Translate this page into:
Propofol or sevoflurane anaesthesia does not affect hepatic integrity as assessed by the M30 & M65 cell death markers & liver enzymes
Reprint requests: Dr Argyro Fassoulaki, Department of Anaesthesia, Aretaieio Hospital, University of Athens, 76 Vasilisis Sofias Ave, 11528, Athens, Greece e-mail: afassou1@otenet.gr, fassoula@aretaieio.uoa.gr
-
Received: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
General anaesthetics may induce apoptosis. The pro-apoptotic/necrotic markers M30 (caspase-cleaved cytokeratin-18) and M65 (intact cytokeratin-18) have been used to identify early apoptosis in liver disease. The aim of this study was to detect the effect of propofol and sevoflurane anaesthesia on these markers and blood transaminase levels in female patients undergoing elective surgery.
Methods:
Sixty-seven women undergoing mastectomy or thyroidectomy under general anaesthesia were randomly allocated to the propofol or sevoflurane groups. Venous blood samples for measuring the apoptotic and necrotic markers M30 and M65 as well as for measuring the alanine aminotransferase (ALT) and the aspartate aminotransferase (AST) liver enzymes were collected before induction of anaesthesia, immediately after completion of surgery, and 24 and 48 h postoperatively.
Results.
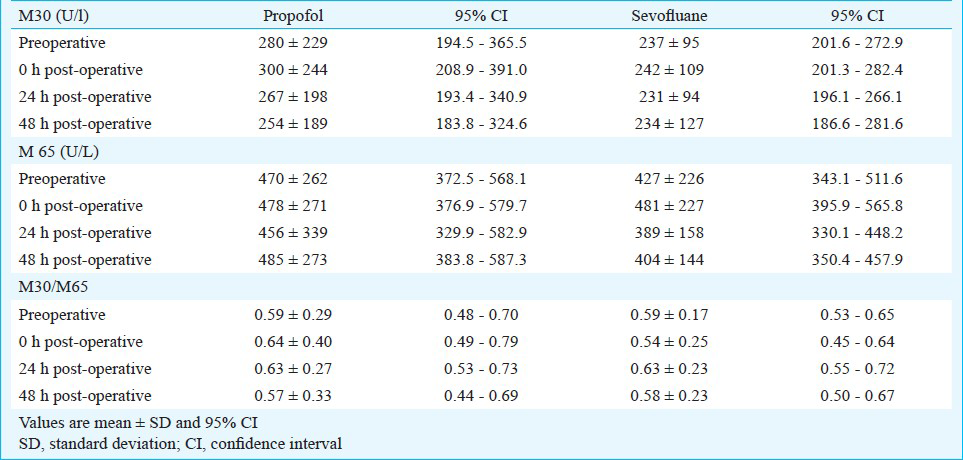
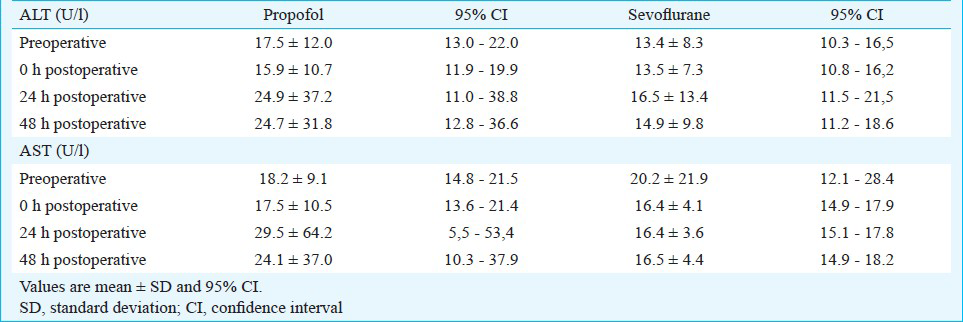
The M30 values preoperatively and 0, 24 and 48 h postoperatively were 280±229, 300±244, 267±198 and 254±189 U/l in the propofol group and 237±95, 242±109, 231±94 and 234±127 U/l in the sevoflurane group, respectively. The M30 values did not differ within or between the groups. The M65 levels at the same time intervals were 470±262, 478±271, 456±339 and 485±273 in the propofol group and 427±226, 481±227, 389±158 and 404±144 U/l in the sevoflurane group, respectively. No significant changes were found in the M65 either within or between the propofol and the sevoflurane groups. The ALT and AST levels did not change at these time intervals.
