Translate this page into:
Resuscitation following trauma & role of trauma training programmes in emergency settings: A literature review & survey
For correspondence: Dr Bhakti Sarang, Department of General Surgery, Terna Medical College & Hospital, Navi Mumbai 400 706, Maharashtra, Indiae-mail: sarangbhakti@gmail.com
-
Received: ,
Abstract
Background & objectives
Traumatic injuries, especially in low- and middle- income countries (LMICs), present significant challenges in patient resuscitation and healthcare delivery. This study explores the role of trauma training programmes in improving patient outcomes and reducing preventable trauma-related deaths.
Methods
A dual approach was adopted, first a literature review of trauma training in LMICs over the past decade, along with a situational assessment survey. For the review of literature, we searched the PubMed database to identify key challenges and innovative practices in trauma training programmes in LMIC’s. The survey, conducted among healthcare professionals in various LMICs, collected direct insights into the challenges and the status of trauma training programmes in these countries.
Results
The literature review analysed 68 articles, with a significant focus on the African subcontinent (36 studies), underscoring the region’s emphasis on research on trauma training programmes. These studies mainly targeted physicians, clinicians, postgraduate trainees in surgical or anaesthesia fields and medical students (86.8%), highlighting innovations like simulation-based training and the cascading training model. In our survey, we received 34 responses from healthcare professionals in India, Belarus, Azerbaijan, Nepal and Pakistan. Around 52.9 per cent reported the absence of established trauma training programmes in their settings. The majority of respondents advocated for hands-on, simulation-based training (94.1%) and emphasised the need for structured training programmes (85.3%), feedback sessions (70.6%) and updated protocols (61.8%). This combined data underlined the critical gaps and potential improvements in trauma training programmes and resuscitation practices in LMICs.
Interpretation & conclusions
Effective trauma care in LMICs requires the establishment of comprehensive, tailored training programmes. Key interventions should include subsidization of pre-existing trauma courses and the adoption of World Health Organization Guidelines for essential trauma care, implementation of trauma quality improvement and review processes and the incorporation of focused assessment with sonography in trauma (FAST) in emergency departments. These steps are crucial for equipping healthcare workers with vital skills and knowledge, fostering a culture of continuous learning and improvement in the realm of trauma care.
Keywords
Emergency
trauma resuscitation
trauma training
LMIC
simulation-based training
FAST
Initial trauma resuscitation plays a critical role in saving lives and reducing morbidity and mortality from injuries. Effective in-hospital resuscitation requires prompt and coordinated interventions delivered by a skilled healthcare team. However, in low- and middle-income countries (LMICs), the trauma burden remains substantial and preventable trauma deaths continue to be a significant public health concern1.
Preventable trauma mortality is defined as deaths due to injury, which are avoidable if optimal care is delivered. Trauma deaths, to be considered preventable, must satisfy three essential criteria as defined by Chiara et al2. These deaths involve survivable injuries, suboptimal treatment compared to established standards, and a direct or indirect link between treatment errors and patient outcomes. In order to address these avoidable deaths in LMICs, it is crucial to examine the barriers and facilitators of initial in-hospital trauma care and the level of training of the trauma teams, which greatly influences the resuscitation process and provision of care2.
This study, aimed to identify key factors that hinder effective trauma resuscitation and explore potential strategies and interventions in trauma training that can strengthen in-hospital trauma care to enhance outcomes. The purpose of undertaking this study is to guide policymakers, healthcare professionals and educators in developing and implementing effective strategies for initial trauma resuscitation and comprehensive trauma training in India and similar LMIC contexts.
Material & Methods
This study was undertaken by the Transdisciplinary Research, Advocacy, and Implementation Network for Trauma in India (TRAIN Trauma India) consortium between May 2023 to September 2023. In our quest for a comprehensive understanding of trauma resuscitation and training programme challenges and gaps in LMICs, a two-fold approach was employed by combining insights from existing literature through a literature review and a situational assessment survey documenting first-hand experiences of practitioners to inform context-specific solutions.
