Translate this page into:
Quality of life after electroconvulsive therapy in persons with treatment resistant schizophrenia
Reprint requests: Dr. B.S. Chavan, Professor & Head, Department of Psychiatry, 5th floor, D block, Government Medical College & Hospital, Sector 32, Chandigarh 160 032, India e-mail: drchavanbs@yahoo.com
-
Received: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
In recent years, health-related quality of life (QOL) has been regarded as the most important dimension of outcome in schizophrenia. Recent research has shown that atypical antipsychotics improve QOL in patients with schizophrenia. Importance of electroconvulsive therapy (ECT) has been demonstrated in restoring function and health related quality of life in depressed patients. However, there are no data on patients of schizophrenia. The objective of the present study was therefore, to assess the improvement in quality of life after ECT in treatment resistant schizophrenia.
Methods:
Thirty consecutive patients of treatment resistant schizophrenia were given ECT sessions twice a week and assessments were made with Positive and Negative Syndrome Scale of Schizophrenia (PANSS), WHO QOL Bref, Global Assessment of Functioning Scale and Clinical Global Impressions.
Results:
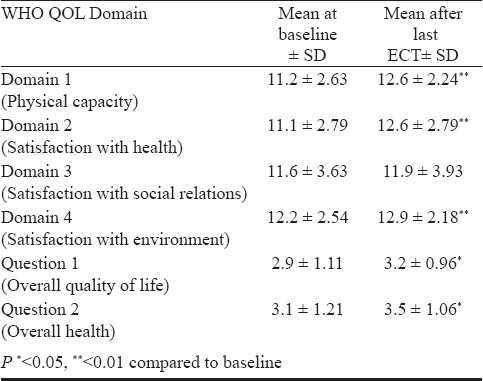
The group improved significantly on all the domains of quality of life scale except the domain named satisfaction with social relations. There was also significant change in the total score of PANSS after 6 ECT sessions (mean at baseline = 86.7, mean after 6 ECT = 65.5, P< 0.001) as well as on different subscales of PANSS. The score on the global assessment of functioning also changed significantly (mean 26.3 at baseline to 44.5 after 6 ECT sessions).
Interpretation & conclusions:
The present findings showed that ECT in addition to improvement in symptomatology led to improvement in QOL in patients of treatment resistant schizophrenia.
Keywords
Electroconvulsive therapy
quality of life
treatment resistant
schizophrenia
In recent years, health-related quality of life (QOL) has been regarded as the most important dimension of outcome in schizophrenia and other serious mental disorders1. However, the determinants of quality of life are poorly understood in this population. Studies have relied on combined measures of subjective and objective QOL2. Indicators of QOL include living situation, marital status, employment status, and involvement in social activities. Although psychiatric symptoms have been associated with subjective measures of QOL, symptom reduction alone often does not result in meaningful improvements in QOL. The results of a meta-analysis suggest that general psychopathology is the strongest contributor to poor QOL3.
Early Identification and treatment of mental disorders generally enhances QOL4. Improvement in quality of life has become appropriate goal for maintenance pharmacological treatment in schizophrenic patients5. Atypical antipsychotics have been shown to improve QOL in patients with schizophrenia6 in comparison with first generation antipsychotics7.
An emerging literature demonstrates the importance of ECT in restoring function and health related quality of life in depressed patients89. There are no studies that have measured quality of life in schizophrenic patients who received ECT. The present study was planned to evaluate the efficacy of ECT in improving quality of life in patients of treatment resistant schizophrenia.
Material & Methods
Settings and patients: The study was conducted at the department of Psychiatry, Government Medical College and Hospital, Chandigarh, from February 2006 to August 2007. The sample consisted of 30 consecutive patients of treatment resistant schizophrenia (TRS)10. During the study period, a total of 42 patients were diagnosed as treatment resistant schizophrenia and of these, nine patients or their relatives refused to give consent for ECT. All the patients were admitted for ECT purpose but the family members of two patients refused admission. So, these patients were administered ECT on outpatient basis. Inclusion criteria were: Patients in the age group of 16 to 65 yr suffering from treatment resistant schizophrenia10, as diagnosed by two psychiatrists independently based on ICD 1011. Patients accompanied by reliable informants who were willing to participate in the study and who were ready to give consent for ECT and anaesthesia. Exclusion criteria were: (i) Patients who had associated medical problems, which could affect the course of illness as well as their fitness for general anaesthesia. (ii) Patients with co-morbid substance dependence except nicotine dependence. (iii) Patients who had received ECT in the past one-year or received at least four ECTs in the past without any significant improvement. (iv) Patients who were intellectually deficient.
