Translate this page into:
Recommendations for India-specific multiple micronutrient supplement through expert consultation
For correspondence: Dr Priyanka Gupta Bansal, Division of Reproductive, Child Health & Nutrition, Indian Council of Medical Research, New Delhi 110 029, India e-mail: priyankaicmr@gmail.com
-
Received: ,
Abstract
Background & objectives
Reducing maternal anaemia and enhancing feto-maternal health to achieve desired birth outcomes is a major health concern in India. Micronutrient deficiencies during pregnancy may impact fetal growth and neonatal outcomes. There is increasing interest in using multiple micronutrient supplement (MMS) during pregnancy. However, the World Health Organization (WHO) recommends use of MMS containing Iron and Folic Acid (IFA) in the context of “rigorous research”. Against this backdrop, an Indian Council of Medical Research (ICMR)-led MMS design expert group met over six months to review the evidence and decide on the formulation of an India-specific MMS supplement for pregnant mothers for potential use in a research setting.
Methods
The India-MMS design expert group conducted a series of meetings to assess the available evidence regarding the prevalence of micronutrient deficiencies in pregnant women in India, the health benefits of supplementing with different micronutrients during pregnancy, as well as nutrient interactions within the MMS formulation. Based on these considerations, the expert group reached a consensus on the composition of the MMS tailored for pregnant women in India.
Results
The India-specific MMS formulation includes five minerals and 10 vitamins, similar to the United Nations International Multiple Micronutrient Antenatal Preparation (UNIMMAP) composition. However, the quantities of all vitamins and minerals except Zinc, Vitamin E, and Vitamin B6 differ.
Interpretation & conclusions
This report provides an overview of the process adopted, the evidence evaluated, and the conclusions from the expert working group meetings to finalize an MMS supplement in pregnancy for the Indian context to be used in a research setting.
Keywords
Multiple micronutrient supplements
micronutrient deficiency
maternal health
neonatal outcomes
maternal anaemia
Routine antenatal iron-folic acid (IFA) supplementation, containing 30-60 mg of elemental iron and 400 µg of folic acid, is recommended by the World Health Organization (WHO) to prevent maternal anaemia in pregnant women. According to the WHO, 60 mg of iron is preferred in settings where anaemia is a major health problem1. India started IFA supplementation (containing 60 mg of elemental iron and 500 µg of folic acid) to all pregnant women as a component of antenatal care in 19732, which evolved over the years to the present-day Anaemia Mukt (free) Bharat programme3. Anaemia during pregnancy has deleterious consequences for maternal and fetal/infant outcomes, including increased risk of postpartum haemorrhage, preeclampsia, preterm birth, low birth weight, small-for-gestational-age, stillbirth, and neonatal and perinatal death4. Interventions to reduce maternal anaemia and improving feto-maternal health and birth outcomes remain an important public health priority in India. Widely prevalent micronutrient deficiencies during pregnancy may affect fetal growth, birth and neonatal outcomes. Therefore, antenatal micronutrient supplementation has been speculated as a potential intervention for better birth outcomes and child survival. The national programmes in India, to date, have relied heavily on IFA supplementation for pregnant mothers and other age groups2,3. The United Nations International Multiple Micronutrient Antenatal Preparation (UNIMMAP) was developed in 1999 in response to the recognized need for improved antenatal care and addressing maternal nutritional deficiencies through comprehensive micronutrient supplementation during pregnancy5. Experts debate the suitability of a globally standardized multiple micronutrient supplement (MMS) like UNIMMAP, as different population groups have varying nutrient deficiencies due to differences in dietary patterns. Recognizing the need for an India-specific MMS, especially for pregnant women, the Indian Council of Medical Research (ICMR)-led India-MMS design expert group finalized the composition of an India- Multiple Micronutrient Supplement (India-MMS) after a series of meetings over six months. This composition is contextualized to local needs based on available evidence. This document delineates the systematic process adopted to arrive at the formulation of India-MMS.
Constitution of expert committee
An expert committee comprising 15 members with expertise in pharmacology, gynaecology, paediatrics, physiology, epidemiology, food technology, and nutrition was formed to meticulously examine evidence and propose a tailored composition for an MMS specific to pregnant Indian women. The committee convened four meetings, with the first coordination meeting held on April 27, 2023, at ICMR, New Delhi, the focus of which was on reviewing the evolution, efficacy, and rationale for using UNIMMAP in low- and middle- income countries (LMICs). The meeting also delved into global evidence on MMS and analyzed data regarding micronutrient status during pregnancy in India and other LMICs. Two additional meetings took place on June 19 and September 6, 2023. During these sessions, the committee examined matters related to micronutrient deficiencies, recommended dietary allowances, and interactions among constituents for the formulation of the India-specific MMS. In the fourth and final consultation on September 6, 2023, the committee finalized the dosage of various vitamins and minerals in the India-specific MMS. This ensured a well-informed and evidence-based approach in determining the optimal composition for the India-specific MMS formulation. The issues discussed and considered by the expert group and the justification for the inclusion and the dosages of various micronutrients are detailed below.
