Translate this page into:
Quality of asthma management in an urban community in Delhi, India
Reprint requests: Dr Anita Kotwani, Associate Professor, Department of Pharmacology, V. P. Chest Institute, University of Delhi, Delhi 110 007, India e-mail: anitakotwani@gmail.com
-
Received: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
High prevalence and poor control of asthma make its management a major public health issue worldwide, especially in developing countries. Optimum review of asthma management in the community is essential to improve asthma control. This study was conducted to investigate the quality of asthma management, knowledge about asthma and quality of life of asthma patients referred to a public tertiary care chest hospital in Delhi.
Methods:
Diagnosis of asthma was confirmed by symptoms and reversible spirometry in 50 referred patients on their first visit. Patients were interviewed using three questionnaires on quality of asthma management before visiting referral hospital, asthma knowledge and asthma quality of life (AQLQ). Correlation amongst quality of treatment, asthma quality of life, and asthma knowledge was also determined.
Results:
Findings revealed that only 60 per cent of patients were informed about their disease, and 10 per cent had undergone lung function tests previously. Only 44 per cent of patients were prescribed inhalers. None were provided with any educational material. Patients had poor knowledge of aetiology, pathophysiology, medication and how to assess the severity of their asthma. The mean scores in AQLQ indicated a moderate degree of impairment in quality of life.
Interpretations & conclusions:
This study provides evidence of unsatisfactory asthma management and patient-doctor interaction as patients had limited knowledge of asthma disease, its management and had poor quality of life as measured by a standardized questionnaire. Thus, there is need to implement suitable interventions to improve asthma management according to standard treatment guidelines in the community.
Keywords
Asthma
asthma knowledge
asthma management
India
quality of life
Asthma, a chronic disease, is a major health care issue worldwide due to its increasing prevalence in many countries following trends of urbanization and industrialization. India alone has an estimated burden of more than 15 million patients1. Despite the existence of effective medicines, asthma control is poor globally and especially in developing countries2. Poorly controlled asthma is associated with significant morbidity, mortality and socio-economic problems3. Assessing asthma management in the community is essential to plan for intervention studies to improve asthma control. Hence, the present study was conducted to examine asthma management in the community in the capital city of India, Delhi.
Earlier studies have documented that important factors leading to under-treatment of asthma include non-availability and under-use of basic tools like the spirometer for diagnosis and management of asthma45. Further, non-availability of essential inhalation medicines in most public sector hospitals and low affordability in developing countries make providing rational asthma management more difficult67. It has been reported that poor knowledge of both practitioners and patients and doctors who do not provide education about self-management of asthma to patients are important barriers to effective treatment and management of asthma8–11. Differences exist in prescribing patterns of anti-asthma medications across European countries, particularly under-use of asthma controller medications1213.
The gap in knowledge about asthma and its management is well recognized891415. Many international guidelines have been published with the aim to standardize the diagnosis and management of asthma with emphasis on patient education and providing self management plans to patients1617. Hence, patients’ knowledge is an integral component in the long-term management of asthma.
With this background, the present study was designed with an aim to assess the quality of treatment in the community and knowledge about asthma and quality of life in asthmatic patients who were referred to a referral public tertiary care chest hospital in Delhi.
Material & Methods
A questionnaire-based study was conducted from March to December 2006 at the out-patient department of Vallabhbhai Patel Chest Institute, Delhi, a tertiary care referral hospital. Patients from National Capital, Delhi and nearby towns are referred to this public hospital. The study was approved by the Institutional Ethics Committee. Informed written consent was obtained from the patients.
Patients aged ≥18 yr who presented to the chest clinic for the first time with history suggestive of asthma were included. They were evaluated and the diagnosis of bronchial asthma was confirmed based on the symptoms and reversible spirometry as per the Global Initiative for Asthma (GINA) guidelines16. Patients with an acute exacerbation of asthma and those with another concurrent respiratory disease or any systemic disease were excluded.
Spirometry was carried out on a dry rolling seal spirometer of computerized pulmonary function equipment (Benchmark Model, PK Morgan, UK) according to standardized guidelines of the American Thoracic Society/European Respiratory Society, 20051819.