Literature review
The literature review focused on publications from the last 10 yr (January 2014 to August 2023) from the PubMed database utilizing the population-concept-context framework. This included keywords related to trauma training, such as ‘trauma training’, ‘education’, ‘innovations’, ‘implementation and supervision’, and pairing them with terms denoting ‘challenges’, ‘gaps’, ‘implementation barriers and facilitators’. Additionally, country-specific terms for LMICs were used to ensure comprehensive coverage. The search strategy with the Medical Subject Headings (MeSH) terms is provided as Supplementary Material: Box. The review aimed to extract critical insights from published literature regarding existing LMIC trauma care training programmes focussing on their innovations, implementation challenges, gaps, and potential future steps, forming the foundational knowledge base. Articles that were systematic/scoping reviews and meta-analyses were excluded, and also, articles from high-income countries (HICs) were excluded.
All the selected studies were entered into Rayyan QCRI (https://www.rayyan.ai), an intelligent online platform for systematic review, developed by the Qatar Computing Research Institute. A two-stage screening process was implemented where two reviewers independently screened the articles for inclusion. In case of disagreement, a third reviewer made the final decision. The PRISMA flowchart for inclusion and exclusion process is shown in Figure 1.
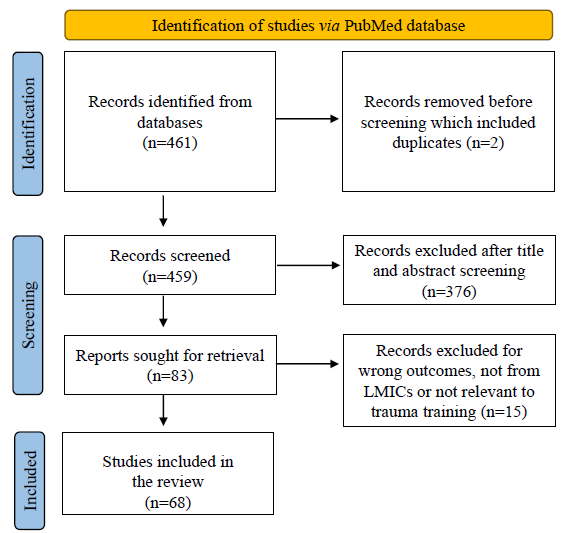
- PRISMA flowchart for inclusion. LMICs, low- and middle-income countries.
Situational assessment survey
This survey was undertaken by the TRAIN-India consortium after procuring an approval by Terna Medical College & Hospital, Navi Mumbai. Institutional Ethics Committee between August 2023 to September 2023. The availability and accessibility of existing trauma training programmes in LMICs and challenges in the wider integration of trauma education into regular clinical/surgical training was evaluated through this survey. The survey was presented as a Google form which was developed based on the initial literature review of relevant articles and weekly discussions with global experts in trauma care. The study tool was disseminated through various social media platforms to the target participants, comprising trauma care providers in LMIC settings involved in initial trauma care.
A structured questionnaire was used for data on experiences, challenges and resource availability in trauma care. Simultaneously, insights into unmet needs and strategies for adopting trauma training programmes in LMICs were sought. The survey encouraged snowball sampling through email and social media to maximise participation. Ethical standards ensuring confidentiality and anonymity were adhered to. A written informed consent was obtained from all study participants as part of the survey.
Results
Literature review
The geographical distribution of the studies included in the initial literature review is depicted in Supplementary Table. Out of the total 68 included articles, most studies (52.9%) were from the African subcontinent.
The studies documented various training programmes with their advantages, innovative strategies used, challenges faced in implementing these programmes and proposed recommendations. Most of the mentioned programmes were documented in academia. About 86.8 per cent of the studies discussed training programmes that were primarily designed for physicians, clinicians, postgraduate trainees (surgery or anaesthesia) and medical students. Low levels of inclusivity were noted, with only a few training courses meant for nurses, paramedical personnel and administrators who had a significant role in the provision of in-hospital trauma care.
The various innovations used in these training programmes included simulation-based training, cascading training model (initial training of local faculty by HIC faculty and future courses conducted by trained local faculty) focussing on local context, use of checklists, videos and slides along with traditional lectures. Table I3-45 depicts a comprehensive review of the studies documenting challenges in implementation, identified gaps and recommendations for future implementation.