Multiple micronutrient supplementations during pregnancy
Micronutrient deficiencies are common among women of reproductive age, particularly in LMIC where dietary diversity is often lacking6. There is limited evidence, primarily from small-scale studies7, on the prevalence of micronutrient deficiencies in India during pregnancy. Over time, there has been increasing advocacy for incorporating MMS in place of IFA in routine antenatal care, especially in LMICs8-10. United Nations International Children’s Emergency Fund (UNICEF), the United Nations (UN), and WHO collaboratively developed an MMS for pregnant women named UNIMMAP, which contains 10 vitamins and five minerals details of which are available in the public domain11. Research suggests that MMS may mitigate the risk of adverse pregnancy outcomes such as low birth weight, small for gestational age, stillbirth, and preterm birth, particularly among anaemic and underweight women. However, little to no effect on mortality outcomes, including maternal, neonatal, perinatal, and infant mortality, and on maternal anaemia or haemoglobin status was reported10,12-15. However, WHO has taken a cautious stance on this matter, changing its recommendation from “not recommended” in the year 2016 to “recommended in the context of rigorous research”16 in the year 2020. Thus, the transition from IFA to MMS requires weighing the risks of supplementary nutrition in the daily routine of pregnant women. Given the growing attention towards investigating the potential benefits of MMS on birth outcomes and maternal anaemia, there is a need to develop a tailored MMS supplement for Indian women. This would allow researchers to primarily test its possible efficacy in future studies conducted in India.
Need for a separate country-specific MMS formulation
Opinions differ on the uniform acceptability and utility of a globally standardized MMS composition like UNIMMAP, because patterns of nutrient deficiencies vary in different population groups17 due to inherent differences in nutrient intakes and the nutritional requirements18. Moreover, the nutritional needs of Indian pregnant women differ due to variations in gestational weight gain. Studies have indicated that gestational weight gain (GWG) tends to be lower than the recommended guidelines in Indian women19,20. While the Institute of Medicine (IOM) 200921 suggests a GWG of 11.5-16 kg for women with a body mass index (BMI) between 18.5-22.9 kg/m2 (Asian category), a systematic review20 on Indian pregnant women found an average GWG of 10.08 kg. Globally, the pooled mean GWG is reported at 13.4 kg, with Asian populations averaging 11.4 kg22. A recent publication from the Garbh-Ini cohort19 found that Indian women’s GWG fell significantly below the INTERGROWTH-21st reference23, with around 26 per cent below the 10th centile at 18-20 wk of gestation, increasing to 45 per cent at delivery. Therefore, a careful examination of specific micronutrient deficiencies prevalent in Indian pregnant women is required to contextualize the MMS and maximize the expected benefits, particularly in improving maternal and birth outcomes. The UNIMMAP composition is based on the US population’s recommended dietary allowances (RDA); some differences are observed between these and ICMR-National Institute of Nutrition (ICMR-NIN), Hyderabad RDA for pregnant women18. The experts opined that a suitable formulation should be designed after a comprehensive mapping of nutritional deficiencies based on available dietary intake and biochemical nutritional deficiency data in pregnant women from India.
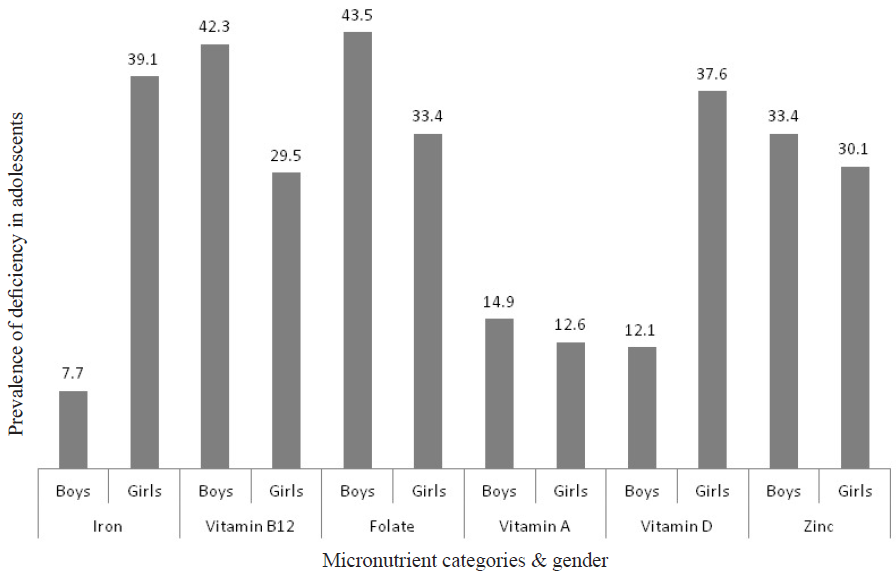
Evidence presented on micronutrient deficiency status in India
Data from national surveys and independent studies on pregnant Indian women (published and unpublished, including personal communication) were reviewed to gauge micronutrient deficiencies based on biomarkers (Table I-IV7,24-44 and Figure45). The review was broadened to include studies from India and adjacent South Asian countries due to a paucity of data on some micronutrient deficiencies. Additionally, available data on the dietary intake of micronutrients during pregnancy in Indian women was compiled and evaluated (Table V)46,47. Other studies on the dietary intake of pregnant women revealed dietary inadequacies in terms of diet diversification and optimal intake of nutrient-rich foods, especially for iron and calcium48,49.