Interpretation & conclusions:
Under the present study design propofol or sevoflurane anaesthesia did not induce apoptosis or affected the liver function as assessed by the M30, M65 markers and liver enzymes in patients undergoing mastectomy or thyroidectomy under general anaesthesia.
Keywords
Anaesthesia
apoptosis
liver
M30
M65
necrotic markers
propofol
sevoflurane
General anaesthetics though considered safe, on rare occasions have been incriminated for severe liver damage and patient's fatal outcome1234. Propofol has been shown to exert an apoptotic effect on the human promylocytic leukemia cells (HL-60 cells), which are sensitive to proapoptotic stress, as the drug interferes with both the mitochondrial and cell surface pathways1. In the clinical setting, cases of hepatotoxicity after exposure to propofol anaesthesia for short duration surgery have been reported, with high transaminase levels and liver histology indicating hepatocellular injury2.
Sevoflurane has also been shown to cause hepatotoxicity. Hepatic necrosis occurred in a 37 yr old man after sevoflurane anaesthesia4. Fulminant hepatic necrosis with fatal outcome occurred in another patient exposed to sevoflurane for repair of a torn subclavian vein during central venous catheter insertion4.
The M30 (caspase-cleaved cytokeratin-18) is a monoclonal antibody, which recognizes a neoepitope generated from caspase cleaved keratin-18 at the Asp396 site, and serves as a biomarker of epithelial apoptosis in the liver. The M65 (intact cytokeratin-18) is a substrate expressed by epithelial cells like hepatocytes suggesting necrosis6. The circulating levels of the M30 and M65 have been used to assess severe liver impairment in pathological conditions like fibrosis in heavy alcohol drinkers7, to identify patients suffering from α1- antitrypsin deficiency later developing liver disease8, and as predictive markers in acute liver failure due to acetaminophen toxic doses9.
The aim of this study was to identify possible changes in the apoptotic and/or necrotic markers M30 and M65 and in the alanine aminotransferase (ALT) and aspartate aminotransferase (AST) enzymes, in female patients undergoing elective mastectomy or thyroidectomy under propofol or sevoflurane anaesthesia.
Material & Methods
The study was approved by the Aretaieio University Hospital Institutional Review Board (Hospital Ethics Committee, Reference number, Σ-74/07-07-2009) and registered in a clinical trial registry (www.clinicaltrials.gov) under the identification number NCT01000337. All patients gave their written informed consent. This prospective, randomized clinical study was conducted between October 2009 and July 2011 in Aretaieio University Hospital, Athens, Greece.
Female adult patients undergoing elective surgery for mastectomy or thyroidectomy were randomly assigned using computer-generated random numbers (www.randomizer.org) to receive either total intravenous anaesthesia with propofol (Propofol group) or inhalational anaesthesia with sevoflurane (Sevoflurane group). Two sets of 30 unique numbers per set were generated, each set corresponding to one of the groups and the numbers of each set to individual patients. The statistician and the laboratory specialist who analyzed the blood samples were blinded to the study groups. In contrast, the anaesthesiologist who administered anaesthesia was aware of the group the patient was allocated.
Exclusion criteria were age older than 65 yr, body weight exceeding 20 per cent of the ideal, hepatic, renal or cardiovascular disease, elevated ALT and AST enzymes, drug allergies, previous chemotherapy, bronchial asthma, chronic obstructive pulmonary disease, haematological disorders, pregnancy, alcohol or drug addiction, history of convulsions, unstable angina pectoris, myocardial infarction within the last six months and general anaesthesia within the last three months.
