Translate this page into:
Profile of urinary tract infections in paediatric patients
Reprint requests: Dr Jharna Mandal, Department of Microbiology, Jawaharlal Institute of Postgraduate Medical Education & Research (JIPMER), Puducherry 605 006, India e-mail: drjharna@gmail.com
-
Received: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
This cross-sectional study was conducted at a tertiary care centre in Puducherry, south India, with the aim of finding the profile of the paediatric urinary tract infection (UTI), bacterial pathogens involved, and also to observe vesicoureteric reflux (VUR) and renal scarring in these patients.
Methods:
A total of 524 paediatric patients ≤13 yr, suspected to have UTI, were included in the study. Urine samples were collected, processed for uropathogen isolation and antibiotic susceptibility test was performed as per the Clinical and Laboratory Standards Institute (CLSI) guidelines. Thirty two culture proven children with UTI underwent micturating cysto-urethrography (MCU) and dimercaptosuccinic acid (DMSA) scanning was done for 69 children.
Results:
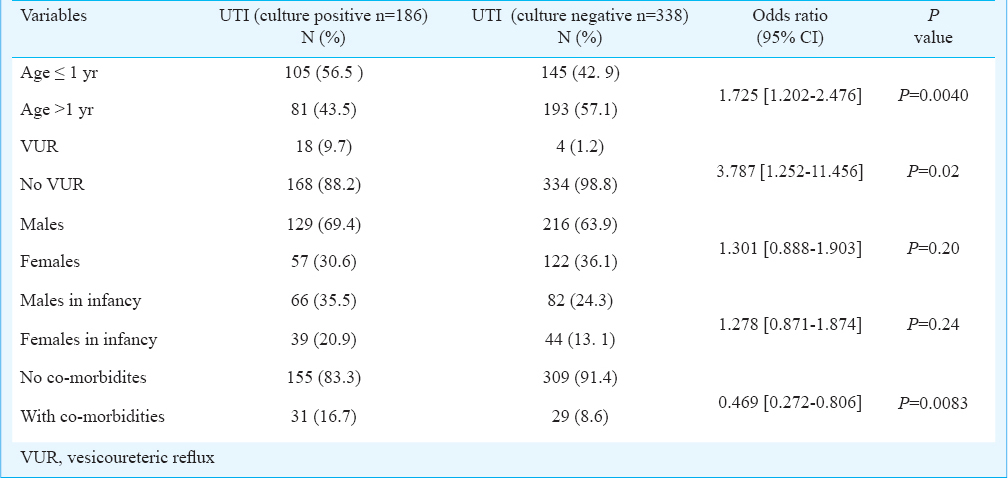
of the 524 children, 186 (35.4%) had culture proven UTI with 105 (56.4%) being infants, 50 (27.4%) between 1-5 yr, 30 (16.12%) between 5-13 yr and 129 (69.35%) males. Posterior urethral valve (PUV) was noted in three, hydronephrosis in one, VUR in 18 and renal scarring in 33. VUR as well as renal scarring were more in males >1 yr of age. A significant association (P=0.0054) was noted with a combined sensitivity and specificity of these investigations being 83 and 90 per cent, respectively of the MCU and DMSA scans for detecting VUR. Escherichia coli was the most common pathogen isolated, sensitive to nitrofurantoin, followed by cefoperazone-sulbactam, aminoglycosides and meropenem.
Interpretation & conclusions:
Our results indicate that UTI varies with age and gender and extensive evaluation is required in boys under one year of age with UTI. This study also highlights the better efficacy of aminoglycosides, cefoperazone-sulbactam and nitrofurantoin in vitro compared with meropenem in Gram–negative uropathogens.
Keywords
Cefoperazone-sulbactum
children
meropenem
posterior urethral valve (PUV)
urinary tract infection (UTI)
vesicoureteric reflux
In children most often urinary tract infection (UTI) manifests as fever of unknown origin. The clinical presentation of UTI in infants and young children can vary from occult and undiagnosed fever to gastrointestinal manifestations as well as upper and lower urinary tract symptoms whereas, in older children symptoms referring to the urinary tract may be observed1. Incidence of UTI varies with age of the child. Five per cent of children below two years with fever have UTI. In the first year of life, especially in the first three months, UTI is seen more commonly in boys (3.7%) than in girls (2%). Thereafter, the UTI has been reported to be among three per cent girls and 1.1 per cent boys1. Children are at risk of developing UTI due to certain anatomic and physiologic factors among which vesicoureteric reflux (VUR) is the most common. VUR leads to repeated infections and other complications like chronic pyelonephritis and eventual renal scarring which are components of reflux nephropathy2. Hence, it is important to diagnose this condition at the appropriate time as it is a preventable cause of renal damage.