| Analyte | Global clinical cut-off | Prevalence of deficiency during pregnancy (%) (n; cut off) | Authors & year |
|---|---|---|---|
| Vitamin D (ng/ml) | <12 ng/ml |
63.5 (n=1931; ∼10-25 ng/ml), 74*, 32 (range 34-96%; n=4088) |
Bhatnagar et al24, 2019 Taneja et al25, 2020 Jeykumar et al26, 2021 |
| Ferritin (ng/ml) |
(i) <15 ng/ml (ii) Proportion deficient (CRP ≤5 mg/l & Ferritin <15 ng/ml or CRP >5 mg/l & Ferritin <70 ng/ml) |
73.4 (n=283), 67.7 (<12 ng/ml) 52.5 (n=1935)**, 52, 31 (ferritin <15 ng/ml; n=1132) |
Pathak et al7, 2004 Bhatnagar et al24, 2019 Taneja et al25, 2020 Nair et al27, 2023 |
| Vitamin B12 (pg/ml) | <200 pg/ml |
49*, 51, 55 (n=120) 40-70 (n=4000) |
Finkelstein et al28, 2017 Taneja et al25, 2020 Barney et al29, 2020 Behere et al30, 2021 |
| Zinc (mcg/dl) | <66 µg/dl |
73.5 (<70 µg/dl; n=283), 45.1 (n=1835)**, 35* |
Pathak et al31, 2008 Bhatnagar et al24, 2019 Taneja et al25, 2020 |
| Folate (ng/ml) | <4 ng/ml |
26.3 (<3 ng/ml; n=283), 24.3 (<3 ng/ml), 20.7(3–5.9 ng/ml; n=584), 4.5 (n=1979)**, 15* |
Pathak et al7, 2004 Bhide et al32, 2019 Bhatnagar et al24, 2019 Taneja et al25, 2020 |
| Vitamin B6 | <20 nmol/l | 10.4 (n=230) | Deepa et al33, 2023 |
| Vitamin B1 | Whole-blood Thiamine Diphosphate (ThDp) <74 nmol/l | 38.2 (n=492) | Kareem et al34, 2023 |
| Copper | <80 mg/dl | 2.7 (n=283) | Pathak et al7, 2004 |
| Iodine | 4.67 mIU/l |
6.4 (n=283) 14.4 (n=139) |
Pathak et al7, 2004 Gopal et al35, 2022 |
| Vitamin A | <20 μg/dl | 32.1 | Meshram et al36, 2022 |
| Micronutrient |
Pre-conception & pregnancy (Group A) n=248 |
Pre-conception only (Group B) n=247 |
Pregnancy only (Group C) n=250 |
Routine care (Group D) n=250 |
|---|---|---|---|---|
| Vitamin A, mg/l | ||||
| Mean (±SD) | 0.48 (0.21) | 0.39 (0.18) | 0.48 (0.22) | 0.36 (0.2) |
| Proportion deficient (%) (<0.196 mg/l) | 12 (5.8) | 23 (11.2) | 13 (6) | 44 (20.7) |
| Vitamin D-3 (ng/ml) | ||||
| Mean (SD) | 17.0 (9.7) | 8.8 (6.5) | 18.7 (11.5) | 9.8 (7.7) |
| Proportion deficient (<12 ng/ml) | 89 (35.9) | 196 (79.4) | 89 (35.6) | 189 (75.6) |
| Vitamin B12 (pg/ml) | ||||
| Mean (SD) | 236.7 (153.6) | 212.6 (175.5) | 248.9 (232) | 218.4 (214.5) |
| Proportion deficient (%) (<203 pg/ml) | 127 (51.2) | 158 (64.0) | 140 (56) | 158 (63.2) |
| Zinc (µg/dl) | ||||
| Mean (SD) | 92.9 (84) | 96.2 (67.5) | 90.1 (67.1) | 88.4 (72) |
| Proportion deficient (%) (<66 µg/dl) | 126 (50.8) | 100 (40.5) | 114 (45.8) | 124 (49.6) |
| Ferritin (ng/mL) | ||||
| Mean (SD) | 46.0 (52.5) | 30.5 (35.2) | 50.1 (65.9) | 29.8 (33.5) |
|
Proportion deficient (%) (CRP ≤5 mg/l & Ferritin <15 ng/ml or CRP >5 mg/l & Ferritin <70 ng/ml) |
90 (36.3) | 121 (49) | 94 (37.6) | 125 (50) |
| Folate (ng/ml) | ||||
| Mean (SD) | 11.8 (5.9) | 8.1 (5.8) | 12.4 (5.9) | 7.8 (5.6) |
| Proportion deficient (<4 ng/ml) | 38 (15.3) | 82 (33.2) | 29 (11.6) | 81 (32.4) |
| Selenium (ug/l) | ||||
| Mean (SD) | 123.8 (18.5) | 121.9 (18.1) | 126.5 (17) | 122.9 (18.3) |
| Proportion deficient (%) (<85 ug/l) | 1(0.4) | 4 (1.7) | 1 (0.4) | 3 (1.3) |
SD, standard deviation. Source: ref 25
| Micronutrients | Age group | Prevalence (95 % CI) | Micronutrients | Age group | Prevalence (95 % CI) |
|---|---|---|---|---|---|
| Vitamin A | Pooled | 19 (9, 29) | Iodine | Pooled | 17 (7, 26) |
| <18 yr (n=3384) | 19 (10,28) | <18 yr (n=2067) | 11 (5,17) | ||
| >18 yr (n=165224) | 13 (0, 30) | >18 yr (n= 3545) | 12 (6, 17) | ||
| Non-specific (n=735) | 28 (0, 59) | Non-specific (n=6682) | 59 (0, 100) | ||
| Vitamin D | Pooled | 61 (56, 65) | Folate | Pooled | 37 (27, 46) |
| <18 yr (n=10969) | 60 (51,69) | <18 yr (n=2689) | 39 (22, 57) | ||
| >18 yr (n= 11755) | 60 (53, 67) | >18 yr (n=949) | 41 (24, 58) | ||
| Non-specific (n=56786) | 63 (55, 70) | Non-specific (n=84) | 25 (12, 38) | ||