Before the study, estimation of the sample size was performed using the program GPower3.1 (http://www.psycho.uni-duesseldorf.de). For an effect size of 0.20, assuming a two-sided type I error of 0.05 and a power of 0.80, a sample size of 60 patients (30 patients in each group) was calculated. The sample size was increased further to allow for dropouts and missing data. For these reasons 67 patients were included.
Anaesthetic technique: In the operating room, standard monitoring including non-invasive measurement of systolic and diastolic arterial pressure, heart rate monitoring with electrocardiography and peripheral oxygen saturation (SpO2) with a pulse oximeter was applied to all patients (S/5 Anaesthesia Monitor, GE Healthcare Oy, Helsinki, Finland). Bispectral Index (BIS) monitoring (Aspect Medical Systems A-2000 XP, Newton, MA, USA) was used targeting to BIS values intraoperatively between 40 and 50 in all patients.
An intravenous (iv) 18 G cannula was inserted on the dorsal side of the hand and 10 ml of blood was obtained before induction of anaesthesia. Subsequently, patients received i.v. 50 mg ranitidine (Zantac, GlaxoSmithKline, Middlesex, UK) and 10 mg metoclopramide (Primperan, Sanofi-Aventis, Paris, France). All patients were preoxygenated for three minutes. Before induction of anaesthesia 1 g of iv paracetamol (Apotel, Uni-Pharma, Athens, Greece) and 100 mg of iv tramadol (Tramal, Vianex SA, Athens, Greece) were given. Supplementary analgesia was provided intraoperatively by 50 per cent nitrous oxide.
In the propofol group anaesthesia was induced with iv administration of propofol (2-2.5 mg/kg) (Lipuro, B. Braun Medical Supplies Inc., Taguig City, Philippines) and maintained with continuous propofol intravenous infusion. The maintenance dose of propofol was 6 mg/kg by means of an ordinary syringe pump (Graseby syringe pump 3100, Graseby Medical Ltd., UK) but this rate was changed manually as required, to maintain BIS between 40 and 50. In the sevoflurane group, anaesthesia was induced with 8 per cent sevoflurane (Sevorane, Abbott Laboratories, Illinois. USA), in 6 l/min of oxygen until BIS values were decreased to 40-50. Subsequently, the trachea was intubated and sevoflurane inspired concentration was decreased to about 1.8-2 per cent targeting to maintain BIS between 40 and 50. As it is difficult to administer equipotent anaesthetic doses of propofol and sevoflurane in terms of mg and inspired concentrations, propofol infusion doses and sevoflurane inspired concentrations were adjusted to obtain intraoperatively BIS values between 40 and 50, which indicated an adequate depth of anaesthesia.
Intraoperatively, both groups were receiving 50 per cent N2O in oxygen, with a total gas flow 2 l/min. Intubation was facilitated in all patients with administration of 0.6 mg kg rocuronium (Esmeron, N.V. Organon, Netherlands). All patients were mechanically ventilated to maintain the end tidal CO2 around 4.7 kPa. At the end of surgery the residual block was reversed with sugammadex 2 mg/kg (Bridion, N.V. Organon, Netherlands). After extubation, the patients were transferred to the Postanaesthesia Care Unit, where they were monitored for 60 min. Post-operative analgesia consisted of iv tramadol 100 mg, and 1g paracetamol iv 3 times daily.
Blood sampling and measurements: Blood samples for M30, M65, AST, and ALT levels were obtained before the beginning of surgery, immediately after the end of surgery, as well as 24 and 48 h postoperatively. The end of surgery was defined as the time at which skin closure was accomplished. For M30 and M65 levels blood samples were kept under room temperature for almost one hour. Serum was separated by centrifugation and 1 ml aliquots were frozen at -80°C until the analysis.
