Translate this page into:
Prevention & management of snakebite envenomation: A qualitative study on perspectives & practices in Maharashtra & Odisha
For correspondence: Dr Rahul Gajbhiye, Clinical Research Laboratory, ICMR-National Institute for Research in Reproductive and Child Health, Mumbai 400 012, Maharashtra, India e-mail: gajbhiyer@nirrch.res.in
-
Received: ,
Abstract
Background & objectives
Snakebite envenoming (SBE) is a major public health concern, with India bearing the highest global burden of SBE-related deaths. SBE is concentrated in rural and tribal regions of India, where the knowledge, attitude and behaviour of the dwelling communities largely influence mortality and morbidity. Understanding these factors is crucial to designing effective SBE prevention and management strategies. The present study’s objective was to document the perspectives of community members and practices in selected blocks of Maharashtra and Odisha States regarding SBE prevention, first aid and health-seeking behaviour.
Methods
Between March and April 2022, 28 focus group discussions (FGDs) were conducted. Study sites included Shahapur block in Thane district, Aheri block in Gadchiroli district of Maharashtra, and Khordha block in Khordha district, Kasipur block in Rayagada district of Odisha. Separate FGDs were held for males (n=14) and females (n=14), involving about 8-16 participants above 18 yr. All discussions were audio recorded, and a grounded theory approach was employed to identify key themes from the translated transcripts.
Results
The findings of this study revealed a variety of perspectives and practices determining the SBE burden at the study sites. The findings included insufficient knowledge about snake species and their nature of toxicity, use of non-scientific first aid techniques, inaccessible health care and reliance on traditional healers, non-utilization of prevention methods, varied cultural beliefs and practices, and differential treatments based on gender. The findings have been collated in two simplistic frameworks; barriers to effective prevention and barriers to effective management.
Interpretation & conclusions
SBE burden results from a complex interplay between socioeconomic, cultural, and demographic factors, necessitating a collaborative inter-sectoral effort for adequate control. Through crucial regional inputs and the barriers to prevention and management models, this study provides critical insights and priority intervention areas to strengthen India’s upcoming National Action Plan for Prevention and Control of Snakebite Envenoming (NAPSE) in all high-burden States.
Keywords
Envenomation
focus group discussion
India
knowledge
attitude and practices
mortality
morbidity
snakebites
Snakebite envenoming (SBE) remains a significant global public health issue, causing 81,000 to 138,000 fatalities annually while leaving at least three times more individuals disabled1,2. South Asia and particularly India are affected by this burden noticeably, contributing to 86 and 70 per cent of global SBE deaths, respectively3. Despite some progress in reducing SBE mortality over the last three decades, the current rate of decline falls short of the World Health Organization’s (WHO) target to halve SBE deaths by 20303. Notably, low- and low-to-middle-income countries (LICs and LMICs) experience the greatest impact4, where farmers, migrants, and their families are mainly affected5,6. The situation is further compounded in rural areas by limited healthcare access, lack of health personnel, unavailability of anti-venom, and reliance on traditional methods7-10. Moreover, geographical, meteorological, and cultural factors also play a significant role in determining the burden and impact of SBE in specific regions10-12.
In India, there are substantial regional variations in SBE deaths. Mortality figures ranged from 2,400 in the north-eastern States to 82,900 in Andhra Pradesh and 153,600 in Uttar Pradesh between 2001 and 201413. This disparity in the burden points towards differences in the frequencies of human-snake conflict, gaps in understanding the prevention aspects and varied health-seeking behaviour. A better understanding of these lacunae can offer crucial insights to design and implement SBE prevention and management strategies effectively.
