Translate this page into:
Prospective study estimating healthcare associated infections in a paediatric hemato-oncology unit of a tertiary care hospital in north India
Reprint requests: Dr Arti Kapil, Professor, Department of Microbiology, All India Institute of Medical Sciences New Delhi 110 029, India e-mail: akapilmicro@gmail.com
-
Received: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Healthcare associated infections (HAIs) are responsible for morbidity and mortality among immunocompromised and critically ill patients. We undertook this study to estimate the burden of HAIs in the paediatric cancer patients in a tertiary care hospital in north India.
Methods:
This prospective, observational study, based on active surveillance for a period of 11 months was undertaken in a 4-bedded isolated, cubicle for paediatric cancer patients. Patients who stayed in the cubicle for ≥48 h, were followed prospectively for the development of HAIs.
Results:
Of the 138 patients, 13 developed 14 episodes of HAIs during the study period. Patient-days calculated were 1273 days. Crude infection rate (CIR) and incidence density (ID) of all HAIs were 9.4/100 patients and 11/1000 patient-days, respectively. Of the 14 episodes of HAIs, seven (50%) were of blood stream infections (HA-BSI), five (36%) of pneumonia (HAP) and two (14%) urinary tract infections (HA-UTI). The CIRs of HA-BSI, HAP and HA-UTI were 5.1, 3.6 and 1.4/100 patients, respectively. The corresponding IDs were 5.5, 3.9 and 1.6/1000 patient-days, respectively. Mean length of stay was significantly higher in patients who developed an HAI [13.8 (range 7-30), median (Interquartile range) 12 (11-14)] vs 7.5 days [range 2-28, median (interquartile range) 7 (5-9); P<0.0001]. Also mortality was significantly higher in patients who developed an HAI [23% (3/13) vs 3% (4/125), P<0.05].
Interpretation & conclusions:
The incidence of HAIs in the paediatric cancer patients in the study was 11/1000 patient days, of which HA-BSIs were the commonest. HAIs were associated with an increase in morbidity and mortality amongst this high risk patient population.
Keywords
Cancer
HA-BSI
HAP
healthcare associated infections
mortality
paediatric
Healthcare associated infections (HAIs) contribute significantly to the morbidity and mortality amongst critically ill and immunocompromised patients. The overall annual direct medical cost of HAIs to U.S. hospitals ranges from $28.4 - 45 billion1. A few studies from India have focused on measuring the burden of HAIs amongst patients of paediatric age group2345. In one such study, the incidence of all HAIs in a paediatric intensive care unit was 21 per 1000 patient days2. Due to their underlying illnesses and intensive anti-cancer treatment, paediatric cancer patients are at increased risk of infectious complications6789. HAIs in this patient population have been investigated in a few prospective studies, mostly from the developed world1011121314. Hence, the present study was undertaken to determine the burden of HAIs in this patient population in a paediatric oncology unit of a tertiary care hospital in north India, using active, prospective and patient based surveillance.
Material & Methods
This prospective study was done in the Leukemia Cubicle (LC) of the paediatric ward of the All India Institute of Medical Sciences (AIIMS), New Delhi, India, for 11 months from August 2007 - February 2008 and August- December 2008. LC is a 4-bedded isolated cubicle under the premises of the paediatric ward, specifically designated for admitting paediatric patients diagnosed with a malignancy. Such patients were admitted for various reasons such as initiation of chemotherapy, undergoing investigations relevant to their diagnosis and if they developed complications during treatment. In case of infectious complications, the main reason for admission was administration of intravenous antibiotics. Non-neutropenic patients were given injectable IIIrd generation cephalosporins with or without an aminoglycoside. The febrile neutropenic patients were given a combination of ceftazidime and an aminoglycoside. Vancomycin was added if haemodynamic instability was also found. All patients who were diagnosed with a malignancy were given alternate day co-trimoxazole as prophylaxis. The microbiologic workup for infections was guided by the clinical features and relevant clinical samples were collected. Children admitted in LC were discharged when they completed the intended chemotherapy and if they were admitted for management of infectious complications, they were discharged after they completed the intravenous antibiotics. All patients admitted in LC were assessed daily during their stay. Detailed data were taken only for children who stayed in LC for ≥ 48 h. After discharge from LC, they were followed for upto 48 h for the development of an HAI.