| Programme name | Challenges & gaps in implementation | Recommendations |
|---|---|---|
| Primary Trauma Course (PTC)3-12 | Lack of evidence linking training to long-term outcomes, initial funding & cost | Reduction in initial cost, long-term outcome audits, application of cascading model, inclusion as part of academic training |
| Advanced Trauma Life Support (ATLS)1,3,6,12–18 | Lack of trained staff, implementation policy issues, non-availability & expenses of equipment | Combining ATLS with residency training, cost reduction, accessibility & modification to suit all healthcare personnel |
|
Morbidity and Mortality meetings (M & M meetings)19 |
Lack of guideline-based implementation, not mandatory at present | Guideline-based implementation, to be included as a mandatory academic activity (post-graduate curriculum) |
| WHO Emergency Trauma Course (WHO ETC)20-23 | Staff, infrastructure, equipment, expenses for initial training of faculty | Scale-up to national level, use of cascading model for implementation |
| Post-graduate Course in Emergency medicine (PG in EM)24 | Conflict with broad speciality training programmes (orthopaedics & surgery) | 3 yr training course, focus on competency-based medical education |
| Trauma Evaluation and Management (TEAM)1,3,6,12,15,16,25–28 | Focussed Assessment with Sonography for Trauma (FAST) training difficult | Post-test evaluation |
| Sequential Trauma Education Programmes (STEPs)12,29,30 | Inappropriate course organization, lack of evidence to link training to outcomes | Long-term outcome audits |
| Institute for Global Orthopaedics and Traumatology (IGOT) Digital Learning Portal31,32 | Internet connectivity, access to devices, language barriers, limited interactivity & discussion | Expand & evaluate content, increase language accessibility, pre & post-assessments |
| Online Master of Science (MSc) degree in Trauma Sciences by Queen Mary University of London (QMUL)33 | Internet access differences by country | Increase support for students from developing countries & assess the impact of the programme on patient outcomes |
| Collaboration in Higher Education for Nursing and Midwifery in Africa (CHENMA), Mozambique34 | Medical dominance, lack of policies for nursing advancement, lack of postgraduate nursing specialization programmes previously | Establish regulatory nursing authority, invest in nursing advancement, evaluate programme impact on patient outcomes in 5 yr |
| Orthopaedic Trauma Care Specialist (OTCS) residency programme, Haiti12,35 | Funding, developing local faculty, lack of specialised orthopaedic trauma training previously | Expand to other surgical specialties, injury pattern surveillance |
| WHO Basic Emergency Care (BEC) course21,36,37 | Ensuring quality instruction with limited local expertise, long-term knowledge retention, need evaluation of the impact on clinical care & outcomes | Incorporate locally relevant examples, supplies that are available locally in teaching the skills sessions for future iterations of the course, focus on key knowledge gaps, assess long-term knowledge retention & impact patient outcomes |
| Four-day trauma training course at a regional hospital in the Dominican Republic38 | Resource limitations, data collection, no standardized trauma curriculum previously | Longitudinal reinforcement using a longitudinal trauma curriculum may bolster retention, develop a trauma checklist or registry, assess actual clinical practices |
| Pre-deployment training, including a Surgical Readiness Training Exercise (SURGRETE), Honduras39 | Language barriers, funding, low trauma volume during the training period, dedicated space for trauma resuscitations, traditional pre-deployment training lacks trauma volume & realism of deployed setting | Incorporate training in an environment similar to the deployment setting when possible, utilising organic equipment rather than modern hospital anaesthesia equipment, evaluate long-term skill retention after training, cost-effective analysis between SURGRETE and U.S. Army Trauma Training Center (ATTC) |
| TRUE-Bolivia40 | Knowledge gaps, inability to track patient outcomes to assess the programme’s impact on trauma mortality, high course attrition rate, resource constraints, limited long-term evaluation | Refining course content, developing a real-time incident tracking app, aligning didactic and practical sessions, providing first aid kits, enhancing long-term evaluation methods, adopting a Train-the-Trainer model, offering refresher courses, promoting improved participant safety behaviours, sustaining community partnerships, & focusing on low cost & replicability to reduce prehospital trauma mortality. |
| Kampala Advanced Trauma Course (KATC)41,42 | Resource constraints, insufficient trained faculty, infrastructure deficiencies, & expensive databases and simulators. | Assess course effectiveness with trainee follow-up, & improve long-term impact by enhancing infrastructure and training peers. |
| Trauma training Course (TTC)43 | Lack of funding, government support, & human resources, & lack of basic training. | Use simulation-based models as more effective teaching & learning tools. |
| Advanced Trauma Care for Nurses (ATCN)12,44 | Intermittent electrical power & internet connectivity, transportation issues, funding constraints, data limitations for impact measurements & family responsibilities. | Collaborate with established organizations, secure funding for infrastructure, provide ongoing remote education, streamline licensure processes, & ensure program sustainability through local faculty training & certification. |
| Definitive Surgical Trauma Care (DSTC) and National Trauma Management Course (NTMC)45 | Time-consuming setup of animal labs with veterinary ethical certification | Promote the course globally and use its guidelines & publications to define core competencies for residency training & develop curricula for schools of medicine & nursing. |
Situational assessment survey
Out of the 98 reached potential respondents from nine countries, 34 (35%) responses were gathered over one month with responders from India, Belarus, Azerbaijan, Nepal and Pakistan. Most (82.4%) responses were from consultants with 73.5 per cent having more than ten years of clinical experience. Most respondents (52.9%) mentioned a lack of an established trauma training programme in their hospitals. More than half of the respondents were involved in initial trauma resuscitation more than a few times a month. Maximum respondents also faced a lack of clear protocols or guidelines and a lack of training in specific resuscitation and management techniques as the most common challenges in initial patient resuscitation. Figure 2 depicts the challenges in initial trauma resuscitation as documented by survey respondents.