Information on quality of prior treatment, patients’ knowledge about asthma and quality of life was obtained by using three questionnaires administered by one of the authors (AK). The two questionnaires, Asthma Knowledge and Asthma Quality of Treatment were developed on the basis of the GINA guidelines16. There is no “gold standard” for knowledge and, therefore, only content validity is relevant. The content of knowledge a patient is expected to have served as the basis for development of the questionnaire. Repeatability was tested by re-administration on another occasion and comparing the two sets of responses.
The “Asthma Quality of Life Questionnaire”20 is a standard tool extensively used for this purpose and its repeatability and validity have been well studied. The questionnaires were administered in a random order.
Quality of Treatment Questionnaire (Appendix 1): A questionnaire was developed based on the GINA guidelines for asthma management, both in English and a local language, Hindi. Hindi version of the questionnaire was used for all patients. It contains 20 questions which have been divided into the following four domains – Information about the health care provider (3 questions), Diagnosis and assessment of severity (4 questions), Treatment (6 questions) and Patient education (7 questions). Many questions in this questionnaire made inferences about the doctor talking to his/her patient about the diseases, treatment, education the patient received, and whether the patient had been given information about self-management. These questions gave insight into doctor-patient interaction, such as how doctors explain spirometery, techniques and precautions to be taken on the use of inhalers, the purpose of each inhaler, written action plans provided to the patient and how doctors explain the early signs of worsening of asthma and its management. Subject responses were categorical (yes/no) as well as structured multiple-choice. The percentage of subjects with different responses to each question was calculated.
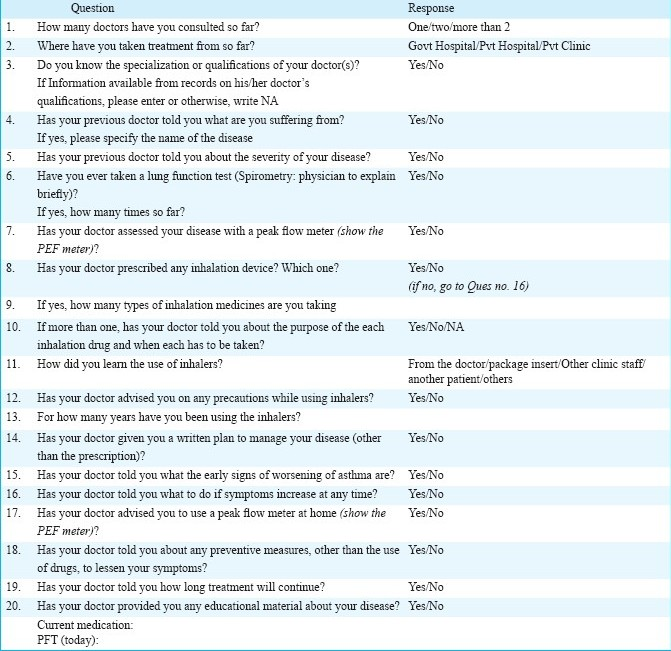
- Quality of Treatment Questionnaire for Asthmatics
Asthma knowledge questionnaire (Appendix 2): This was developed in both English and Hindi and designed to obtain information about different aspects of the disease that a patient is expected to be given to make him/her an active partner in self-management. The 28 questions were divided into the following six domains – Aetiology (3 questions), Pathophysiology (3 questions), Symptoms and assessment of severity (8 questions), Medication (8 questions), Prevention (4 questions) and Natural history (2 questions). Subject responses were scored on a categorical scale where 0 represented ‘no knowledge/no response’ and 1 represented knowledge of the subject addressed in a particular question. A final score was obtained by summing these scores. The maximum possible score was 28. The scores were expressed as percentage of the maximum possible score. The percentage of subjects with different responses to each question was also calculated.