| Iron | Pooled | 54 (49,59) | Vitamin B12 | Pooled | 53 (41, 64) |
| <18 yr (10541) | 55 (42,68) | <18 yr (n=2542) | 57 (25, 89) | ||
| Adults (148339) | 53 (42,65) | >18 yr (n=4008) | 48 (35, 62) | ||
| Pregnant women (n=449215) | 61 (50,72) | Non-specific (n=235) | 68 (38, 98) | ||
| Non-specific (n=225442) | 49 (39,59) |
| Author | Region & sample size | Time point | Prevalence of deficiency during pregnancy |
|---|---|---|---|
| Pathak et al37 |
Haryana (rural – north India) n=283 |
≥28 wk pregnancy |
74% had B12 deficiency 68% had Iron deficiency 26% had folate deficiency 16% had concomitant deficiencies of iron, folate, & vitamin B12 |
| Krishnaveni et al38 |
Mysore (south India) n=774 |
30 wk gestation |
43% B12 deficiency 4% Folate deficiency |
| Yajnik et al39 |
Pune (rural – west India) n=600 |
18 & 28 wk pregnancy |
60% B12 deficiency (in 18 wk) 70% had B12 deficiency (in 28 wk) 1% had folate deficiency |
| Katre et al40 | Pune (rural & urban) n=163 | 17 wk pregnancy |
80% rural women had B12 deficiency 65% urban women had B12 deficiency |
|
Finkelstein et al28 Samuel et al41 |
Bengaluru n=366 |
≤14 wk of gestation & in 2nd & 3rd trimester |
51% had B12 deficiency 22% had low erythrocyte folate |
| Gadgil et al 42 |
Pune (hospital based) n=50 |
36 wk of gestation |
35% women had B12 deficiency 82% had high folate concentration (above the range of 3–12 ng/ml) |
| Wadhwani et al43 | Pune (hospital based sample) n=109, a longitudinal study | At 16-20 wk pregnancy, at 28-30 wk & at the time of labour |
22, 32 & 42%, respectively had B12 deficiency at the 3time points (<150 pg/ml) 47, 56 & 62%, respectively had folate deficiency at 3 time points (<10 ng/ml) |
| Kaushal et al44 |
Himachal Pradesh cross-sectional hospital-based study n=172 |
antenatal women attending the outpatient |
49% had Vitamin B12 deficiency 34% had Folate deficiency 50% had Iron deficiency |
| Micronutrients | Urban (n=326) | Rural (n=421) | Nutrient requirement | Gap (urban) | Gap (rural) | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Median | IQR | Median | IQR | EAR | RDA | EAR- Median (Urban) | RDA - Median (Urban) | EAR-Median | RDA- (Median | |
| Iron, mg | 11.3 | 8.6, 15 | 11 | 7.6, 16.4 | 21 | 27 | 9.7 | 15.7 | 10 | 16 |
| Zinc, mg | 7 | 5.5, 9.3 | 6.8 | 5.1, 8.9 | 12 | 14.5 | 5 | 7 | 5.2 | 7.7 |
| Calcium, mg | 319.8 | 201.9, 484.3 | 334 | 177.6, 456.4 | 800 | 1000 | 480 | 680 | 466 | 666 |
| Vitamin A, µg | 105.9 | 48.9, 214.9 | 124 | 61.5, 511.6 | 406 | 900 | 300 | 794 | 282 | 776 |
| Vitamin C, mg | 47.3 | 25.2, 74.3 | 24.9 | 12.5, 47.9 | 65 | 80 | 18 | 33 | 40.1 | 55.1 |
| Thiamin, mg (B1) | 1 | 0.8, 1.3 | 1.1 | 0.8, 1.5 | 1.6 | 2 | 0.6 | 1 | 0.5 | 0.9 |
| Riboflavin, mg (B2) | 0.6 | 0.5, 0.8 | 0.7 | 0.5, 0.9 | 2.3 | 2.7 | 1.7 | 2.1 | 1.6 | 2 |
| Niacin (B3), mg | 8.6 | 6.8, 11 | 12.9 | 9, 16.4 | 14 | 16 | 5 | 7 | 1.1 | 3.1 |
| Dietary folate, µg | 167 | 127, 235.3 | 108.6 | 72.7, 154.4 | 288 | 342 | 121 | 175 | 179.4 | 233 |
EAR, estimated average requirement; RDA, recommended dietary allowance; IQR, inter-quartile range
Justification for the proposed doses of various micronutrients in the India-specific MMS
Recommendations were made regarding each of the micronutrients as listed in the UNIMMAP on whether to include or exclude any of these from the India-MMS formulation. The nutrient requirements for pregnant women are defined using two key metrics: the Estimated Average Requirement (EAR) and the RDA. The EAR represents the average requirement of a population subgroup, while the RDA corresponds to the 97.5th percentile of the requirement. These metrics take into account various factors affecting nutritional needs during pregnancy, including weight gain, higher metabolic demands due to maternal tissue expansion, additional