The study protocol was approved by the ethics committee of the institute and written informed consent was obtained from parents/guardians of the patients.
Case definition: A patient was diagnosed with an HAI during his/her stay in the LC, as per Centers for Disease Control & Prevention (CDC) criteria for site specific infections15. Healthcare associated blood stream infection (HA-BSI) must meet at least one of the following criteria: (i) Patient has a recognized pathogen cultured from one or more blood cultures and organism cultured from blood is not related to an infection at another site, and/or (ii) Patient has at least one of the following signs or symptoms: fever (>38°C), chills, or hypotension and positive laboratory results and signs and symptoms and positive laboratory results are not related to an infection at another site.
Healthcare associated urinary tract infection (HA-UTI) was diagnosed as: patient has at least one of the following signs or symptoms with no other recognized cause: fever (>38°C), urgency, frequency, dysuria, or suprapubic tenderness and patient has a positive urine culture, that is, ≥ 105 microorganisms per ml of urine with no more than two species of microorganisms.
Healthcare associated pneumonia (HAP) was diagnosed using radiological, clinical and laboratory criteria as follows: radiologically, two or more serial chest radiographs with at least one of the following: new or progressive and persistent infiltrate, consolidation, cavitation and pneumatoceles in infants ≤1 yr old. Clinically, for any patient, at least 1 of the following: Fever (≥38°C or ≥100.4°F) with no other recognized cause leukopenia (≤4000 WBC/μl) or leukocytosis (≥12,000 WBC/μl) and at least two of the following: (i) new onset of purulent sputum or change in character of sputum, (ii) new onset or worsening cough, or dyspnoea, or tachypnoea, (iii) rales or bronchial breath sounds and in laboratory at least one of the following: positive growth in blood culture not related to another source of infection or positive growth in culture of pleural fluids.
Microbiological diagnosis: Upon suspicion of development of an HAI, representative samples for the diagnosis of a site specific HAI were collected, processed and interpreted as per standard guidelines16. Identification of bacterial isolates grown was done by conventional biochemical tests for identification17. Antimicrobial susceptibility testing of the bacterial isolates was done by disk diffusion technique using Kirby Bauer's method as per Clinical Laboratory Standards Institute guidelines18.
Calculation of patient-days: The data for calculation of patient-days were collected using standardized National Nosocomial Infection Surveillance System protocols and definitions19.
Incidence or crude infection rate (CIR) of HAIs: CIR was determined as dividing the total number of patients who developed an HAI by total number of patients stayed for ≥48 h and multiplying the result by 100. CIR of a site specific HAI was calculated similarly.
Incidence density (ID) of HAIs: ID of HAIs was calculated by dividing the total episodes of HAI x 1000 by patient-days. The ID of a site specific HAI was calculated by dividing the total episodes of site specific HAI x 1000 by patient-days.
Mean length of stay (LOS): It was calculated as the total number of days spent in the LC by patients who stayed for ≥48 h was divided by total number of patients who stayed in LC for ≥48 h.
Crude excess mortality: It was determined as the difference between the crude overall case-fatality of patients with an HAI and the crude case-fatality of patients hospitalized in the LC, who did not developed an HAI.
Statistical analyses: Data were managed on MS Excel and analyzed using Stata software, version 7.0 (Stata Corp., College Station, Tx, USA). Mann-Whitney test and Fisher's exact test were used for statistical analysis.
Results
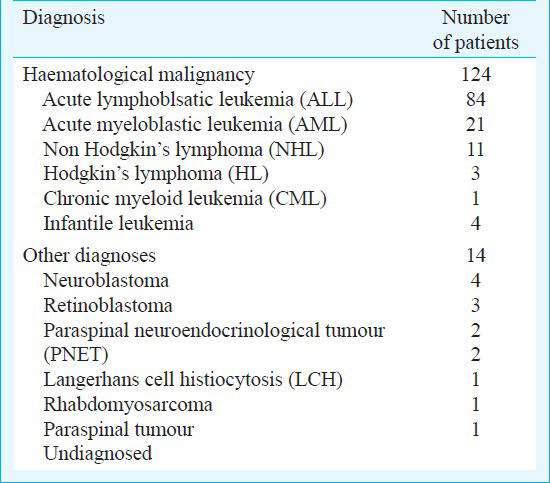
One hundred thirty eight patients were included in the study. Of these, 107 (77.5%) were male and 31 (22.5%) were female; six (4%) were <1yr old, 79 (57%) were between 1-6 yr and 53 (39%) were >6 yr of age. The distribution of the patients’ diagnoses is given in Table I. Of these 138 patients, 124 (90%) had haematological malignancies whereas 14 (10%) had malignancies other than haematological. Of the 138 patients, 42 (30%) were admitted for the purpose of instituting chemotherapy. Of these, 14 patients were admitted for receiving induction chemotherapy. Forty six (33%) of 138 patients had febrile neutropenia on admission in the hospital.