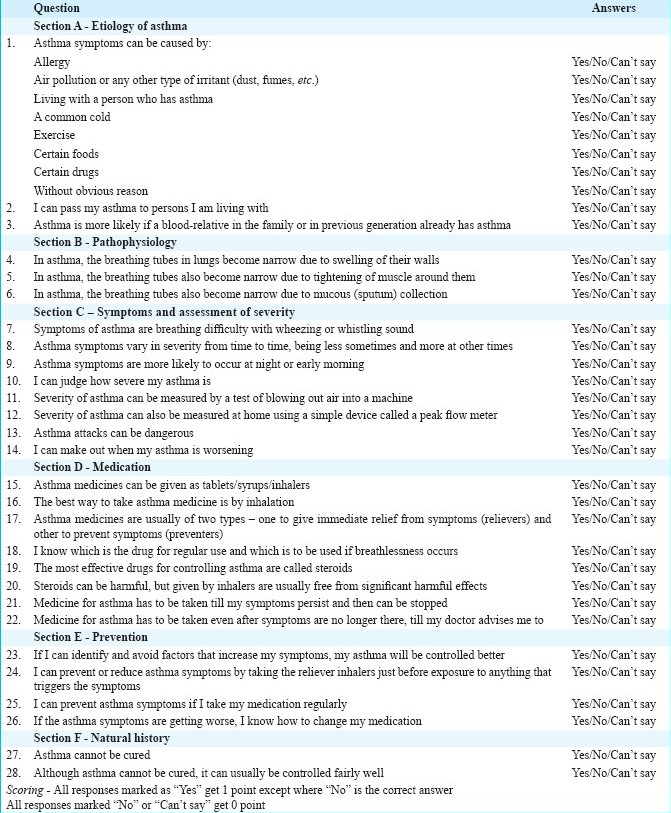
- Asthma Knowledge Questionnaire
Asthma quality of life questionnaire (AQLQ): AQLQ (provided kindly by Professor E. Juniper) is a standardized, widely available and validated instrument to assess quality of life in asthmatic patients. The Hindi version was used. The 32 questions of AQLQ are divided into the following four domains – symptoms (12 questions), activity limitations (11 questions), emotional function (5 questions), and environmental stimuli (4 questions). Patients respond to each question on a seven-point scale and recall their experiences during the previous two weeks. Each domain score also ranges from 1 to 7 with 1 representing the greatest impairment possible or most of the time and 7 represents the least or none of the time.
Statistical analysis: Scores obtained from AQLQ and Asthma Knowledge Questionnaire were expressed as Mean ± SD. Correlation between quality of treatment, asthma quality of life, the pulmonary function test parameter (Forced expiratory volume in one second, FEV1) and asthma knowledge was determined by using the Pearson correlation coefficient.
Results
Fifty adult patients (26 men and 24 women) completed the three interviewer administered questionnaires. Of these, 22, 18 and 10 patients, respectively had mild, moderate and severe persistent asthma. Twenty eight patients said that they had asthma for over 10 yr, and four patients had for more than one year but less than two years. Only eight patients had asthma for less than 1 yr.
Quality of treatment (Table I): Information about health care providers - Of the 50 patients, 33 (66%) had consulted more than one doctor before visiting the referral chest clinic. Up to 22 (44%) patients had no knowledge about their doctor's qualification. Among those who knew the qualifications of their doctor, 12 (24%) patients consulted MBBS doctors, 10 (20%) went to doctors with MD degree and 6 (12%) consulted practitioners from the alternative systems of medicine (homeopathy, unani, etc.) or unqualified medical practitioners.