The M30 ELISA and M65-Apoptosense ELISA assays (PEVIVA, Alexis, Grunwald, Germany) were used to measure caspase-cleaved CK 18 and total CK-18, respectively1011. The M30 Apoptosense assay specifically measures a neo-epitope formed by caspase cleavage of CK18 at Asp396 (K18Asp396-NE M30). The specificity of this assay was confirmed via immunoprecipitation of CK-18 fragments in serum samples. M65 ELISA is a solid phase enzyme immunoassay-ELISA that uses two anti-CK18 mouse monoclonal IgG antibodies (clone M6 and clone M5, both IgG2b)12. The microtiter plate provided by the manufacturer has been pre-coated with M6 antibody specific to CK 18. Serum ALT and AST levels were measured by routine hospital laboratory tests.
The primary outcome of the study was the M30 values 24 h postoperatively in the propofol or sevoflurane groups. The secondary outcomes were the M65 levels, the M30/M65 ratio and the ALT and AST levels measured at the same time points with the M30 and M65 markers.
Statistical analysis: The mixed-linear model analyses were run with PROC MIXED command, including CLASS statements, where the variance–covariance structures were given in an unstructured statement. The same mixed-linear model was used to compare the AST and ALT values at each time point between the two groups. Statistical evaluation was performed using SAS 9.1.3 s.p.4. (SAS Institute Inc., USA).
Results
Of the total 67 patients, seven were discharged from the hospital earlier so the 48-h sample was not collected (Figure), thus only 60 patients were included in the final analysis. During anaesthesia none of the patients developed arterial oxygen saturation below 97 per cent or arterial hypotension, thus decrease in systolic arterial pressure more than 20 per cent of the baseline value was obtained before induction of general anaesthesia.
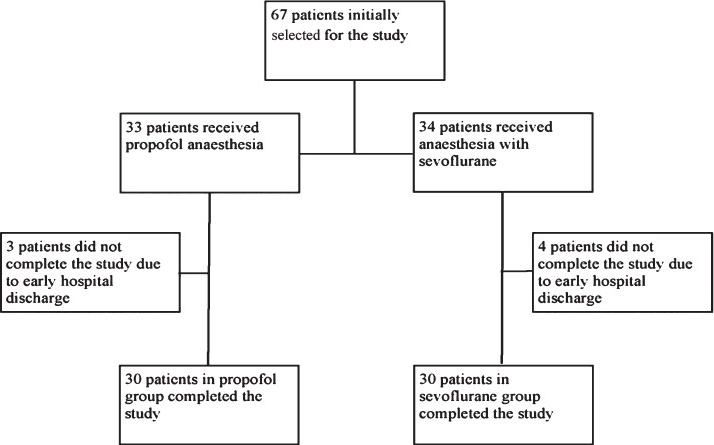
- Flow chart showing the study design.
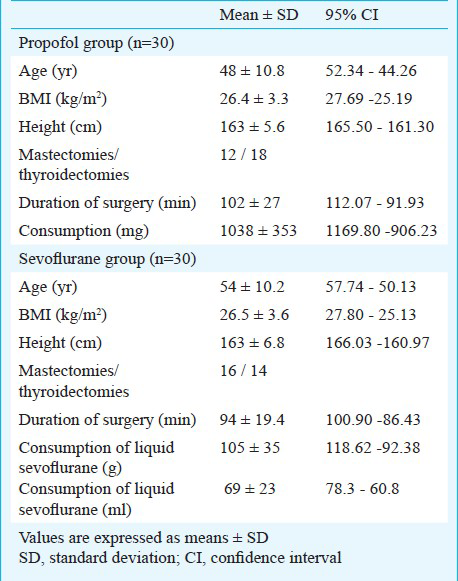
Patient characteristics, duration of surgery and anaesthetic consumption in each group are shown in Table I. No significant changes were observed in the M30, M65 cell death markers or in the M30/M65 ratio immediately after surgery and 24 and 48 h postoperatively (Table II). The ALT and AST enzyme values did not change at the same time points (Table III).
Discussion
Our results showed no changes in the M30 or M65 markers in patients undergoing surgery under propofol or sevoflurane anaesthesia. The serum ALT or AST levels also did not change immediately and 24 and 48 h postoperatively. Propofol administered for minor gynaecological procedures in healthy women had no effect on the ALT, AST or alkaline phosphatase13.