Of the 138 patients, seven (5%) died during the hospitalization. Of these, five were diagnosed with acute lymphoblastic leukemia (ALL) and one each had Burkitt's lymphoma with superior mediastinal syndrome and acute myeloblastic leukaemia (AML). Of the five patients with ALL, four had febrile neutropenia on admission and one had ALL relapse with hyperleucocytosis. The antecedent causes for death were sepsis with pneumonia in four patients and septic shock alone in three patients.
Of the 13 patients who developed an HAI in LC, nine (69%) were male, two (15%) were <1 yr of age at admission, seven (54%) belonged to 1-6 yr age group and four (31%) were >6 yr of age. Of these 13 patients, five patients each were of ALL and AML, two had neuroblastoma and one had non Hodgkin's lymphoma (NHL). Also, four of these 13 patients had febrile neutropenia at the time of diagnosis of an episode of HAI. Three (23%) of 13 patients died, who were diagnosed with ALL, AML and Burkitt's lymphoma, respectively. The antecedent causes for death amongst them were sepsis with pneumonia in two patients and septic shock alone in the patient diagnosed with AML.
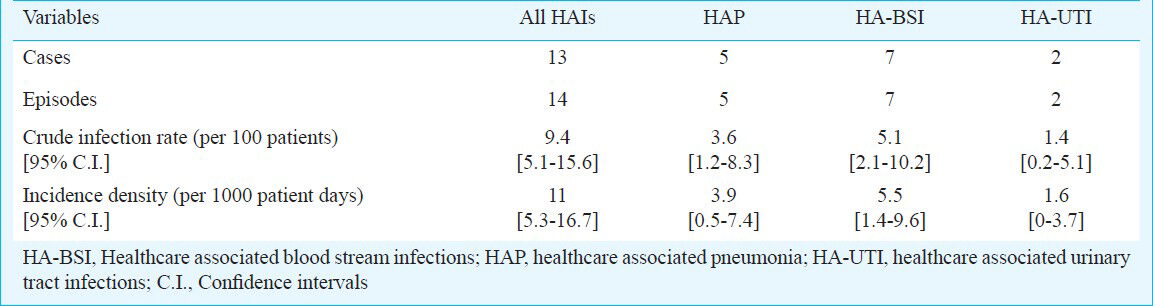
Total incidence rats of HAIs: Of the 138 patients included, 14 episodes of HAIs occurred in 13 patients, while their stay in LC. The CIR of all HAIs was 9.4 [95% Confidence interval (C.I.): 5.1-15.6] per 100 patients. During the study period, total patient-days calculated were 1273. The ID of all HAIs was 11 [95% C.I.: 5.3-16.7] per 1000 patient-days (Table II). No case of HAI was documented within 48 h after discharge from hospital.
Site specific infections in LC
(i) HA-BSI: Seven episodes of HA-BSI occurred. The CIR was 5.1 [95% C.I.: 2.1-10.2] per 100 patients and ID was 5.5 [95% C.I.: 1.4-9.6] per 1000 patient-days (Table II). In these seven episodes, eight bacterial organisms were implicated as one episode was polymicrobial due to Klebsiella pneumoniae and Pseudomonas aeruginosa. In all, two episodes each were due to Staphylococcus aureus, K. pneumoniae and P. aeruginosa and one episode each was due to coagulase negative Staphylococcus (CoNS) and Escherichia coli. One more episode of BSI occurred due to K. pneumoniae, which was secondary due to HAP.