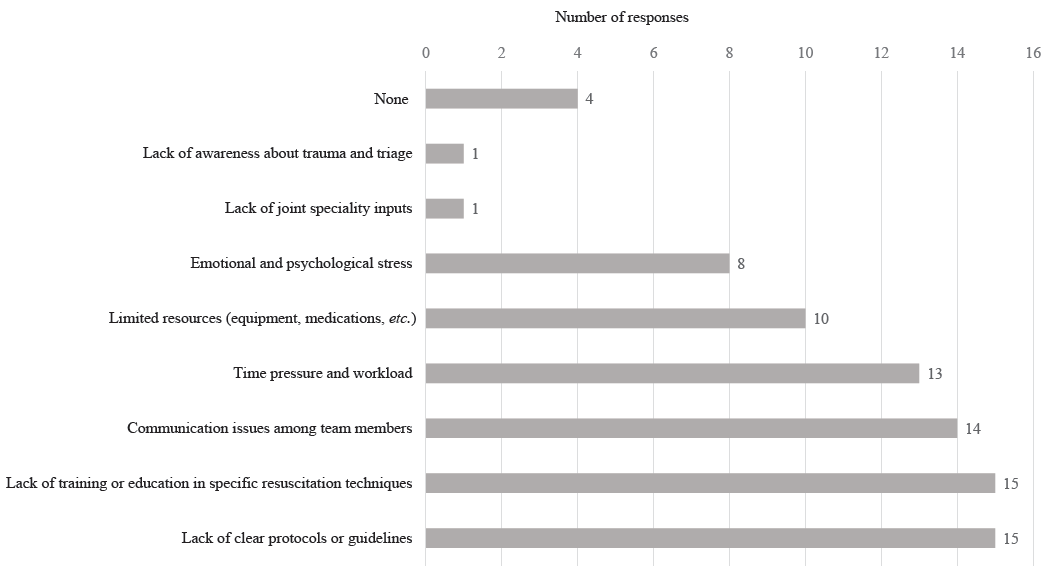
- Bar diagram depicting challenges faced by survey respondents in initial trauma resuscitation.
The improvement strategies proposed by the respondents were hands-on simulation-based training (94.1%), feedback and debriefing sessions after trauma patient resuscitation efforts (70.6%) and access to updated guidelines and protocols (61.8%). Twenty-nine out of 34 (85.3%) respondents expressed the felt need for structured trauma training programmes.
The respondents proposed various measures to be incorporated in trauma training programmes meant for all emergency room employees. Certain specific improvements were highlighted to help implement the protocols envisioned or developed at the commencement of the trauma training. Policy and system development was deemed crucial, necessitating awareness of protocols based on simple decision-making trees, the involvement of administrators in the change implementation, and dedicated training days. For capacity, it was proposed that building trauma training programmes with basic life support, cardiopulmonary resuscitation, extended Focussed Assessment with Sonography in Trauma (e-FAST) for medical interns, postgraduate trainees, nurses and mandatory assignment of emergency room staff be underpinned by regular simulation sessions and context-specific courses. The need for emergency departments to have dedicated and user-friendly structured environments, data registries and scribes for data recording round the clock was emphasised. The enhancement of inter-departmental collaboration with regular morbidity and mortality meetings and the subsidization of training costs were suggested to encourage participation across all staff levels for cohesive learning and service provision. A robust standardisation by a national accreditation and certification process was seen as imperative, with training programmes that are uniform, replicable, context-relevant and reinforced biannually. Financial strategies were recommended to include subsidized training costs and incentives to ensure wide participation, affordability, and accessibility. The maintenance of quality assurance through ongoing reviews, feedback with loop closure exercises and quality improvement (QI) cycles was advocated. Another imperative strategy proposed was to bolster community education and engagement through consistent reinforcements coupled with financial incentives, ensuring a robust framework for sustained participant motivation.