The ethics committee of the institution approved the study protocol.
ECT technique: Patients were given ECT twice a week. The total number of sessions was not pre-determined. Patients were given ECT as long as they showed improvement. It was stopped when patients showed no further improvement on two consecutive ECT sessions or if the patient or informant refused further ECT sessions. The anaesthesia and ECT were carried out using standard procedure.
Concurrent antipsychotic medication: All patients were continued on the same antipsychotic drugs at the same dose that they were taking at the time of inclusion into the study. If the patients responded to ECT, the same medication was continued after ECT. If they did not respond even to 6 ECTs, they were prescribed a different antipsychotic to which they were not resistant earlier and ECT was stopped.
Assessment: World Health Organization Quality of Life Scale – brief version (WHO QOL - Bref)12 was used to assess quality of life. It was applied at the baseline and at the end of ECT course. WHOQOL Bref produces a quality of life profile. It is possible to derive 4 domain scores. The 4 domain scores denote an individual's perception of quality of life. Higher domain scores denote higher quality of life. There are also two items that are examined separately: question 1 asks an individual's overall perception of quality of life and question 2 asks an individual's overall perception of their health.
All the patients were assessed at baseline and at the end of ECT course on Positive and Negative Syndrome Scale (PANSS)13, Global Assessment of Functioning Scale (GAF)14 and the Clinical Global Impressions (CGI)15.
Statistical analysis: The baseline and post-treatment scores were analyzed by within patient contrast wilcoxon signed ranks test.
Results & Discussion
Of the 30 patients, 21 (70%) were males. 13 patients (43.3%) were between 26 and 35 yr of age and 20 (66.7%) were unmarried; 26 patients (86.7%) were unemployed at the time of intake into the study and 21 (70%) had a total family income of less than Rs. 3500 per month. Majority of patients (25, 83.3%) were living in a nuclear family and in urban areas (22, 73.3%). The mean age of the patients was 31.53 ± yr with a range of 21 to 45 yr. The mean duration of illness was 9.67 ± 3.956 yr (range 4-17 yr).
Prior to inclusion in the study, majority of patients had taken risperidone (22, 73.33%) and olanzapine (17, 56.67%) in the past; 12 (40%) patients were resistant to clozapine. Other antipsychotics received were haloperidol, quetiapine, chlorpromazine, loxapine, ziprasidone, aripiprazole and trifluperazine. Many patients were resistant to more than two antipsychotics before inclusion into the study. The mean number of antipsychotics received was 2.8 with a range of 2-5.
Throughout the course of ECT, patients were continued on same antipsychotics that they were taking before induction into the study so that the treatment response could not be attributed to antipsychotic medication. Seven patients (23.33%) were on two antipsychotics at the time of entry into the study and the remaining 23 patients (76.67%) were on a single antipsychotic.
Outcome measures: The Table shows the score on four different domains of WHO-QOL at baseline and at the end of ECT course. The group improved significantly (P<0.01) on three domains which are classified as satisfaction with physical capacity, health and environment. The improvement seen on the third domain, which is classified as satisfaction with social relations was not significant. The total score on PANSS also changed significantly from 86.7 (± 14.05) at baseline to 65.5 (± 19.11) at the end of ECT course (P<0.001). There was significant change on three different domains of PANSS namely positive syndrome scale, negative syndrome scale and general psychopathology scale. There was a significant change in mean score between baseline and at the end of ECT course on GAF from 26.3 ± 7.18 at baseline to 44.5 ± 15.70 (P<0.001) and CGI from 5.6 ± 0.67 to 4.4 ± 1.24 (P<0.001). When the results were adjusted for possible confounding factors like age, gender, education, income, socio-economic status, it was found that none of these factors affected the results.
This was an open label, non-randomized, prospective study in which 30 patients of schizophrenia who were ill for 9.67 yr (range 4-17 yr) and were resistant to multiple antipsychotics, were started on ECT. In routine psychiatry practice in India, majority of patients and their family members carry multiple misconceptions related to ECT and getting consent for ECT is very difficult16. In the present study also, it was difficult to convince patients and their relatives to undergo ECT as is evident from the fact that 9 out of 42 patients refused ECT (refusal rate 21.4%).
There was significant improvement in QOL in three domains of WHOQOL-Bref i.e., physical capacity, satisfaction with health and environment. However, the change in score for the fourth dimension depicting satisfaction with social relation was not significant. The findings demonstrate that medication alone may not be sufficient to improve QOL in all spheres of life. Community perception towards a person suffering from mental illness may not change even after improvement in symptoms. Similar observations have been made earlier6. Psychosocial intervention targeting family members, friends, employers and community leaders should be made adjunct to medication.