(ii) HAP: Five episodes of HAP occurred during the study period. The CIR and ID were 3.6 [95% C.I.: 1.2-8.3] per 100 patients and 3.9 [95% C.I.: 0.5-7.4] per 1000 patient-days, respectively (Table II). Of these, four episodes were diagnosed clinically and radiologically. No bacterial aetiology was established in these cases. One episode was due to K. pneumoniae and secondary bacteraemia due to K. pneumoniae also occurred in this patient.
(iii) HA-UTI: Two episodes of HA-UTI occurred. The CIR and ID were 1.4 [95% C.I.: 0.2-5.1] per 100 patients and 1.6 [95% C.I.: 0-3.7] per 1000 patient-days, respectively (Table II). K. pneumoniae and E. coli were implicated in the causation of these episodes.
Antimicrobial susceptibility profile of bacterial isolates: All four isolates of K. pneumoniae, were extended spectrum beta lactamase (ESBL) producers, two were resistant to carbapenems while only one was sensitive to piperacillin-tazobactam. Both isolates of E. coli were ESBL producers and sensitive to carbapenems. Of the two isolates of S. aureus, one was methicillin resistant i.e. MRSA. Of the two isolates of P. aeruginosa, one was resistant to both ceftazidime and carbapenems, whereas only one isolate was resistant to piperacillin-tazobactam.
Length of stay (LOS) and outcome: The mean LOS of 138 patients was 8.1 (95% C.I.: 6.5-9.7) ± 4.93 days, [range 2-30, median (interquartile range, IQR) 7 (4-12)]. The mean LOS was significantly increased in patients who developed an HAI [13.8 (95% C.I.: 10.1-17.5) ± 6.8 days (range 7-30, median 12, IQR 11-14)] when compared to those who did not [7.5 (95% C.I.: 6.7-8.3) ± 4.5 days (range 2-28, median 7, IQR 5-9)] (P<0.001).
Overall, seven (5%) patients died in the study group. The mortality was significantly increased in patients who developed an HAI [23% (3/13) (C.I.: 5-53.8%) vs 3% (4/125) (C.I.: 0.1-8%), P<0.05]. Crude excess mortality in patients who developed an HAI was 20 per cent (95% C.I.: 3.3-42.9%).
Discussion
With current advances in therapeutics, the duration of survival of cancer patients has increased which in turn leads to prolonged periods of immunosuppression, predisposing them to various infections, especially nosocomial, if they repeatedly encounter the hospital environment. The burden of HAIs in paediatric hemato-oncology patients has been estimated in only a few studies1011121314. Our estimate of an incidence of 9.4 per 100 patients and an ID of 11 per 1000 patient-days was similar to the data reported from western countries. However, in a multicentric study done14 in the cancer patients of Germany and Switzerland, the ID of HAIs was much lower at 4.8 infections per 1000 patient-days. There are no reports from developing countries estimating the burden of HAIs in paediatric haemato-oncology patients. We observed significant increase in the length of stay in the hospital and the risk of death amongst patients who developed an HAI.
The most common site specific HAI identified in our study was blood stream infection. The neutropenic fever of unknown origin (nFUO) was not included as an HAI in our study, in accordance with the CDC definitions of site specific HAIs15.
In our study, Gram-negative bacilli (GNBs) were responsible for the majority of HAIs, as 70 per cent culture positive episodes were caused by GNBs. This finding was in contrast to the studies available from various developed countries where Gram-positive cocci (GPCs) have been implicated in the majority of HAIs. Simon et al14 and Urrea et al11 reported that 68 and 78 per cent, of nosocomial BSIs in paediatric cancer patients were caused by GPCs, respectively. However, various studies from India have implicated GNBs, particularly Acinetobacter spp. and P. aeruginosa as the commonest bacterial organisms implicated in the causation of culture positive HAIs34520. Prabhash et al21 reported that GNBs were responsible for 68 per cent culture positive BSIs in the cancer patients. Pseudomonas spp. were the most common organisms, being responsible for 37 per cent of all cases, however, these were not always nosocomial. In our study, K. pneumoniae was the most common bacterial organism implicated in the causation of culture positive HAIs, being responsible for 40 per cent episodes.
One major limitation of our study was the short duration of surveillance and scarce number of episodes of occurrence of HAIs. With our observed prevalence of HAI, our sample size of 138 patients was adequate to estimate this prevalence with an absolute error margin of ± 5 per cent, in a 95% 2-sided confidence interval. However, with such a margin of error being high, the results need to be interpreted with this limitation.