Discussion
Inadequate airway management, fluid resuscitation and haemorrhage control are the leading causes of preventable deaths in India and other LMICs46. The lethality from airway compromise in resource-limited LMIC settings is high, with mortality ranging between 30 and 80 per cent47. Mortality due to haemorrhage in trauma patients is early, mostly within the first three hours of injury48. The lack of effective airway management strategies and measures to control life-threatening haemorrhage have been recognized as a knowledge and capability gap which warrants remediation49.
Patients often face underprepared healthcare systems in LMICs, which lack essential equipment, trained personnel, and standard guidelines compared to HICs when transported for care50. Inadequate training in trauma care using standard protocols by healthcare providers and variations in training seem to be significant barriers to the effective provision of trauma care12. Hence, the key to facilitating improvement in the hospital settings is an immediate focus on trauma education and training initiatives using the multidisciplinary approach, standard QI initiatives, and use of standardized protocols and guidelines for trauma management. The existing challenges could be mitigated by an adequate needs assessment, empowering the emergency care personnel in essential skills, training course standardization with uniform accreditation and provision of appropriate infrastructure and equipment.
Through the multifaceted approach used in this study, the focus remained on a few interventions for the purpose of improving trauma training and enhancing provision of trauma care in low-resource settings. In alignment with this focus, the National Medical Commission (NMC) India has mandated the incorporation of advanced trauma care courses into the curricula for postgraduate students in traumatology and general surgery51. Furthermore, it has directed medical schools to establish simulation labs for training undergraduates and postgraduate students in various skills52. In addition, there are time-tested trauma training courses like Advanced Trauma Life Support (ATLS) and Advanced Trauma Care for Nurses (ATCN), which have collectively trained over 10,000 healthcare professionals through 700 courses in India12,44,53. However, to maintain the sustainability of training, these courses can be provided at subsidized rates by regulatory bodies like the NMC and National Board of Examinations with the addition of specialized trauma training sites. Furthermore, the freely available WHO Guidelines for Essential Trauma Care or Standard Treatment Guidelines for trauma care by the Ministry of Health and Family Welfare may be utilized as the ‘cascading model’ and conducted every six months for the purpose of reinforcements54–58. FAST evaluations should be an integral part of the training of first-line emergency healthcare providers, including clinicians, nurses and allied healthcare workers. Patients with immediate availability of FAST had 64 per cent reduction in the time from presentation to intervention with reduced complications and length of hospital stay59.
Emergency departments (EDs) across the United States have widely adopted the practice of non-radiologists performing emergency ultrasound, considering it a standard of care60. Two studies from a level-one trauma centre in India have documented similar sensitivity of FAST performed by emergency medicine residents as compared to radiology consultants61,62. There remains a significant potential and utility of FAST in the Indian EDs for first-line healthcare providers, wherein radiologists are not always available61-63. FAST is already a component of ATLS training. The only concern is the successful navigation of the ‘Pre-Conception and Pre-Natal Diagnostic Techniques Act’ for using the ultrasound machine. Morbidity and mortality meetings (M & M), crucial for trauma quality improvement, analyze deaths and complications to find preventable factors64. These meetings should be considered as opportunities to identify issues and improve the system, rather than just discussions of negative outcomes.
A crucial step for successful implementation in the discussed context involves the engagement of local faculty and the training of local trainers, fostering longitudinal interactions with the populations they serve65. This can empower local healthcare providers to develop and sustain trauma training programmes that are contextually relevant. Integrating low-cost primary trauma guidelines/courses into the curriculum with regular refresher sessions, supported by necessary infrastructure and technology is essential to ensure effective training both at the urban and rural levels41. Given its significance in trauma patient assessment and management, diversity, equity and inclusivity must be central to trauma education, advocating for multidisciplinary involvement. Implementing low-cost, simulation-based training and utilizing technology for e-learning can significantly enhance the accessibility and quality of trauma training. Finally, collaborative partnerships and knowledge sharing among institutions, countries, and global health organizations are imperative. These collaborations can facilitate the exchange of best practices, resources, and innovations to strengthen the capacity and effectiveness of trauma training in LMICs.