Bacteria are common causes of UTI in children with Escherichia coli being the most commonly isolated pathogen. Susceptibility patterns of the bacterial isolates vary with geographic region and act as a reference for guiding the empirical therapy. The aetiology of paediatric UTI and the antibiotic susceptibility of urinary pathogens in both the community and hospitals have been changing, and drug resistance has become a major problem3456. With this background, the present study was conducted to observe the profile of the paediatric UTI, to find out the bacterial pathogens involved and their antimicrobial susceptibility pattern, and also to get a short overview of VUR and consecutive renal scarring in these patients at a tertiary care centre in south India.
Material & Methods
This cross-sectional study was undertaken in the department of Microbiology in collaboration with the departments of Pediatrics, Radiodiagnosis and Nuclear Medicine, Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER), Puducherry, India. The study protocol was approved by the ethics committee of the institute.
Patients: All consecutive paediatric patients (children ≤ 13 yr) suspected to have UTI within a period of three months (from May to July 2013) were included after obtaining informed written consent from their guardians/parents. Background information was collected from the guardian regarding the demographic details of the patient, previous incidence of UTI, family history of UTI/VUR, drug intake, previous interventions, and any other complaints.
Microbiological and radiological methods: The urine samples collected from patients were processed according to the standard microbiological procedures with a calibrated one microlitre loop using the semi-quantitative method of plating onto cysteine lactose electrolyte deficient medium (Hi- Media, Mumbai, India) to isolate the uropathogens. The antibiotic sensitivity testing was performed using the Kirby-Bauer method7 as per the Clinical Laboratory Standards Institute (CLSI)8910. Simultaneously, the follow up data were collected for the micturating cysto-urethrography (MCU) and the dimercaptosuccinic acid (DMSA) scan reports, respectively of these patients.
Statistical analysis: All data were expressed in percentages, Chi square test with Yates correction was used to analyze the data, odds ratios were calculated using Woolf's correction.
Results & Discussion
Of the 524 children with suspected UTI included in this study, 186 (35.4%) were found to be culture positive. The commonest type was (85%) simple UTI (the uncomplicated community acquired UTI). Among the 186 children with culture proven UTI, 32 underwent MCU scan, of whom, 18 (56.25%) had VUR (6 bilateral and 12 unilateral). Renal scarring was noted in 33 (47.8%) of the 69 children who underwent DMSA scan. A significant association (P=0.0054) was noted with a combined sensitivity and specificity of these investigations being 83 and 90 per cent, respectively of the MCU and DMSA scans for detecting VUR. Of the culture proven cases of UTI (n=186), 114 (61.2%) children presented to the Paediatrics outpatient department (OPD), 32 (17. 2%) were admitted into the paediatric ward, 25 (13.44%) needed operative management and 15 (8%) needed intensive care.
The number of episodes of UTI were maximum in children ≤ one yr of age (Table I). Majority of the children involved were boys (129, 69.4%) (Table I). VUR as well as renal scarring were more in males than in females (data not shown in Table I). Hence, extensive evaluation in boys over one year with UTI is required. Our observations were concordant with an earlier report11.
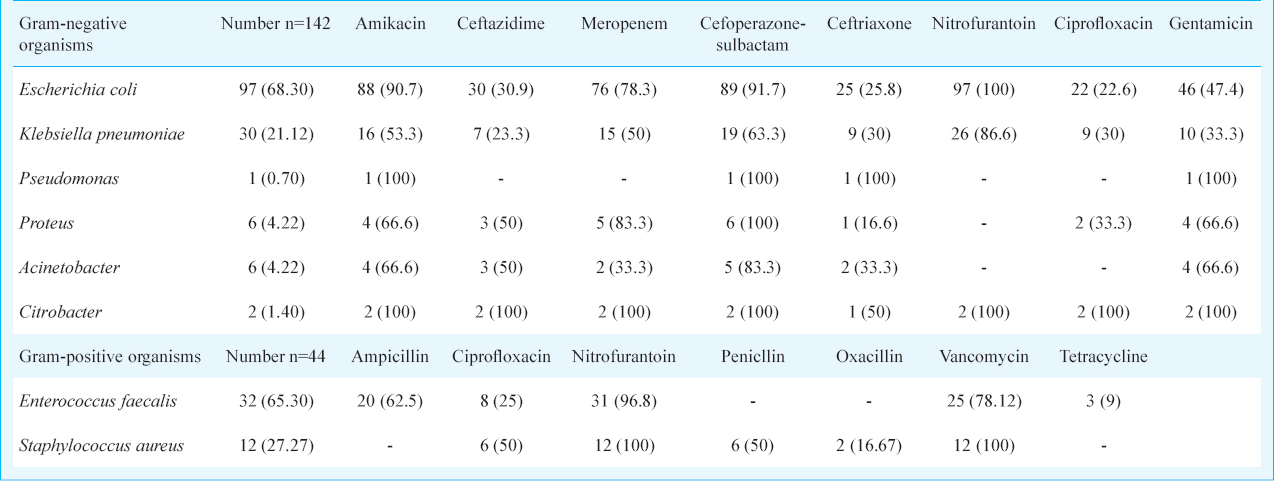