requirements for the growing baby, and nutrient storage requirements for the mother. It is important to note that these levels are applicable to help maintain the balance of nutrients in a “healthy individual” and are not intended for correcting deficiencies over a short period of time. When biomarker inadequacy and intake gaps are lower, it is considered that one EAR of nutrients would be adequate. However, to address higher gaps in intake and prevalence of micronutrient biomarker insufficiency in pregnancy, the micronutrients need to be provided at higher doses, exceeding the requirement for more than 97.5 per cent of the population (RDA)18,50. Therefore, 1.5 times the RDA levels may be used for these nutrients. However, it is important to exercise caution to prevent the consumption of excessive amounts of additional nutrients daily that surpass the tolerable upper limit (TUL) of the nutrient. This is crucial as exceeding the TUL may potentially lead to health risks. It is worth noting that the TUL values are established based on long-term intake considerations and are not relevant when intention is to treat in short term. These values hold true for healthy people with good baseline micronutrient status, which is not the case for women residing in LMICs50. In view of the points examined above, the experts decided that for micronutrients with a high prevalence of deficiency (above 30%), the supplemental dose of 1.5 times the RDA should be used in the Indian formulation of MMS. Since deficiencies of iron, folate, vitamin D, and vitamin B12 are widespread with higher than 30 per cent prevalence, a dose equivalent to 1.5 times the RDA is included in the proposed formulation. For nutrients where the prevalence of deficiency is less than 30 per cent, it was decided to use a dose equivalent to one EAR, which refers to the average requirement for pregnant women. For copper, selenium, and vitamin E, a dose equal to Adequate Intake (AI) is recommended since EAR values are not available for these nutrients. The committee decided that a micronutrient from the UNIMMAP list will be excluded from the Indian MMS formulation only in case of demonstrated harmful effects of that particular nutrient. It was also decided that if there is a known interaction between certain micronutrients, their proportions in the MMS formulation will be suitably modified to achieve a favourable impact. In addition, the expert committee discussed the inclusion of iron salt in the supplement. Given the similar iron content and relative bioavailability as ferrous sulphate and the expert committee recommended including ferrous fumarate in the India-specific MMS51 due to its better sensory properties. The final proposed India-specific MMS supplement is outlined in Table VI.
| Nutrient | India-MMS | Rationale | UNIMMAP |
|---|---|---|---|
| Iron (mg) | 40 | 1.5 RDA | 30 |
| Folate (µg) | 500 | 1.5 RDA | 360 |
| Vitamin A (µg) | 400 | EAR | 800 |
| Vitamin C (mg) | 65 | EAR | 70 |
| Vitamin D (IU) | 400 | 1.5 RDA@ | 200 |
| Thiamine (mg) | 1.6 | EAR | 1.4 |
| Riboflavin (mg) | 2.3 | EAR | 1.4 |
| Niacin (mg) | 11 | EAR | 18 |
| Vitamin B-12 (µg) | 4 | 1.5 RDA | 2.6 |
| Zinc (mg) | 15 | RDA | 15 |
| Iodine (µg) | 160 | EAR | 150 |
| Vitamin E (mg) | 10 | AI | 10 |
| Vitamin B-6 (mg) | 1.9 | EAR | 1.9 |
| Copper (mg) | 1.7 | AI | 2 |
| Selenium (µg) | 40 | AI | 65 |
Iron at 40 mg/day was considered adequate for the prevention of anaemia. This dose is lower than that used in the IFA tablet (60 mg/day) because the MMS contains other nutrients, including vitamin C, vitamin A, vitamin B12, and riboflavin, which are known to increase the absorption and utilization of iron52,53. Moreover, lower iron content may improve the compliance due to fewer side effects15,54.