We acknowledge that this study was not without some limitations. The exclusive use of only PubMed for our literature review, which, while extensive, does not capture the breadth of data available in other databases. This limitation may have led to a potential selection bias and a narrower scope of findings. Moreover, the survey component of our research saw a response rate of only 35 per cent, which could affect the generalizability of our results. A higher response rate might have provided a more comprehensive insight into the training needs and experiences of trauma care providers. Snowball survey sampling, while valuable, presents limitations that could be addressed in future studies through focused interviews and facility-based assessments for more robust data. We consider these factors as critical points for future research to build upon, ensuring more inclusive and comprehensive data collection.
Overall in LMICs, the insufficiencies in trauma resuscitation and training programmes pose significant barriers. To summarize, the three pivotal interventions aimed at enhancing trauma care in resource-constrained settings include, offering subsidies for ATLS and ATCN courses and adopting WHO Guidelines for Essential Trauma Care or similar trauma guidelines, employing a cascading training model to equip healthcare workers with the essential skills and knowledge for optimal trauma care, implementing QI processes for continuous learning and system enhancement and incorporating FAST in emergency departments to expedite haemorrhage detection and improve patient outcomes.
Acknowledgment
Authors acknowledge the Transdisciplinary Research, Advocacy, and Implementation Network for Trauma in India (TRAIN Trauma India) for their scientific inputs on methodology and drafting this manuscript.
Financial support & sponsorship
None.
Conflicts of Interest
None.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of AI-assisted technology for assisting in the writing of the manuscript and no images were manipulated using AI.
References
- Preventable trauma deaths: From panel review to population based-studies. World J Emerg Surg. 2006;1:12.
- [CrossRef] [PubMed] [Google Scholar]
- Trauma training in low- and middle-income countries: A scoping review of ATLS alternatives. Afr J Emerg Med. 2022;12:53-60.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Primary trauma care: A training course for healthcare providers in developing countries. J Pak Med Assoc. 2019;69:S82-5.
- [PubMed] [Google Scholar]
- Are primary trauma care (PTC) courses beneficial in low- and middle-income countries - A systematic review. Injury. 2020;51:136-41.
- [CrossRef] [PubMed] [Google Scholar]
- Increasing the use of continuing professional development courses to strengthen trauma care in Ghana. Ghana Med J. 2020;54:197-200.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Do trauma courses change practice? A qualitative review of 20 courses in east, central and southern Africa. Injury. 2017;48:2010-6.
- [CrossRef] [PubMed] [Google Scholar]
- Delivering a sustainable trauma management training programme tailored for low-resource settings in east, central and southern African countries using a cascading course model. Injury. 2016;47:1128-34.
- [CrossRef] [PubMed] [Google Scholar]
- Impact of the primary trauma care course in the Kongo central province of the Democratic Republic of Congo over two years. Injury. 2020;51:235-42.
- [CrossRef] [PubMed] [Google Scholar]
- A multicountry health partnership programme to establish sustainable trauma training in east, central, and southern African countries using a cascading trauma management course model. Lancet. 2015;385:S43.
- [CrossRef] [PubMed] [Google Scholar]
- How useful are primary trauma care courses in sub-Saharan Africa? Injury. 2015;46:1293-8.
- [CrossRef] [PubMed] [Google Scholar]
- Trauma training courses and programs in low- and lower middle-income countries: A scoping review. World J Surg. 2021;45:3543-57.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Does ATLS training work? 10-year follow-up of ATLS India program. J Am Coll Surg. 2021;233:241-8.
- [CrossRef] [PubMed] [Google Scholar]
- Advanced trauma life support training for hospital staff. Cochrane Database Syst Rev. 2014;2014:CD004173.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- A national trauma capacity assessment of Haiti. J Surg Res. 2016;201:126-33.
- [CrossRef] [PubMed] [Google Scholar]
- Combating terror: A new paradigm in student trauma education. J Trauma Acute Care Surg. 2015;78:415-21.
