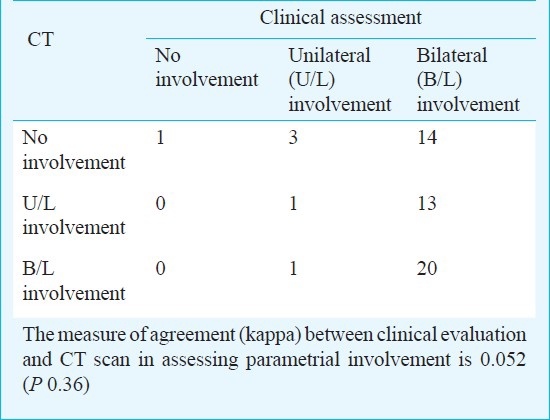
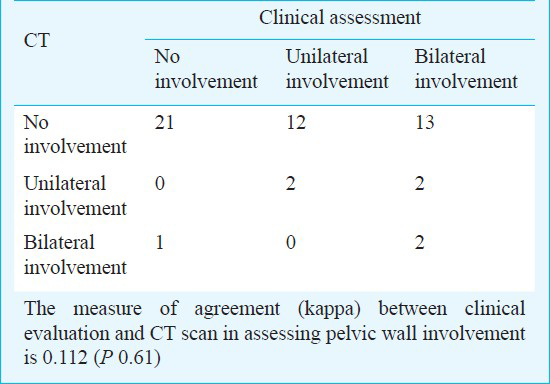
The percentage of agreement between CT and clinical examination in evaluation of parametrial invasion was 41.5 per cent. CT underestimated the parametrial invasion (Table III). Of the 53 patients, 14 (26.4%) had clinical features of unilateral pelvic side wall involvement and 17 (32%) had bilateral involvement. CT showed pelvic wall invasion in seven patients. The percentage of agreement between CT and clinical examination in evaluation of pelvic wall invasion is 47.16 per cent. CT underestimated the pelvic wall invasion when compared with clinical examination (Table IV).
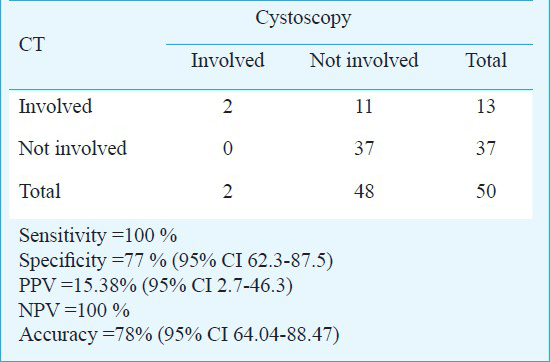
Cysto-sigmoidoscopy was performed in 50 of 53 patients. Two patients showed involvement of urinary bladder and one patient showed rectal involvement. Three patients in whom cysto-sigmoidoscopy was not done, were excluded from this analysis. CT showed definite involvement of urinary bladder in seven patients and suspicious involvement in six patients. The sensitivity, specificity, PPV, NPV and accuracy of CT in assessment of urinary bladder invasion by cervical cancer were 100, 77, 15.38, 100 and 78 per cent respectively (Table V).
CT showed definite involvement of rectum in eight patients and suspicious involvement in five patients. The sensitivity, specificity, PPV, NPV and accuracy of CT in assessment of invasion of rectum by cervical cancer were 100, 75.5, 7.6, 100 and 76 per cent respectively (Table VI). CT showed involvement of pelvic nodes in 11 (20.7%) patients and retroperitoneal nodes in six (11.3%) patients. Obturator and internal iliac nodes were the commonly involved pelvic nodes. As expected, clinical examination could not identify lymph node involvement in any cases.

Forty patients received standard treatment with external beam radiotherapy (EBRT) with chemotherapy followed by intracavitary radiotherapy. Two patients received additional interstitial brachytherapy. Seven patients received palliative radiotherapy. Six patients did not come for treatment. Because of the advanced disease in all patients, none underwent surgery.
Discussion
Staging and treatment decisions for invasive cervical cancer are based on clinical FIGO guidelines. The major limitations of FIGO staging are the discrepancies with surgical staging, inability for lymph nodal assessment and variable intra- and inter-observer variability which would adversely affect treatment decisions14. Treatment options for carcinoma cervix are surgery (radical hysterectomy with pelvic lymph node dissection) and chemoradiation. Surgery is preferred for early stage (up to IIA) while other patients are generally considered for chemo-radiotherapy.
With developments in imaging techniques, cross-sectional imaging modalities like CT and MRI are frequently used and conventional imaging with IVU and barium enema has almost became obsolete in the staging work up of cervical carcinoma. MRI is the imaging modality of choice for local staging of cervical carcinoma15. Positron emission tomography (PET)-CT is not suitable for tumour staging in early cervical cancers; however, it is useful and more accurate than MRI for the detection of lymph nodes and distant metastases and hence, is desirable in locally advanced cervical cancer16. MRI is superior to CT in depiction of primary tumour17. However; in developing countries where the burden of cervical cancer is high, CT is the preferred modality being more widely available and less expensive.
In our study, there was significant disagreement in CT staging and clinical staging. Ozsarlak et al18 reported the overall accuracy of staging for clinical examination, CT, and MRI to be 47, 53, and 86 per cent respectively when compared with surgical findings18. CT has limitations in the depiction of cervical cancer because up to 50 per cent of tumours are isodense to cervical stroma on contrast-enhanced CT and hence not demonstrated14. When the primary tumour is visible, it is hypodense relative to normal cervical stroma. Our study showed similar results. It has been observed that the possibility of missing the primary tumour in CT is higher when the tumour size is small and hence, normal CT does not exclude presence of the cervical cancer14.