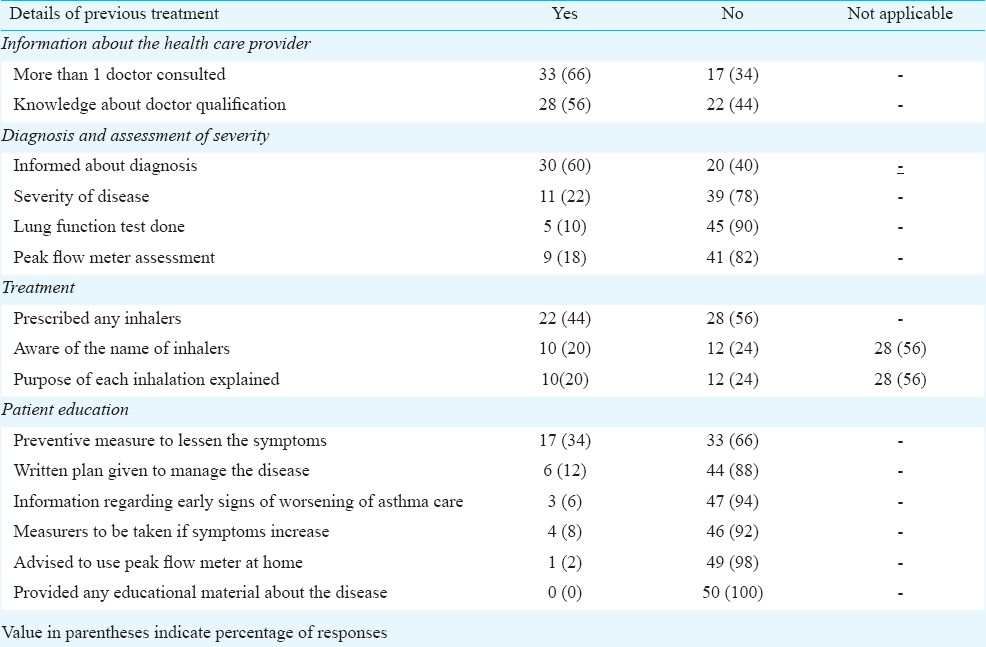
Diagnosis and assessment of severity - Only 30 (60%) patients were informed by their doctors that they were suffering from asthma; of these, only 11 (22%) patients were told about the severity of their disease. Lung function test and peak flow measurement were done in only 5 (10%) and 9 (18%) of patients, respectively.
Treatment - Of the total 50 patients, only 22 (44%) were prescribed inhaled therapy by their doctors. Of these 22 patients, only 10 were aware of the medicine in the inhalers and the purpose of inhalation. Of these 10 patients, eight were prescribed both reliever and preventer inhalers whereas two patients received only reliever therapy. Twelve patients revealed that they learnt the use of inhalers from the package insert, other patients or hospital staff other than their doctor.
Patient education - None of the subjects were provided with any educational material about the disease process. Only 6 (12%) patients were given a written plan to manage asthma in the event of a worsening condition but the content was never discussed by the doctor so these patients could not recall. Only 3 (6%) patients recalled having been given information regarding the early signs of worsening of asthma. One patient had an objective mean of assessing his asthma as he was advised to use a peak flow meter at home. Four patients were told about the measures to be taken if asthma symptoms increase. Up to 33 (66%) of patients revealed that they were not given any instructions regarding the preventive measures to lessen the symptoms of asthma.
Asthma knowledge: Scores obtained in different domains revealed that a large proportion of patients lacked basic knowledge about asthma and its treatment (Fig.).
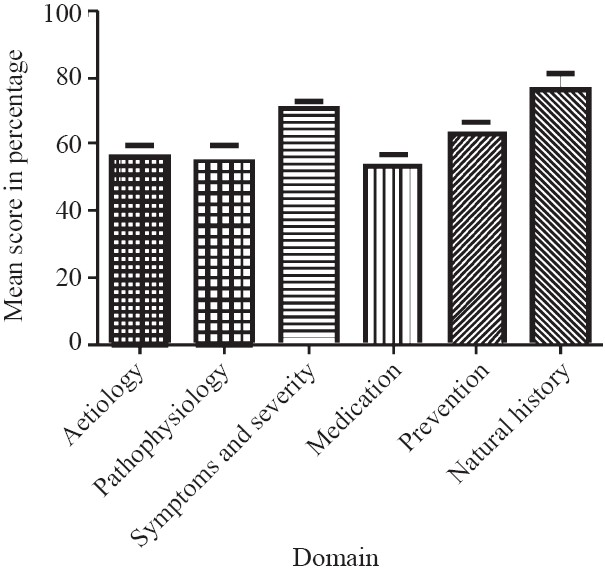
- Mean scores of different domains of Asthma Knowledge Questionnaire.
Aetiology - When patients were asked to identify the causative factors for asthma, 25 (50%) patients believed that asthma is a contagious disease and could be contracted by living with another asthma patient. Up to 74 per cent of patients (37) were not aware of the fact that drugs can also cause asthma symptoms.