To conclude, our study showed that the HAIs were associated with increased morbidity and mortality in paediatric cancer patients. The bacterial organisms implicated were different from those found in the developed world. Hence, active surveillance for HAIs in this patient population should be a necessary component of infection control strategies in the hospitals of developing world.
References
- The Direct Medical Costs of Healthcare-Associated Infections in U.S. Hospitals and the Benefits of Prevention. 2009. Centers for Disease Control and Prevention. Available from: http://www.cdc.gov/HAI/pdfs/hai/Scott_Costpaper.pdf
- [Google Scholar]
- Burden of healthcare-associated infections in a paediatric intensive care unit of a developing country: a single centre experience using active surveillance. J Hosp Infect. 2011;78:323-6.
- [Google Scholar]
- Nosocomial bloodstream infection in a pediatric intensive care unit. Indian J Pediatr. 2008;75:25-30.
- [Google Scholar]
- Nosocomial pneumonia in a pediatric intensive care unit. Indian Pediatr. 2007;44:511-8.
- [Google Scholar]
- Study of nosocomial primary bloodstream infections in a pediatric intensive care unit. J Trop Pediatr. 2007;53:87-92.
- [Google Scholar]
- Incidence of septicaemias and invasive mycoses in children undergoing treatment for solid tumours: a 12-year experience at a single Italian institution. Eur J Cancer. 2001;37:2413-9.
- [Google Scholar]
- Fungal infections in children with cancer: a prospective, multicenter surveillance study. Pediatr Infect Dis J. 2006;25:634-9.
- [Google Scholar]
- Incidence of bacteremias and invasive mycoses in children with high risk neuroblastoma. Pediatr Blood Cancer. 2007;49:672-7.
- [Google Scholar]
- Incidence of catheter-related infections within 30 days from insertion of Hickman-Broviac catheters. Pediatr Blood Cancer. 2007;48:35-8.
- [Google Scholar]
- Surveillance for nosocomial and central line-related infections among pediatric hematology-oncology patients. Infect Control Hosp Epidemiol. 2000;21:592-6.
- [Google Scholar]
- Nosocomial infections among pediatric hematology/oncology patients: results of a prospective incidence study. Am J Infect Control. 2004;32:205-8.
- [Google Scholar]
- A prospective study of septicaemia on a paediatric oncology unit: a three-year experience at The Royal Liverpool Children's Hospital, Alder Hey, UK. Eur J Cancer. 2005;41:2132-40.
- [Google Scholar]
- Surveillance of nosocomial infections in paediatric recipients of bone marrow or peripheral blood stem cell transplantation during neutropenia, compared with adult recipients. J Hosp Infect. 2006;62:80-8.
- [Google Scholar]
- Healthcare-associated infections in pediatric cancer patients: results of a prospective surveillance study from university hospitals in Germany and Switzerland. BMC Infect Dis. 2008;8:70.
- [Google Scholar]
- CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control. 2008;36:309-32.
- [Google Scholar]
- Laboratory strategy in the diagnosis of infective syndromes. In: Collee G, Marmion BP, Fraser AG, Simmons A, eds. Mackie and McCartney practical medical microbiology (14th ed). London, UK: Churchill Livingstone; 1996. p. :53-94.
- [Google Scholar]
- Tests for the identification of bacteria. In: Collee G, Marmion BP, Fraser AG, Simmons A, eds. Mackie and McCartney practical medical microbiology (14th ed). London, UK: Churchill Livingstone; 1996. p. :131-49.
- [Google Scholar]
- CLSI. Performance Standards for antimicrobial susceptibility testing; 21st Informational Supplement. CLSI document M100-S21. Wayne PA: Clinical and Laboratory Standards Institute; 2011.
- [Google Scholar]
- Surveillance of nosocomial infections. In: Mayhall CG, ed. Hospital epidemiology and infection control (3rd ed). Philadelphia: Lippincott Williams & Wilkins; 2004. p. :1659-702.
- [Google Scholar]
- Nosocomial bacteraemia in intensive care unit patients of a tertiary care centre. Indian J Med Res. 2005;122:305-8.
- [Google Scholar]
- Blood stream infections in cancer patients: A single center experience of isolates and sensitivity pattern. Indian J Cancer. 2010;47:184-8.
- [Google Scholar]