The major uropathogens isolated were Escherichia coli, followed by Enterococcus faecalis and Klebsiella pneumoniae (Table II). Majority of the E. coli and Klebsiella isolates were sensitive to nitrofurantoin, followed by cefoperazone-sulbactam, aminoglycosides and meropenem. Our findings were different from an earlier study from north India4 but similar to others56. The sensitivity patterns of the most commonly isolated pathogens indicated that the isolates obtained from the OPD were more susceptible to most of the antibiotics than in the ward followed by the paedric intensive case unit (PICU). Both E.coli and K. pneumoniae were sensitive to nitrofurantoin, amikacin, cefoperazone-sulbactam followed by meropenem. Among the Gram-positive organisms, Enterococcus faecalis was the most frequently isolated pathogen. Vancomycin resistant enterococci were isolated from seven children who were admitted to the PICU, three of whom had posterior urethral valve (PUV), one had catheter induced UTI, one had undergone surgical intervention for PUV, while in the remaining two children no risk factor could be ascertained. Amongst the staphylococci, 33.3 per cent were MRSA (methicillin resistant Staphylococcus aureus). Most of the children with UTI associated with VUR had significant bacteriuria with counts above 100,000 cfu/ml, similar to earlier reports12131415.
In conclusion, our study shows that UTI varies with age and gender and, therefore, extensive evaluation is required in boys under one year of age with UTI. This study also highlights the better efficacy of aminoglycosides, cefoperazone-sulbactam and nitrofurantoin in vitro compared with meropenem in Gram–negative uropathogens. Long term studies on a large sample of children need to be planned to understand the disease process better in terms of the interplay between the host and microbial factors.
References
- European Association of Urology (UAE). Guidelines on urological infections. In: Grabe M, Bjerklund-johansen TE, Botto H, Wullt B, Cek M, Naber KG, eds. Arnhem. The Netherlands: UAE; 2013. p. :42-9.
- [Google Scholar]
- Vesicoureteric reflux: screening of first degree relatives. Arch Dis Child. 1989;64:1538-41.
- [Google Scholar]
- Paediatric urinary tract infections in a tertiary care centre from north India. Indian J Med Res. 2010;131:101-5.
- [Google Scholar]
- Evaluation of extended spectrum beta lactamase in urinary isolates. Indian J Med Res. 2004;120:553-6.
- [Google Scholar]
- Bacteriology and antibiotic resistance pattern in community acquired urinary tract infections. Indian Pediatr. 2013;50:707.
- [Google Scholar]
- Antibiotic susceptibility testing by a standardized single disk method. Am J Clin Pathol. 1966;45:493-6.
- [Google Scholar]
- Laboratory strategy in the diagnosis of infective syndromes. In: Collee JG, Fraser AG, Marmion BP, Simmons A, eds. Mackie & McCartney practical medical microbiology (14th ed). New York: Churchill Livingstone; 1999. p. :84-90.
- [Google Scholar]
- Clinical and Laboratory Standards Institute (CLSI). Performance standards for antimicrobial susceptibility testing; 22nd informational supplement. CLSI document M100-S22. Wayne, Pa: CLSI; 2012.
- [Google Scholar]
- Revised statement on management of urinary tract infections. Indian Pediatr. 2011;48:709-17.
- [Google Scholar]
- Evaluation of the use of DMSA in culture positive UTI and culture negative acute pyelonephritis. Indian Pediatr. 2005;42:691-6.
- [Google Scholar]
- Urinary tract infection in children: Epidemiology, evaluation and management. Pediatr Clin North Am. 1997;44:1133-69.
- [Google Scholar]
- Diagnosis and management of pediatric urinary tract infections. Clin Microbiol Rev. 2005;18:417-22.
- [Google Scholar]
- American Academy of Pediatrics Urinary tract infection: Clinical practice guideline for the diagnosis and management of the initial UTI in febrile infants and children 2 to 24 months. Steering Committee of American Academy of Pediatrics. Pediatrics. 2011;128:595-610.
- [Google Scholar]
- Urinary tract infection. In: Srivastava RN, Bagga A, eds. Pediatric nephrology (5th ed). New Delhi: Jaypee Brothers; 2011. p. :273-300.
- [Google Scholar]