Pathophysiology - Between 36 and 68 per cent patients (18-34) had knowledge of the underlying pathologic process during an asthma attack.
Symptoms and assessment of severity - Between 80 and 90 per cent patients (40-45) were aware of the symptoms of asthma. However, only 14 (28%) patients knew about the early signs of worsening of asthma. Merely 5 (10%) patients knew that the severity of asthma can be judged by a peak flow meter and the remaining 45 (90%) patients had no understanding of the concept. Ten per cent of patients did not think that asthma can be dangerous and can result in death during an attack.
Medication - Sixty per cent of patients did not know whether the drug prescribed to them was a “reliever” or “preventer” of asthma symptoms. Up to 30 per cent of patients did not believe that the best way of taking asthma medicines is by inhalation. Seventy eight per cent patients did not think steroids were the most effective drugs for controlling asthma and 68 per cent believed that steroids are in fact harmful even when given by inhalation route.
Prevention - Up to 68 per cent of patients knew that asthma could be prevented by avoiding trigger factors and by taking medication regularly.
Natural history - Thirty (60%) patients believed that asthma cannot be cured but 44 (88%) patients mentioned though asthma cannot be cured but can usually be controlled.
Asthma Quality of Life
The overall quality of life impairment due to asthma was moderate with a mean value of 3.68 ± 0.78. Mean scores in each domain are as shown in Table II.
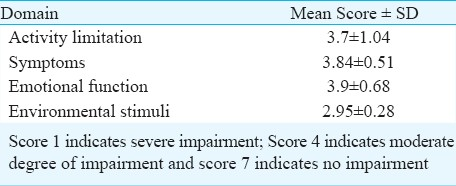
Activity limitation - Asthma limited the activities of all patients except one with moderate to severe limitation observed in 80 per cent of the patients. Strenuous activities such as running and walking upstairs led to symptoms in 94 and 88 per cent of patients respectively. Up to 60 per cent of patients reported moderate to very severe problems during sleep due to asthma.
Symptoms - Moderate to severe symptoms were observed in up to 36 (72%) patients. Up to 34 (68%) patients recalled waking up with asthma symptoms most of the time. Nocturnal asthma occurring most of the time over the past two weeks was reported by 27 (54%) patients.
Emotional function - About 82 per cent of the patients felt frustrated as a result of asthma and 84 per cent were concerned about having asthma in the past two weeks. Thirty eight per cent patients revealed that they felt worried most of the time when they did not have their asthma medicines with them.
Environmental stimuli - Environmental triggers such as dust, weather, air pollution, and strong smells were reported to have provoked recent asthma symptoms in 47 patients. Passive smoke exposure had provoked asthma in 37 (74%) patients. More than 80 per cent patients (40) reported avoiding situations because of potential exposure to these triggers.
Pulmonary function and correlation: Correlations between quality of treatment (QoT), asthma quality of life (AQLQ), and asthma knowledge (AK) were studied. A significant correlation was seen only between the quality of treatment and asthma knowledge (P<0.05) (Table III).

Discussion
Our study has identified substantial deficiencies in the management of asthma in an urban community in India. Other studies from different parts of the world have also reported under-treatment or under-use of essential asthma medication8913142122. In India, a majority of asthma patients in the community are managed by general practitioners in the private sector and non-specialized public sector physicians in primary/secondary health care facilities. Our previous study indicated that in many States of India essential inhalation medicines for asthma were not available in public sector7. Earlier studies from India and other countries have documented that general practitioners have poor knowledge about preventive therapy for asthma and its management8122123 which contributes to increased morbidity and mortality.
Guidelines recommend that the diagnosis and follow up of patients should be based on the evaluation of the frequency of symptoms and on the level and variability of the peak expiratory flow rate. However, in the present study, a spirometer or peak flow meter was used for diagnosis in only 10 and 18 per cent of patients, respectively. Non adherence to recommended treatment guidelines has been reported not only from developing but from developed countries as well2426. Results from these studies revealed that only 43 per cent of Australian general practitioners and 33 per cent of Spanish pediatricians routinely measured airways function with spirometers and peak flow meters25. Underutilization of these objective tools in management of asthma is a cause for concern.