The committee deliberated on the optimal dosage and form of vitamin D for supplementation. Given the widespread vitamin D deficiency in Indian women, a dosage of 1.5 times the RDA, equivalent to 900 International Units (IU), was initially considered for the India-specific MMS. However, it was noted that pregnant women already receive 250 IU of vitamin D3 twice daily and calcium supplements from the 14th week of pregnancy until six months postpartum, following current guidelines. Consequently, the decision was made to modify the vitamin D dosage in the India-specific MMS to 400 IU. This adjustment ensures that the total dose of vitamin D from both the MMS and the calcium and vitamin D3 supplementation will add up to approximately 900 IU, 1.5 times the RDA and well below the TUL of 4000 IU. Additionally, the committee considered an unpublished study conducted at St. John’s Research Institute, Bengaluru, Karnataka, which found that over 70 per cent of women exhibited a vitamin D deficiency, and supplementation of up to 800 IU per day had no adverse effects on the participants (through personal communication). Further, concerning chemical form, experts advocated for the inclusion of vitamin D3 (Cholecalciferol) due to evidence supporting its superior effectiveness in raising serum 25(OH)D levels compared to equimolar vitamin D2 (Ergocalciferol)26,55,56.
Interactions of two micronutrients, vitamin C and zinc, with iron were discussed. Experts considered whether increasing the dose of vitamin C to 120 mg (1.5 times the RDA) is needed to enhance iron bioavailability and, secondly, an appropriate dose of zinc to maintain the optimal iron-zinc ratio. It was recommended that a dose of ascorbic acid equivalent to the EAR (65 mg) be used, as the purpose here is to provide vitamin C to meet physiological requirements. It may also increase iron absorption when combined with iron. Similarly, the proposed dose of 15 mg of zinc (1 RDA) in the MMS formulation would result in an Fe/Zn molar ratio of approximately 3 and would not negatively impact zinc and/or iron absorption based on published studies57-59.
Prophylaxis and treatment
Experts concluded that for pregnant women, one MMS tablet or capsule can be used as prophylaxis instead of an IFA tablet in a research setting. In cases of mild or moderate anaemia, the MMS will need to be supplemented with an additional IFA tablet.
The widespread prevalence of micronutrient deficiency and the increasing focus on MMS supplementation during pregnancy underscore the critical need for comprehensive research on the possible effects of MMS supplementation on pregnancy outcomes and maternal anaemia. This report details the methodology and rationale behind formulating an India-specific MMS specifically designed to facilitate research endeavours for pregnancy.
Acknowledgment
Authors acknowledge Drs Nitin Kumar Singhal (Scientist, Department of Food Science and Technology, National Agri-Food Biotechnology Institute, Mohali), Sadhna Joshi (Nutritional Medicine Centre, BVP Deemed University, Pune), Aditi Apte (Clinical Pharmacologist, KEM Research Centre, Pune), A Ruckmani (Former Professor and Head, Department of Pharmacology, Chettinad Hospital & Research Institute, Tamil Nadu), Shantaraman Kalyanaraman (Professor, Pathology, Tirunelveli Medical College, Tamil Nadu), Ashish Bavdekar (Acting Director, Department of Pediatrics, Consultant Pediatric Gastroenterologist, KEM Hospital), Shailaja Sopory (Principal Scientist II) and Lovejeet Kaur (Junior Research Scientist), Translational Health Science and Technology Institute, Faridabad for their valuable scientific inputs. Special thanks to Drs Vikas Shukla (Project Scientist) and Vani Kandpal (Consultant), India Council of Medical research, New Delhi for their help in the preparation of the manuscript.
Disclaimer
This guidance from ICMR regarding the composition of MMS for potential research trials in India is not an endorsement or explicit recommendation for its use during pregnancy; rather, it serves as a framework for researchers considering its use in trials within India.
Declaration
Some experts assumed the role of authors due to their extensive involvement and direct contribution to the manuscript’s content. While still valuable contributors, others were acknowledged for their significant input without assuming the authorship role. Relevant experts were duly notified regarding the acknowledgement in the manuscript for their consultative role.
Financial support & sponsorship
None.
Conflicts of Interest
None.
Use of Artificial Intelligence (AI)-Assisted Technology for manuscript preparation
The authors confirm that there was no use of AI-assisted technology for assisting in the writing of the manuscript and no images were manipulated using AI.
References
- WHO recommendations on antenatal care for a positive pregnancy experience. Available from: https://www.who.int/publications-detail-redirect/9789241549912, accessed on April 26, 2024.
- Prevention & management of anaemia in pregnancy: Multi-pronged integrated interventions may pay rich dividends. Indian J Med Res. 2021;154:12-5.
- [Google Scholar]
- Anaemia Mukt Bharat. Available from: https://nhm.gov.in/index1.php?lang=1&level=3 &sublinkid=1448&lid=797, accessed on April 26, 2021.
- Maternal haemoglobin concentrations across pregnancy and maternal and child health: A systematic review and meta-analysis. Ann N Y Acad Sci. 2019;1450:47-68.
- [Google Scholar]
- Expert consensus on an open‐access United Nations International Multiple Micronutrient Antenatal Preparation–multiple micronutrient supplement product specification. Ann N Y Acad Sci. 2020;1470:3-13.
- [Google Scholar]
- Micronutrient’s deficiency in India: a systematic review and meta-analysis. J Nutr Sci. 2021;10:e110.
- [Google Scholar]
- Prevalence of multiple micronutrient deficiencies amongst pregnant women in a rural area of Haryana. Indian J Pediatr. 2004;71:1007-14.
