Translate this page into:
Primary parachordoma in the trachea: An unusual cause of dyspnoea
*For correspondence: zhangxiaoju1010@hotmail.com
-
Received: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
A 42 yr old man† was hospitalized in August 2015 in the Respiratory and Critical Care Medicine ward, Zhengzhou University People's Hospital, Zhengzhou, Henan, PR China, with long-lasting (more than one year), gradually worsening and drug-resistant dyspnoea. The physical examination revealed inspiratory dyspnoea. Computed tomography scan of chest showed a lesion measuring 1.5 cm × 1 cm in trachea with normal bronchus and lung (Fig. 1A). Bronchoscopy demonstrated a circumscribed and homogeneous mass with wide base (Fig. 1B). Subsequently, the neodymium-doped yttrium aluminium garnet (Nd-YAG) laser was used to resect the obstructive lesion and moderate bleeding during the operation. The argon plasma coagulation (APC) was used to stop the bleeding. The definitive pathology confirmed the diagnosis of parachordoma. There were glomoid rounded cells and spindle cells were embedded in a matrix that varied from myxoid to densely hyaline (Fig. 1C & D). Immunohistochemistry exhibited positive expression of cytokeratins 8/18 (CK8/18), epithelial membrane antigen (EMA), protein gene product 9.5 (PGP 9.5), S-100, vimentin, alcian blue periodic acid-Schiff (AB-PAS) and negative expression of synaptophysin (SYN) and neuron specific enolase (NSE) (Fig. 2). The EWS RNA binding protein 1 (EWSR1) gene break-apart rearrangement results were negative. After the therapy, the patient's symptom of dyspnoea disappeared, and on two years’ follow up, there was no recurrence of symptoms, or tumour on bronchoscopy. The prognosis depends mainly on the possible resection of the lesion and the stage, like in other primary tracheal tumours.
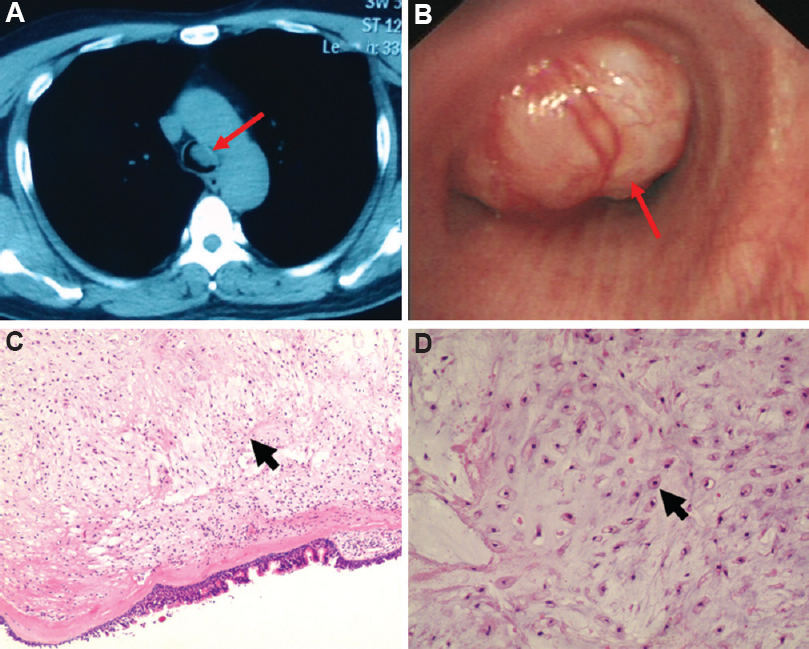
- (A) Computed tomography scan showed a lesion in trachea (red arrow). (B) Bronchoscopy found a mass in the trachea (red arrow). (C) Hematoxylin and eosin (H and E), ×10. (D) H and E, ×100 (Glomoid rounded cells and spindle cells were shown with black arrows).
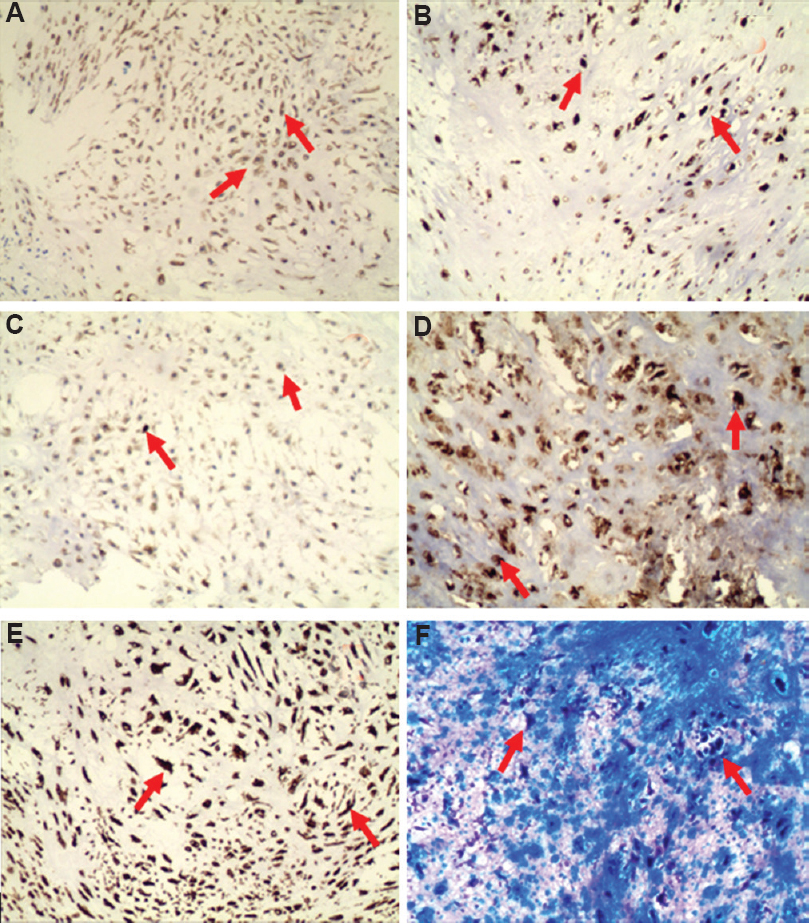
- Immunohistochemistry exhibited positive expression (red arrows) of the present tracheal tumor. (A) cytokeratins 8/18 CK8/18 (×100), (3,3'-diaminobenzidine); (B) epithelial membrane antigen (EMA) (×100), (DAB); (C) protein gene product 9.5 (PGP 9.5 ×100), (DAB); (D) S-100 (×100), (DAB); (E) Vimentin (×100), (DAB); (F) Alcian blue periodic acid-Schiff (AB-PAS ×100).
Acknowledgment
Authors acknowledge Dr HongJian Xie, the pathologist for the confirmation of the case and Dr Olajuyin Ayobami Matthew for improving the manuscript.
Conflicts of Interest: None.