The finding of a systematic review demonstrated that atypical antipsychotics have advantage over conventional medication in terms of improving subjective quality of life7. However, another study did not support these observations6. It has been documented that ECT results in a net improvement in function and quality of life for a period of at least 1 year after treatment1718. Our data also support the fact that ECT improves the QOL of treatment resistant patients of chronic schizophrenia.
In our study, the improvement in QOL from baseline to last ECT may be attributed to significant improvement in depressive, somatic concern and anxiety score on general psychopathology scale of PANSS. Earlier studies have also reported that psychiatry symptoms are the best independent predictors of subjective and objective QOL in schizophrenia45. The depressive symptoms and better cognitive functioning are associated with poor life satisfaction. The better insight because of better cognitive functioning can lead to self-devaluation and depression19.
Our study had certain limitations viz., short duration, lack of control group, and it was an open, non-randomized study. The patients were continued on antipsychotics that they were taking before entering into the study. All the patients were resistant to these drugs, however, ECT augmenting their effect cannot be ruled out.
In summary, ECT in addition to improvement in symptomatology leads to improvement in QOL in the domain of physical capacity, satisfaction with health and environment. However, lack of improvement in the domain of social relation necessitates the use of adjunct psychosocial interventions (cognitive behaviour therapy, social skill training, assertiveness training and supported employment) in the treatment of schizophrenia.
References
- Subjective and objective quality of life in schizophrenia. Schizophr Res. 2008;98:201-8.
- [Google Scholar]
- Psychiatric symptoms and quality of life in schizophrenia: A meta-analysis. Schizophr Bull. 2007;33:1225-7.
- [Google Scholar]
- Quality of life in treated and never treated schizophrenic patients. Acta Psychiatr Scand. 2001;103:131-42.
- [Google Scholar]
- Conventional versus atypical neuroleptics: subjective quality of life in schizophrenic patients. Br J Psychiatry. 1997;170:422-5.
- [Google Scholar]
- Social functioning and quality of life as measures of effectiveness in the treatment of schizophrenia. World Psychiatry. 2009;8:35-6.
- [Google Scholar]
- Quality of life in persons with schizophrenia in out-patient treatment with first or second generation antipsychotics. Acta Psychiatr Scand. 2004;110:108-18.
- [Google Scholar]
- A systematic review of quality of life and weight gain- related issues in patients treated for severe and persistent mental disorders: focus on aripiprazole. Neuropsychiatry dis Treat. 2009;5:117-25.
- [Google Scholar]
- Health-related quality of life in a clinical trial of ECT followed by continuation pharmacotherapy: effects immediately after ECT and at 24 weeks. J ECT. 2011;27:97-102.
- [Google Scholar]
- Health-related quality of life following ECT in a large community sample. J Affect Disord. 2006;90:269-74.
- [Google Scholar]
- Clozapine for the treatment resistant schizophrenic: A double blind comparison with chlorpromazine. Arch Gen Psychiatry. 1988;45:789-96.
- [Google Scholar]
- World Health Organization. In: The ICD –10 classification of mental and behavioral disorder: Diagnostic criteria for research. Geneva: World Health Organization; 1992.
- [Google Scholar]
- WHOQOL group. The World Health Organization's WHOQOL – Bref quality of life assessment: psychometric properties and results of the international field trial. A report from the WHOQOL group. Qual Life Res. 2004;13:299-310.
- [Google Scholar]
- The positive and negative syndrome scale for schizophrenia (PANSS) Schizophr Bull. 1987;13:261-76.
- [Google Scholar]
- The Global Assessment of Functioning Scale. A procedure for measuring overall severity of psychiatric disturbance. Arch Gen Psychiatry. 1976;33:766-71.
- [Google Scholar]
- US Department of Health, Education and Welfare, Publication no. 76-338. In: Clinical global impressions. Rockville MD: DHEW; 1976.
- [Google Scholar]
- Knowledge and attitude towards ECT among Indian patients. Indian J Psychiatry. 2006;48:34-8.
- [Google Scholar]
- Quality of life and function after electroconvulsive therapy. Br J Psychiatry. 2004;185:405-9.
- [Google Scholar]
- Electroconvulsive therapy is associated with superior symptomatic and functional change in depressed patients after psychiatric hospitalization. J Affect Disord. 2001;63:17-25.
- [Google Scholar]
- Personality, functioning, and recovery from major depression. J Nerv Ment Dis. 1996;184:240-5.
- [Google Scholar]






