Translate this page into:
Retropharyngeal abscess in cutaneous T-cell lymphoma, resembling immune reconstitution syndrome
*For correspondence: drpadmasundaram@gmail.com
-
Received: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
A 55 year old diabetic male†, recently diagnosed non-Hodgkin's lymphoma (NHL, cutaneous T cell) presented to department of Medical Oncology, Amrita Institute of Medical Sciences, Cochin, India, in October 2019, with throat pain. Positron emission tomography–computed tomography (PET-CT) showed fluorodeoxyglucose (FDG)-avid lower cervical nodes (Figure A), FDG avid hypodense collection in the retropharyngeal space and extensive unsuspected mediastinitis (Figure B). Cryptococcus neoformans was isolated on culture from the site of abscess. Skin and subcarinal nodes were biopsied (Figure C-E). Amphotericin B (0.8 mg/kg/day) and flucytosine (100 mg/kg/day in 4 divided doses) were given, however, after three days, the patient developed high fever, malaise, oliguria and septic shock. Lactate dehydrogenase, inflammatory markers, CD4+ cells were elevated and the illness mimicked immune reconstitution inflammatory syndrome (IRIS) usually described in HIV patients post-antiretroviral therapy. However, in this non-HIV, NHL (cutaneous T cell type) patient with retropharyngeal abscess, extensive mediastinitis (with tracking sinuses) mimicked IRIS (type 1) after starting antifungal therapy. FDG PET/CT was incremental in upstaging lymphoma (stage IIE) and illustrated all sites of occult infection in neck, beneath sternocleidomastoid, and mediastinum; facilitating complete surgical debridement and faster amelioration of symptoms. Phototherapy (Psoralen and ultraviolet light A i.e PUVA), immunomodulators like steroids were started. The patient showed clinical improvement after 4 weeks of initiating antifungal therapy.
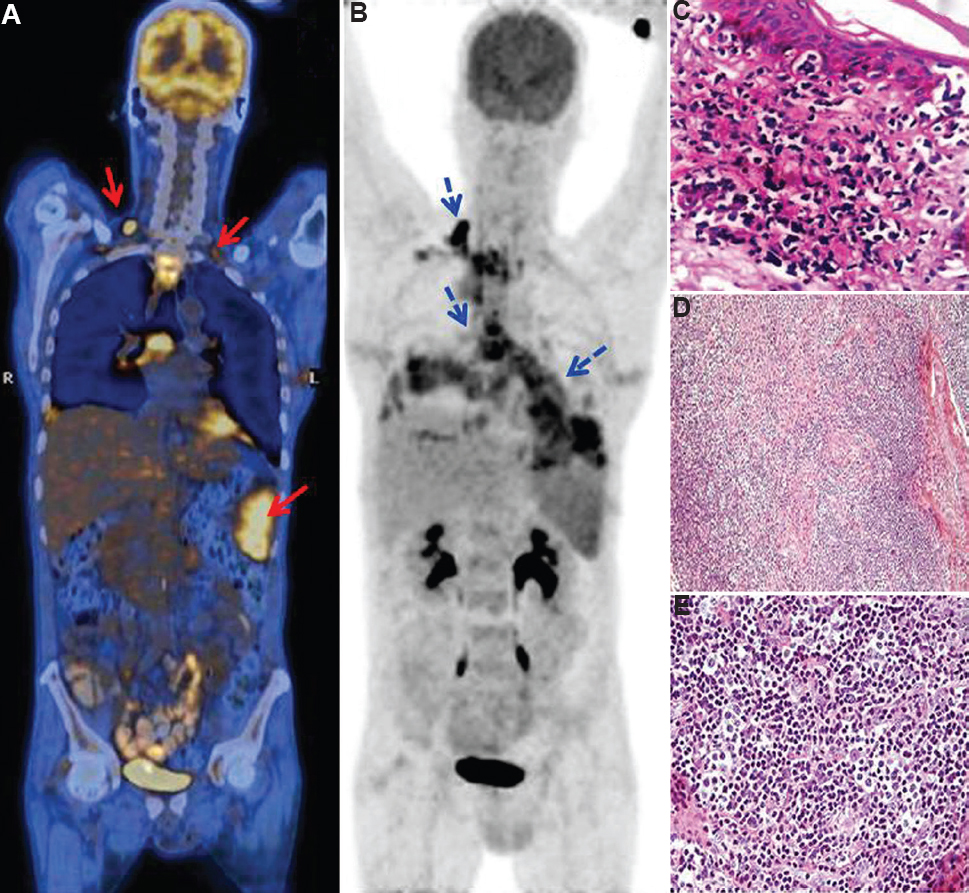
- (A) Fused coronal 18F FDG PETCT (Fluorodeoxyglucose positron emission tomography –computed tomography) image (head to mid-thigh) shows FDG avid bilateral lower cervical lymph nodes (arrows, SUV Max 3.4) and additional splenic involvement (SUV Max 6.7), thereby upstaging NHL to Stage IIE, as per Ann Arbor classification. (B) Coronal PET images (arrow) depict FDG avid retropharyngeal collection and sinus tracking into prevascular, paracardiac spaces, around pericardium and into mediastinum on both sides (SUV Max 17.2). Infection was also noted beneath the right sternocleidomastoid. A large FDG avid subcarinal node was also noted. (C) High-resolution magnified skin biopsy sections H and E, ×40 showing thinned out epidermis, lymphoid infiltrate at dermoepiderma junction with cytological atypia. Cells showing epidermotropism and Pautrier's microabscess formation – suggesting Cutaneous T cell lymphoma. (D) Low-magnification images of subcarinal lymph node biopsy showing infiltration of polymorphic cells with high endothelial venule-like vessels (H and E, ×10) mimicking IRIS. (E) High magnified image of lymph node H and E, ×40 shows proliferation of medium to large-sized lymphoid cells with a clear cytoplasm (clear cells). The cells are CD3+ and CD4+. Findings are mimicking immune reconstitution inflammatory syndrome type I but clinical condition improved with antifungal therapy.
Acknowledgment:
Authors acknowledge Dr K Pavithran, Clinical Professor, Department of Medical Oncology, Amrita Institute of Medical Sciences, Cochin, Kerala for referring the patient
Conflicts of Interest: None.