- [Google Scholar]
- UNIMMAP MMS for National Health Systems: Considerations for Developing a Supply Strategy. Nov 2022. Available from: https://impekacdn.s3.us-east-2.amazonaws.com/hmhbconsortium.org/content/user_files/2023/01/04072538/FINAL-Kirk_UNIMMAP_MMS_SupplyPaper_Digital.pdf, accessed on April 26, 2024.
- Multiple Micronutrient Supplementation: An approach to improving the quality of nutrition care for mothers and preventing low birthweight. Available from: https://www.unicef.org/media/123271/file#:∼:text=SUPPLEMENTS%20ARE%20SAFE%20AND%20EFFECTIVE,nutritional%20status%20of%20pregnant%20women, accessed on April 26, 2024.
- Multiple‐micronutrient supplementation for women during pregnancy. Cochrane Database Syst Rev. 2019;3:CD004905.
- [Google Scholar]
- Composition of a multi- micronutrient supplement to be used in pilot programmes among pregnant women in developing countries: report of a (UNICEF), World Health Organization (WHO) and United Nations University workshop. Available from: https://www.who.int/publications/i/item/composition-of-a-multi-micronutrient-supplement-to-be-used-in-pilot-programmes-among-pregnant-women-in-developing-countries--report-of-a-united-nations-children-s-fund-(-unicef)---world-health-organization-(-who)--and-united-nations-university-workshop, accessed on April 26, 2024.
- Vitamin and mineral supplementation during pregnancy on maternal, birth, child health and development outcomes in low- and middle-income countries: A systematic review and meta-analysis. Nutrients. 2020;12:491.
- [Google Scholar]
- Impact of small‐quantity lipid‐based nutrient supplement on hemoglobin, iron status and biomarkers of inflammation in pregnant Ghanaian women. Matern Child Nutr. 2016;13:e12262.
- [Google Scholar]
- Effects of lipid‐based nutrient supplements or multiple micronutrient supplements compared with iron and folic acid supplements during pregnancy on maternal haemoglobin and iron status. Matern Child Nutr. 2018;14:e12640.
- [Google Scholar]
- Multiple micronutrient supplements versus iron-folic acid supplements and maternal anemia outcomes: An iron dose analysis. Ann N Y Acad Sci. 2022;1512:114-25.
- [Google Scholar]
- WHO recommendations on antenatal nutrition: An update on multiple micronutrient supplements. BMJ Glob Health. 2020;5:e003375.
- [Google Scholar]
- Precision in prescription: Multiple micronutrient supplements in pregnancy. Lancet Glob Health. 2022;10:e780-1.
- [Google Scholar]
- Nutrients Requirements for Indian. A Report of the Expert Group. 2020. Available from: https://www.im4change.org/upload/files/RDA_short_report%281%29.pdf, accessed on August 16, 2024.
- Gestational weight gain trajectories in GARBH-Ini pregnancy cohort in North India and a comparative analysis with global references. Eur J Clin Nutr. 2022;76:855-62.
- [Google Scholar]
- Burden of excessive gestational weight gain and postpartum weight retention among Indian women - A systematic review and meta-analysis. Clin Epidemiol Glob Health. 2023;23:101364.
- [Google Scholar]
- Rasmussen KM, Yaktine AL, eds. Weight gain during pregnancy. Washington (DC): National Academies Press (US); 2009.
- Post-partum weight retention in women in Asia: A systematic review. Obes Rev. 2011;12:770-80.
- [Google Scholar]
- Gestational weight gain standards based on women enrolled in the fetal growth longitudinal study of the INTERGROWTH-21st project: a prospective longitudinal cohort study. BMJ. 2016;352:i555.
- [Google Scholar]
- Interdisciplinary group for advanced research on birth outcomes–DBT India initiative (GARBH-Ini). A pregnancy cohort to study multidimensional correlates of preterm birth in India: Study design, implementation, and baseline characteristics of the participants. Am J Epidemiol. 2019;188:621-31.
- [Google Scholar]
- Impact of an integrated nutrition, health, water sanitation and hygiene, psychosocial care and support intervention package delivered during the pre- and peri-conception period and/or during pregnancy and early childhood on linear growth of infants in the first two years of life, birth outcomes and nutritional status of mothers: Study protocol of a factorial, individually randomized controlled trial in India. Trials. 2020;21:127.
- [Google Scholar]
- Pooled estimate of vitamin D deficiency among pregnant women in India: A systematic review and meta-analysis. J Health Popul Nutr. 2021;40:28.
- [Google Scholar]
- The complex relationship between iron status and anemia in pregnant and postpartum women in India: Analysis of two Indian study cohorts of uncomplicated pregnancies. Am J Hematol. 2023;98:1721-31.
- [Google Scholar]
- Vitamin B12 status in pregnant women and their infants in South India. Eur J Clin Nutr. 2017;71:1046-53.
- [Google Scholar]
- Prevalence of vitamin b12 deficiency and its associated risk factors among pregnant women of rural South India: A community-based cross-sectional study. Indian J Community Med. 2020;45:399-404.
- [Google Scholar]
- Maternal vitamin B12 status during pregnancy and its association with outcomes of pregnancy and health of the offspring: A systematic review and implications for policy in India. Front Endocrinol. 2021;12:619176.
- [Google Scholar]
- Serum zinc levels amongst pregnant women in a rural block of Haryana state, India. Asia Pac J Clin Nutr. 2008;17:276-9.