- [CrossRef] [PubMed] [Google Scholar]
- Cost analysis of the Mongolian ATLS© program: A framework for low- and middle-income countries. World J Surg. 2019;43:353-9.
- [CrossRef] [PubMed] [Google Scholar]
- Barriers to accessing ATLS provider course for junior doctors at a major university hospital in South Africa. South Afr J Surg. 2017;55:10-15.
- [PubMed] [Google Scholar]
- Surgical mortality audit-lessons learned in a developing nation. Int Surg. 2015;100:1026-32.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The readiness of emergency and trauma care in low- and middle-income countries: A cross-sectional descriptive study of 42 public hospitals in Albania. Int J Emerg Med. 2016;9:26.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Cost-effectiveness analysis of the multi-strategy WHO emergency care toolkit in regional referral hospitals in Uganda. PloS One. 2022;17:e0279074.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Compliance of district hospitals in the center region of Cameroon with WHO/IATSIC guidelines for the care of the injured: a cross-sectional analysis. World J Surg. 2014;38:2525-33.
- [CrossRef] [PubMed] [Google Scholar]
- Strategic assessment of trauma care capacity in Ghana. World J Surg. 2015;39:2428-40.
- [CrossRef] [PubMed] [Google Scholar]
- The 2014 academic college of emergency experts in India’s education development committee (EDC) white paper on establishing an academic department of emergency medicine in India - Guidelines for staffing, infrastructure, resources, curriculum and training. J Emerg Trauma Shock. 2014;7:196-208.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Implementing the trauma evaluation and management (TEAM) course in Kenya. J Surg Res. 2018;232:107-12.
- [CrossRef] [PubMed] [Google Scholar]
- Trauma evaluation and management TEAM® course for medical students in Pakistan. Pak J Med Sci. 2020;36:1257-62.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Using the “twelve tips for applying change models” for undergraduate medical curriculum reform in Pakistan: Incorporating a new trauma evaluation and management TEAM® course. MedEdPublish (2016). 2022;12:29.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The TEAM (Trauma Evaluation and Management) course: Medical student knowledge gains and retention in the USA versus Ghana. Trauma Surg Acute Care Open. 2019;4:e000287.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Developing sustainable trauma care education in Egypt: Sequential trauma education program, steps to success. J Surg Educ. 2015;72:e29-32.
- [CrossRef] [PubMed] [Google Scholar]
- Impact of implementation of sequential trauma education programs (STEPs) course on missed injuries in emergency polytrauma patients, Ismailia, Egypt. Afr J Emerg Med Rev. 2022;12:89-96.
- [CrossRef] [Google Scholar]
- Novel e-learning platform for orthopaedic training in LMICs: a descriptive review of the IGOT portal. Surg Open Sci. 2023;13:24-6.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Building orthopaedic trauma capacity: IGOT international SMART Course. J Orthop Trauma. 2015;29:S17-9.
- [CrossRef] [PubMed] [Google Scholar]
- Delivering trauma mastery with an international trauma masters. Injury. 2019;50:877-82.
- [CrossRef] [PubMed] [Google Scholar]
- Advancing nursing scholarship: the Mozambique model. Glob Health Action. 2017;10:1351116.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Orthopaedic trauma care specialist program for developing countries. J Orthop Trauma. 2015;29:S26-8.
- [CrossRef] [PubMed] [Google Scholar]
- Results from the implementation of the World Health Organization basic emergency care course in Lagos, Nigeria. Afr J Emerg Med. 2021;11:231-6.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Implementation and outcomes of a comprehensive emergency care curriculum at a low-resource referral hospital in Liberia: a novel approach to application of the WHO basic emergency care toolkit. PloS One. 2023;18:e0282690.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Impact of a focused trauma course on retention of provider skills, knowledge and confidence at a regional hospital in the Dominican Republic. Injury. 2021;52:2526-33.
- [CrossRef] [PubMed] [Google Scholar]
- Conducting pre-deployment training in Honduras: the 240th forward resuscitative surgical team experience. Mil Med. 2022;187:e690-5.
- [CrossRef] [PubMed] [Google Scholar]
- TRUE-Bolivia: trauma responders unifying to empower communities in Santa Cruz, Bolivia. J Surg Res. 2022;273:1-8.