We found poor agreement between CT and clinical examination in the evaluation of parametrial invasion in our study. Hancke et al10 reported that clinical examination was more accurate than CT or MRI in assessment of parametrium. In our study, clinical examination showed pelvic wall invasion in 51 per cent patients whereas CT showed in 13.2 per cent patients only. The percentage of agreement between CT and clinical examination in evaluation of pelvic wall invasion was 37.7 per cent in our study which was not significant. Previous study by Whitley et al19 also showed poor sensitivity by CT in diagnosing pelvic wall invasion.
FIGO advocates the use of IVU for the detection of ureteric involvement and hydronephrosis. None of the patients in our study underwent IVU. CT showed hydronephrosis secondary to ureteric involvement in 12 patients. An earlier study has shown that CT is either superior or equal to IVU in assessment of urinary tract involvement by cervical cancer20.
As per the FIGO guidelines all patients with cervical cancer should undergo cystoscopy and biopsy to detect involvement of bladder mucosa2. In our study, CT showed definite involvement of urinary bladder in eight patients and suspicious involvement in six patients. Patients in whom CT showed loss of intervening fat plane only were considered to be having suspicious involvement. For statistical analysis, the patients with suspicious or definite invasion of urinary bladder on CT scan were considered as positive. The high sensitivity and NPV of CT in determining urinary bladder invasion make CT an effective preliminary screening modality and cystoscopy can be done in selective patients. The high sensitivity and NPV of CT make it an effective preliminary screening modality and may obviate sigmoidoscopy in patients with negative CT scan for rectal invasion.
Nodal involvement is one of the important prognostic factors; however, it is not incorporated in the FIGO staging system2. In our study, CT showed involvement of pelvic nodes in 20.8 per cent patients and retroperitoneal nodes in 9.5 per cent patients. Among the pelvic nodes, obturator and internal iliac group of nodes were involved in four patients each.
Treatment plan in all our patients were made according to the clinical FIGO stage and physical status of the patients. CT findings were taken into account for the objective assessment of tumour burden, planning of radiotherapy portals and prognostication of the patients individually. Extended field radiotherapy was given to the patients with retroperitoneal lymphadenopathy. Palliative chemotherapy was offered to the patient with lung metastasis.
Small sample size was a major limitation of our study. All patients presented with advanced stages of the disease therefore, surgery was not feasible. Hence in our study surgical confirmation was not available to assess the accuracy of clinical and CT findings.
To conclude, CT scan does not reliably relate with clinical FIGO staging of cervical cancer. However, it can detect urinary obstruction as well as nodal or distant metastases and thus improve the clinical FIGO staging and has implications on radiation therapy planning and the prognosis.
References
- Revised FIGO staging for carcinoma of the cervix. Int J Gynaecol Obstet. 2009;105:107-8.
- [Google Scholar]
- Revisiting the role of computerized tomographic scan and cystoscopy for detecting bladder invasion in the revised FIGO staging system for carcinoma of the uterine cervix. Int J Gynecol Cancer. 2010;20:368-72.
- [Google Scholar]
- Diagnosis, staging, and surveillance of cervical carcinoma. AJR Am J Roentgenol. 2003;180:1621-31.
- [Google Scholar]
- Role of imaging in pretreatment evaluation of early invasive cervical cancer: Results of the intergroup study American College of Radiology Imaging Network 6651-Gynecologic Oncology Group 183. J Clin Oncol. 2005;23:9329-37.
- [Google Scholar]
- Accuracy of computer tomography and magnetic resonance imaging in the detection of lymph node involvement in cervix carcinoma. Eur Radiol. 2005;15:2469-74.
- [Google Scholar]
- Computed tomography and magnetic resonance imaging in staging of uterine cervical carcinoma: a systematic review. Gynecol Oncol. 2003;91:59-66.
- [Google Scholar]
- Comparison of dynamic helical CT and dynamic MR imaging in the evaluation of pelvic lymph nodes in cervical carcinoma. AJR Am J Roentgenol. 2000;175:759-66.
- [Google Scholar]
- Value of CT scanning in the diagnosis of early cervical carcinoma. Zhonghua Zhong Liu Za Zhi. 2006;28:151-4.
- [Google Scholar]
- Pretreatment staging of cervical cancer: is imaging better than palpation? Role of CT and MRI in preoperative staging of cervical cancer: single institution results for 255 patients. Ann Surg Oncol. 2008;15:2856-61.
- [Google Scholar]
- VassarStats: Web Site for Statistical Computation. available from: http://www.vassarstats.net/clin1.html
- [Google Scholar]
- Staging of uterine cervical cancer with MRI: guidelines of the European Society of Urogenital Radiology. Eur Radiol. 2011;21:1102-10.
- [Google Scholar]
- Clinical impact of 18F-FDG PET/CT in pretreatment evaluation of patients with locally advanced cervical carcinoma. Nucl Med Commun. 2012;33:1081-8.
- [Google Scholar]
- Cervical carcinoma: computed tomography and magnetic resonance imaging for preoperative staging. Obstet Gynecol. 1995;86:43-50.
- [Google Scholar]
- The correlation of preoperative CT, MR imaging, and clinical staging (FIGO) with histopathology findings in primary cervical carcinoma. Eur Radiol. 2003;13:2338-45.
- [Google Scholar]
- Computed tomographic evaluation of carcinoma of the cervix. Radiology. 1982;142:439-46.
- [Google Scholar]
- Excretory urography and computed tomography in the initial evaluation of patients with cervical cancer: are both examinations necessary? AJR Am J Roentgenol. 1984;143:991-6.
- [Google Scholar]