Hepatic glutathione-S-transferase is widely distributed in the liver tissue, allows earlier detection of liver injury and is a more sensitive marker than the ALT and AST. In an earlier study, propofol did not increase the hepatic gluthathione-S-transferase B1 and B2 isoenzyme levels beyond the normal values in patients undergoing plastic surgery lasting more than 10 h anaesthesia14. Ray et al15 reported that sevoflurane anaesthesia in 41 patients undergoing minor or intermediate orthopaedic, nose, throat or eye surgery was associated with increased glutathione-S-transferase concentrations one hour postoperatively but not after 3, 6 and 24 h. Sevoflurane anaesthesia for urological16 or gynaecological17 procedures was associated with increased α-GST levels 60 to 120 min postoperatively, while α-GST levels did not change in women undergoing abdominal hysterectomy under propofol anaesthesia17.
The TNF-related apoptosis inducing ligand (TRAIL) levels increased significantly after sevoflurane anaesthesia for open cholecystectomy when compared to baseline and to TRAIL values measured after propofol or isoflurane anaesthesia18. The caspase-3 did not differ between the three anaesthetics. Significant but similar increases in the ALT and AST were found with the three anaesthetics18. However, in the study by Osman et al18 the type of surgery was a limitation as in cholecystectomy it is hard to distinguish between liver injury due to anaesthetic agent or due to surgery.
The M30 and M65 selected cell-death markers have not been used to assess the effect of general anaesthetics on liver integrity. These markers may predict the outcome of patients with acute liver failure. When total bilirubin was replaced by the M65 in the Model for End-Stage Liver Disease (MELD), the sensitivity to predict survival in patients with acute liver failure was improved19. In patients with acute liver failure due to paracetamol ingestion the M30 levels were increased and were higher in patients who died or received a liver transplant than in spontaneous survivors20. The M65 levels were also increased but did not distinguish between the spontaneous survivors and the patients who died or underwent liver transplantation20.
Several cofactors may increase M30 and M65 markers perioperatively, like liver, gallbladder or pancreatic surgery, drugs, and perhaps fall in liver blood flow due to hypotension. Our patients were haemodynamically stable. Since both groups underwent surface surgery, which does not involve liver injury, and were treated similarly except for the main general anaesthetic, propofol or sevoflurane, a possible increase in the M30 and/or M65 in one group would suggest an apoptotic and/or necrotic effect of the anaesthetic used. As none of the groups exhibited increases in the above markers, there was no indication of apoptosis/necrosis under the study design conditions.
Malignant cells and their subsequent apoptosis may increase the M30 and M65 markers21. Patients scheduled for mastectomy had operable breast cancer, and this might be considered a limitation of the study. But the baseline and subsequently the post-operative values of these markers were within the normal range in all patients. Other limitations of the study were the wide variation of the M30 and M65 values distribution, the relatively short period of measurements, not including possible long term effects of the anaesthetics on the liver beyond the first 48 post-operative hours, and failure to collect samples from seven patients at 48 h due to earlier patient discharge.
Levels of M30 and M65 were measured until 48 h postoperatively. The kinetics of M30 and M65 evaluated as biomarkers of drug induced tumour cell death in rats and in humans with testicular cancer exhibited changes for days after the therapeutic interventions2122. A speculative transient increase in the M30 and/or M65 marker might have occurred at a time point far from the time points of sample collecting. In this case the clinical impact of the anaesthetic regarding a pro- or apoptotic effect would be negligible.
The present study design, despite its limitations suggested that these markers were not altered by the two anaesthetics studied. These results are not applicable to abdominal surgery involving the gall bladder and/or liver, where the hepatic cell injury due to surgery predominates.
In conclusion, under the present study design M30 and M65 markers did not exhibit significant changes related to propofol or sevoflurane anaesthesia in patients undergoing mastectomy or thyroidectomy surgery. Therefore, both agents appear to be equally safe in terms of apoptosis/necrosis. Nevertheless, the markers used showed wide variations in distribution among study patients preventing meaningful conclusions
Acknowledgment
This study was funded from the Department of Anaesthesiology, Aretaieio Hospital, University of Athens and Abbott Laboratories (Hellas) SA, VIOSER SA, and MSD, Greece. Authors thank Mr Darin Peterson for statistical assistance.