Inhalers which are considered to be the mainstay of asthma therapy were prescribed to only 44 per cent of patients in our study. These findings are consistent with several other studies that also reported the underutilization of inhalers2224–27. The primary reason reported in earlier studies was the non-availability of free inhalers (medicines) in public facilities, where a large proportion of populations received prescribed oral medications, and low affordability at private sector facilities due to the high cost of inhalers2728. Consequently, to save cost, patients are prescribed and dispensed affordable oral medications29. Further, a survey conducted in Pakistan revealed that a few practitioners felt inhalers were addictive and should be reserved only for severe cases22.
It is of concern that many subjects were not aware of their doctor's qualification and the majority had consulted more than two doctors at primary and secondary healthcare before visiting the referral (tertiary) chest hospital. Another disappointing fact was that up to 40 per cent of patients were not given the diagnostic label of asthma by their doctors. This finding is consistent with an earlier study from Australia which reported that most practitioners believed that informing a patient that he or she has asthma is not important9. This fact also shows that most doctors at primary and secondary care facilities do not make a diagnosis based on lung function tests, as the equipment is not available in these facilities and they prescribe only symptomatic treatment. The findings of this study also gave an insight into doctor-patient interaction; only 10 patients were told by the doctor about the purpose of each inhaler and were advised how to use inhaler. Only 10 per cent of the patients were told about the peak flow meter and none of the patients were given any written education material. A poor doctor-patient relationship is also highlighted in other studies30. Hence, there is a pressing need for developing good partnerships between patients and doctors for the best practice in the treatment of asthma.
Our study revealed that a majority of the patients were misinformed about the aetiology of the disease, and its pathophysiology and management, whereas higher scores were observed in the domains of symptoms and natural history. Patients probably knew enough about the symptoms of asthma because of their own personal experience. Earlier studies also document that patients are ignorant or have distorted knowledge of their disease and the prescribed treatment which leads to poor compliance263132. Non adherence to the standard treatment leads to uncontrolled symptoms, limitation of daily life activities, unscheduled urgent healthcare visits and progression of the disease resulting in poor quality of life33.
The findings of our study indicate that prescriber as well as patient awareness and education is needed for effective management of asthma in the community. A systematic review by the Cochrane Airways group showed that written self-management action plans had significant benefits in reducing morbidity34. Effectiveness of patient education for asthma management has been shown in several studies from India and elsewhere35–37. There is an enormous gap between evidence-based standard guidelines for asthma management and clinical practice.
Limitations of our study include a small sample size from one chest hospital and a potential for recall bias. Generalization of the results should be done with caution as this study was done in at one referral hospital of Delhi.
In conclusion, this study provides evidence of unsatisfactory asthma management, poor doctor-patient interaction and poor patient education at primary and secondary care levels. Similar baseline studies are needed from other parts of India. Prescriber education at all levels of healthcare and proper patient education will enable patients to comply with treatment regimens and consequently improve the quality of life of asthma patients.
References
- The global burden of asthma: executive summary of the GINA Dissemination Committee Report. Allergy. 2004;59:469-78.
- [Google Scholar]
- Treatment outcome of asthma after one year follow-up in health centres of several developing countries. Int J Tuberc Lung Dis. 2006;10:911-6.
- [Google Scholar]
- Asthma control and future asthma-related morbidity in inner-city asthmatic children. Ann Allergy Asthma Immunol. 2008;101:144-52.
- [Google Scholar]
- Spanish Pediatric Asthma Study Group. The use of spirometers and peak flow meters in the diagnosis and management of asthma among Spanish pediatricians. Results from the TRAP study. Pediatr Allergy Immunol. 2004;15:365-71.
- [Google Scholar]
- Low-cost, open-source spirometry. 2009. Available from: http://davidvansickle.com/2009/02/low-costopen-source-spirometry/,
- [Google Scholar]
- Availability, price and affordability of asthma medicines in five Indian states. Int J Tuberc Lung Dis. 2009;13:574-9.
- [Google Scholar]
- General practitioners’ knowledge of childhood asthma in Delhi, India. Int J Tuberc Lung Dis. 2008;12:677-82.