- [CrossRef] [PubMed] [Google Scholar]
- Design, implementation and long-term follow-up of a context specific trauma training course in Uganda: lessons learned and future directions. Am J Surg. 2020;219:263-8.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical practices following train-the-trainer trauma course completion in Uganda: a parallel-convergent mixed-methods study. World J Surg. 2023;47:1399-408.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Trauma training course: innovative teaching models and methods for training health workers in active conflict zones of eastern Myanmar. Int J Emerg Med. 2014;7:46.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Improving trauma care in Africa. J Trauma Nurs. 2017;24:258-60.
- [CrossRef] [PubMed] [Google Scholar]
- International association for trauma surgery and intensive care (IATSIC) presidential address: improving trauma care globally: how is IATSIC Doing? World J Surg. 2016;40:2833-9.
- [CrossRef] [PubMed] [Google Scholar]
- Learning from 2523 trauma deaths in India - opportunities to prevent in-hospital deaths. BMC Health Serv Res. 2017;17:142.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Tracheobronchial injury. Semin Thorac Cardiovasc Surg. 2008;20:52-7.
- [CrossRef] [PubMed] [Google Scholar]
- Outcomes of traumatic hemorrhagic shock and the epidemiology of preventable death from injury. Transfusion (Paris). 2019;59:1423-8.
- [CrossRef] [Google Scholar]
- An international survey of airway management education in 61 countries†. Br J Anaesth. 2020;125:e54-60.
- [CrossRef] [PubMed] [Google Scholar]
- World trauma education: hemorrhage control training for healthcare providers in India. Trauma Surg Acute Care Open. 2019;4:e000263.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Guidelines for competency based PG programs. Available from: https://www.nmc.org.in/information-desk/for-colleges/pg-curricula-2/, accessed on March 1, 2023.
- Public notice. Available from: https://www.nmc.org.in/MCIRest/open/getDocument?path=/Documents/Public/Portal/LatestNews/Public%20notice%20ug.pdf, accessed on March 1, 2023.
- Advanced trauma life support India program. Available from: https://www.atls.in/, accessed on March 1, 2023.
- Guidelines for trauma quality improvement programmes. Available from: https://iris.who.int/bitstream/handle/10665/44061/9789241597746_eng.pdf?sequence=1, accessed on March 1, 2023.
- Guidelines for essential trauma care. Available from: https://iris.who.int/bitstream/handle/10665/42565/9241546409_eng.pdf?sequence=1, accessed on March 1, 2023.
- Emergency and injury care at district hospitals in India-A report of current status on country level assessment. Available from: https://www.niti.gov.in/sites/default/files/2023-02/AIIMS_STUDY_2_0.pdf, accessed on March 1, 2023
- Standard treatment guidelines major trauma. Available from: http://clinicalestablishments.gov.in/WriteReadData/9451.pdf, accessed on March 1, 2023.
- A national trauma care system: Integrating military and civilian trauma systems to achieve zero preventable deaths after injury. Available from: http://www.nap.edu/catalog/23511, accessed on March 1, 2023.
- Randomized controlled clinical trial of point-of-care, limited ultrasonography for trauma in the emergency department: the first sonography outcomes assessment program trial. Ann Emerg Med. 2006;48:227-35.
- [CrossRef] [PubMed] [Google Scholar]
- Guiding emergency treatment with extended focused assessment with sonography in trauma by emergency responders (GET eFASTER) Air Med J. 2023;42:42-7.
- [CrossRef] [PubMed] [Google Scholar]
- To determine the accuracy of focused assessment with sonography for trauma done by nonradiologists and its comparative analysis with radiologists in emergency department of a level 1 trauma center of India. J Emerg Trauma Shock. 2013;6:42-6.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Accuracy of extended focused assessment with sonography in trauma (e-FAST) performed by emergency medicine residents in a level one tertiary center of India. Adv J Emerg Med. 2018;2:e15.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Removing barriers to emergency medicine point-of-care ultrasound: Illustrated by a roadmap for emergency medicine point-of-care ultrasound expansion in India. J Emerg Trauma Shock. 2023;16:116-26.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Mortality and morbidity reviews practice guide – working version. Available from: https://www.scottishacademy.org.uk/sites/default/files/consultations/SMMP%20Practice%20Guide_Workshop%200318.pdf, accessed on March 1, 2023.
- Assessing the impact of the trauma team training program in Tanzania. J Trauma. 2008;65:879-83.
- [CrossRef] [PubMed] [Google Scholar]