Conflict of interest: None.
References
- Induction and mechanism of apoptotic cell death by propofol in HL-60 cells. Acta Anaesthesiol Scand. 2002;46:1068-74.
- [Google Scholar]
- A rare case of propofol-induced acute liver failure and literature review. Case Rep Gastroenterol. 2010;64:57-65.
- [Google Scholar]
- Hepatocellular injury following the administration of propofol. Anesthesiology. 2001;95:1523-4.
- [Google Scholar]
- Sevoflurane hepatotoxicity: a case report of sevoflurane hepatic necrosis and review of the literature. Am J Ther. 2010;17:219-22.
- [Google Scholar]
- A fatal case of fulminant hepatic necrosis following sevoflurane anesthesia. Toxicol Pathol. 2007;35:780-5.
- [Google Scholar]
- Serum levels of caspase-cleaved cytokeratin-18 and mortality are associated in severe septic patients: pilot study. PLoS One. 2014;9(10):e109618.
- [Google Scholar]
- Serum markers of hepatocyte death and apoptosis are non invasive biomarkers of severe fibrosis in patients with alcoholic liver disease. PLoS One. 2011;18(6):e17599.
- [Google Scholar]
- Performance of enhanced liver fibrosis plasma markers in asymptomatic individuals with ZZ α1-antitrypsin deficiency. Eur J Gastroenterol Hepat. 2011;23:716-20.
- [Google Scholar]
- Apoptosis versus necrosis rate as a predictor in acute liver failure following acetaminophen intoxication compared with acute-onchronic liver failure. Liver Int. 2008;28:713-6.
- [Google Scholar]
- A novel high-through-put assay for screening of pro-apoptotic drugs. Invest New Drugs. 2002;20:253-9.
- [Google Scholar]
- A novel assay for discovery and characterization of pro-apoptotic drugs and for monitoring apoptosis in patient sera. Apoptosis. 2003;8:263-8.
- [Google Scholar]
- Differentiation between cell death modes using measurements of different soluble forms of extracellular cytokeratin 18. Cancer Res. 2004;64:1751-6.
- [Google Scholar]
- Changes in liver function tests after propofol (‘Diprivan’) Postgrad Med J. 1985;61(Suppl 3):160-1.
- [Google Scholar]
- Comparison of the effects of isoflurane and propofol on hepatic glutathione-S-transferase concentrations during and after prolonged anaesthesia. Br J Anaesth. 1994;72:559-601.
- [Google Scholar]
- Effect of sevoflurane anaesthesia on plasma concentrations of glutathione S-transferase. Br J Anaesth. 1996;77:404-7.
- [Google Scholar]
- Hepatocellular integrity during anesthesia with induced hypotension. J Egypt Parasitol. 2009;39:641-51.
- [Google Scholar]
- Effect of regional epidural ropivacaine anesthesia on α-glutathione-S-transferase: Comparison with low flow sevoflurane and total intravenous propofol anesthesia. J Biol Sci. 2004;4:398-404.
- [Google Scholar]
- In vivo effects of different anesthetic agents on apoptosis. Korean J Anaesthesiol. 2012;63:18-24.
- [Google Scholar]
- Cytokeratin 18-based modification of the MELD score improves prediction of spontaneous survival after acute liver injury. J Hepatol. 2010;53:639-47.
- [Google Scholar]
- Circulating apoptotic and necrotic cell death markers in patients with acute liver injury. Liver Int. 2011;31:1127-36.
- [Google Scholar]
- Clinical Evaluation of M30 and M65 ELISA cell death assays as circulating biomarkers in a drug-sensitive tumor, testicular cancer. Neoplasia. 2008;10:1041-8.
- [Google Scholar]
- Preclinical evaluation of M30 and M65 ELISA as biomarkers of drug induced tumor cell death and antitumor activity. Mol Cancer Ther. 2008;7:455-63.
- [Google Scholar]