- [Google Scholar]
- Knowledge of and reported asthma management among South Australian general practitioners. Br J Gen Pract. 1994;44:123-6.
- [Google Scholar]
- A study on perception of patients about bronchial asthma. Indian J Allergy Asthma Immunol. 2003;17:85-7.
- [Google Scholar]
- Patient education programme in bronchial asthma in India: why, how, what and where to communicate? Indian J Chest Dis Allied Sci. 1998;40:117-24.
- [Google Scholar]
- Prescribing patterns for asthma by GP in six European countries. Respir Med. 2000;94:578-83.
- [Google Scholar]
- How appropriate is asthma therapy in general practice? Fund Clin Pharmacol. 2005;19:107-15.
- [Google Scholar]
- The national asthma audit.Bridging the gap between guidelines and practice. Aust Fam Physician. 1998;27:907-13.
- [Google Scholar]
- Management of acute asthma: Gaps between opinion and recorded action by general practitioners. Int J Qual Health Care. 1997;9:405-12.
- [Google Scholar]
- Global strategy for asthma management and prevention: GINA executive summary. Eur Respir J. 2008;31:143-78.
- [Google Scholar]
- National Heart, Lung, and Blood Institute, National Institutes of Health,U.S. Department of Health and Human Services. (2007). Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma—full report. 2007. Available from: http://www.nhlbi.nih.gov/guidelines/asthma/asthgdln.htm
- [Google Scholar]
- American Thoracic Society. ATS documents: Statements, guidelines and reports. Available from: http://www.thoracic.org/statements/
- [Google Scholar]
- European Respiratory Society. Guidelines for respiratory medicine. Available from: http://www.ers-education.org/pages/default.aspx?id=2005
- [Google Scholar]
- Development and validation of the standardized Asthma Quality of Life Questionnaire (AQLQ(S)) J Allergy Clin Immunol. 1998;101:S 188-95.
- [Google Scholar]
- Undertreatment in a nonselected population of adult patients with Asthma. J Allergy Clin Immunol. 1996;98:514-21.
- [Google Scholar]
- Asthma management by general practitioners in Pakistan. Int J Tuberc Lung Dis. 2004;8:414-7.
- [Google Scholar]
- Perceptions of asthma among physicians: an exploratory study with the ISAAC video. Eur Respir J. 2005;26:829-34.
- [Google Scholar]
- Implementation of asthma guidelines in health centres of several developing countries. Int J Tuberc Lung Dis. 2006;10:104-9.
- [Google Scholar]
- Current outpatient management of asthma shows poor compliance with International consensus guidelines. Chest. 1999;116:1638-45.
- [Google Scholar]
- Cost analysis for treatment of mild essential hypertension and mild bronchial asthma. Indian J Pharmacol. 2002;34:222. (abstract)
- [Google Scholar]
- Affordability of inhaled corticosteroids as a potential barrier to treatment of asthma in some developing countries. Int J Tuberc Lung Dis. 2000;4:268-71.
- [Google Scholar]
- Management of asthma at private pharmacies in India. Int J Tuberc Lung Dis. 2006;10:1386-92.
- [Google Scholar]
- How well do asthma clinic patients understand their asthma? Br J Dis Chest. 1985;79:43-8.
- [Google Scholar]
- Asthma care and factors affecting medication compliance: the patients’ point of view. Int J Qual Health Care. 2001;13:375-83.
- [Google Scholar]
- Knowledge about asthma and its management in asthmatics of rural Punjab. Indian J Tuberc. 1993;40:153-5.
- [Google Scholar]
- Is adherence to drug treatment correlated with health related quality of life? Qual Life Res. 2003;12:621-33.
- [Google Scholar]
- Self management education and regular practitioner review for adults with asthma. Cochrane Database Syst Rev (1):CD001117.
- [Google Scholar]
- Reductions in hospital use from self management training for chronic asthmatics. Soc Sci Med. 1998;46:1087-93.
- [Google Scholar]
- The cost and effectiveness of an educational program for adults who have asthma. J Gen Int Med. 1991;6:401-7.
- [Google Scholar]
- A controlled trial of two forms of self management education for adults with asthma. Am J Med. 1993;94:564-76.
- [Google Scholar]