- [Google Scholar]
- Prevalence and determinants of folate deficiency among urban Indian women in the periconception period. Eur J Clin Nutr. 2019;73:1639-41.
- [Google Scholar]
- Vitamin B6 levels and impaired folate status but not Vitamin B12 associated with low birth weight: Results from the MAASTHI birth cohort in South India. Nutrients. 2023;15:1793.
- [Google Scholar]
- Prevalence of thiamine deficiency in pregnancy and its impact on fetal outcome in an area endemic for thiamine deficiency. PLoS Negl Trop Dis. 2023;17:e0011324.
- [Google Scholar]
- Micronutrient deficiency in pregnancy: Time to think beyond iron and folic acid supplementation. Indian J Community Med. 2022;47:425-8.
- [Google Scholar]
- Subclinical vitamin A deficiency and anemia among women and preschool children from Northeast India. Indian J Community Med. 2020;45:371-4.
- [Google Scholar]
- Iron, folate, and vitamin B12 stores among pregnant women in a rural area of Haryana State, India. Food Nutr Bull. 2007;28:435-8.
- [Google Scholar]
- Low plasma vitamin B12 in pregnancy is associated with gestational “diabesity” and later diabetes. Diabetologia. 2009;52:2350-8.
- [Google Scholar]
- Vitamin B12 and folate concentrations during pregnancy and insulin resistance in the offspring: the Pune maternal nutrition study. Diabetologia. 2008;51:29-38.
- [Google Scholar]
- Vitamin B12 and folic acid supplementation and plasma total homocysteine concentrations in pregnant Indian women with low B12 and high folate status. Asia Pac J Clin Nutr. 2010;19:335-43.
- [Google Scholar]
- Vitamin B(12) intake and status in early pregnancy among urban South Indian women. Ann NutrMetab. 2013;62:113-22.
- [Google Scholar]
- Imbalance of folic acid and vitamin B12 is associated with birth outcome: an Indian pregnant women study. Eur J Clin Nutr. 2014;68:726-9.
- [Google Scholar]
- A prospective study of maternal fatty acids, micronutrients and homocysteine and their association with birth outcome. Matern Child Nutr. 2013;11:559-73.
- [Google Scholar]
- The etiology of anemia among pregnant women in the hill state of Himachal Pradesh in North India: A cross-sectional study. Cureus. 2022;14:e21444.
- [Google Scholar]
- Comprehensive National Nutrition Survey (CNNS) National Report. 2019.
- Diet and nutritional status of urban population in India and prevalence of obesity, hypertension, diabetes and hyperlipidaemia in urban men and women. A brief NNMB Urban Nutrition Report (NNMB Technical Report No. 27), 2017. ICMR-National Institute of Nutrition, Hyderabad.
- Diet and nutritional status of rural population, prevalence of hypertension & diabetes among adults and infants & young child feeding practices.- Report of Third Repeat Survey (NNMB Technical Report No-26), 2012. Hyderabad: ICMR-National Institute of Nutrition;
- How adequate are macro- and micronutrient intake in pregnant women with diabetes mellitus? A study from south India. J Obstet Gynaecol India. 2018;68:400-7.
- [Google Scholar]
- Pregnant women in four low-middle income countries have a high prevalence of inadequate dietary intakes that are improved by dietary diversity. Nutrients. 2019;11:1560.
- [Google Scholar]
- The upper level: examining the risk of excess micronutrient intake in pregnancy from antenatal supplements. Ann N Y Acad Sci. 2019;1444:22-34.
- [Google Scholar]
- Guidelines on Food Fortification with Micronutrients. Available from: https://iris.who.int/bitstream/handle/10665/43412/9241594012_eng.pdf?sequence=1. 2006, accessed on June 18, 2024.
- Review of the evidence regarding the use of antenatal multiple micronutrient supplementation in low‐ and middle‐income countries. Ann N Y Acad Sci. 2019;1444:6-21.
- [Google Scholar]
- The role of vitamins in the prevention and control of anaemia. Public Health Nutr. 2000;3:125-50.
- [Google Scholar]
- Oral iron supplementation in iron-deficient women: How much and how often? Mol Aspects Med. 2020;75:100865.
- [Google Scholar]
- National guidelines for calcium supplementation during pregnancy and lactation. Available from: https://nhm.gov.in/images/pdf/programmes/maternal-health/guidelines/National_Guidelines_for_Calcium_Supplementation_During_Pregnancy_and_Lactation.pdf, accessed on August 14, 2024.
- Vitamin D metabolism and guidelines for Vitamin D supplementation. ClinBiochem Rev Internet. 2020;41:103.
- [Google Scholar]
- Preventive Zinc supplementation among infants, preschoolers, and older prepubertal children. Food Nutr Bull. 2009;30:S12-40.
- [Google Scholar]
- Interactive effects of iron and zinc on biochemical and functional outcomes in supplementation trials. Am J Clin Nutr. 2005;82:5-12.
- [Google Scholar]
- Effect of zinc on efficacy of iron supplementation in improving iron and zinc status in women. J Nutr Metab. 2012;2012:216179.
- [Google Scholar]