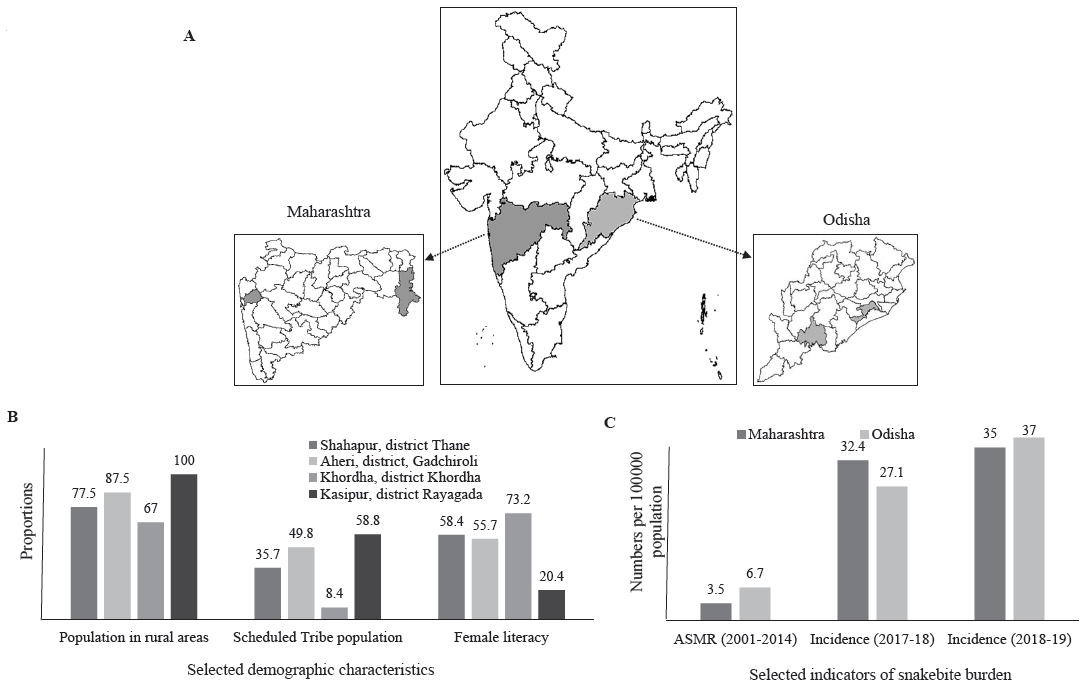
Maharashtra and Odisha States in India have faced a high burden of SBE since the pre-independence era14. The age-standardized mortality rate in Maharashtra and Odisha between 2001 and 2014 was 3.5 and 6.7 per 100,000 population, respectively13. The total number of deaths due to snakebites from 2001-14 was 56,000 in Maharashtra and 40,300 in Odisha, amounting to around 12 per cent of the total snakebite deaths in India during the same period13. The Health Management Information System (HMIS) has reported increased SBE incidence in both States from 2017-18 to 2018-1915. In 2019, the age-standardized death rate for Maharashtra and Odisha was 3.3 and 5, respectively, indicating little reduction from 2001-14 estimates3. Despite having a high burden, gaps in understanding of SBE in these two States, especially in districts with substantial tribal populations, limit the SBE control efforts.
To address these gaps, the Indian Council of Medical Research (ICMR) National Task Force on snakebite recommended a national implementation research project on community engagement and system strengthening to prevent and manage snakebite envenomation in Maharashtra and Odisha16. As part of this research, we conducted the present qualitative study to understand and document the perspectives and practices of communities living in high-burden districts regarding SBE prevention and management in these two States.
Material & Methods
The present study was undertaken by the Clinical Research Laboratory at ICMR-National Institute of Research in Reproductive and Child Health (NIRRCH), Mumbai in Maharashtra and Epidemiology Division of the ICMR-Regional Medical Research Centre (RMRC), Bhubaneswar in Odisha. The study was registered under the Clinical Trial Registry India (CTRI/2021/11/038137). It was approved by the Institutional Ethics Committee of ICMR-NIRRCH, Mumbai for Maharashtra and ICMR-RMRC, Bhubaneswar for Odisha. Before the study, permission was obtained from the Director of the Public Health Departments in Maharashtra as well as Odisha. This study was conducted in four blocks: Shahapur block of Thane district, Aheri block of Gadchiroli district in Maharashtra, Khordha block of Khordha district and Kasipur block of Rayagada district in Odisha. Their location and demographic characteristics are given in Figure 1.
-
(A) Map of Maharashtra and Odisha States in India highlighting the study districts. (B) Selected demographic characteristics of study blocks (numbers are proportions). (C) Selected indicators depicting snakebite burden in both States (numbers per 100000 population). ASMR – Age Standardized Mortality Rate. Source: Maps generated in R-studio based on Administrative Boundary Database provided by Onlinemaps portal of Survey of India, Ministry of Science & Technology (https://onlinemaps.surveyofindia.gov.in/Home.aspx).
Data collection
Data was collected using focus group discussions (FGDs). The study aimed to explore the understanding and practices of communities affected by snakebites. As such, the flexibility provided by the FGD guide proved vital in knowing similar and contrasting opinions from the respondents. FGDs also allowed for probing and enhancing the discussion for better extraction of information. Literature suggests that, the SBE burden is shaped by complex socio-cultural dynamics4,7. To get the complete picture of these factors, separate FGDs were conducted for men and women. The Primary Health Centres (PHCs) are typically the first contact point for the community with the public healthcare system for SBE management. The availability and accessibility of the PHCs, hence, influence the health-seeking behaviour of communities. The awareness intervention for this study was also provided through the PHCs. In this regard, conducting at least six FGDs per block was decided, giving equal representation to each PHC area. However, this number was kept flexible for gathering new information until theoretical saturation. Village selection was done randomly. The ASHA disseminated information about the conduct of an FGD in the village, and people were invited to participate. Participation in the FGDs was voluntary, and individuals above 18 yr who were residents of the respective village for more than six months were included.
Focused group discussions
The FGD guide was developed based on previous experience7 and a literature review of qualitative studies on SBE burden. It underwent critical review by national SBE experts (Supplementary Figure & Annexure). The revised guide was translated into local languages (Marathi and Oriya) and approved by language experts. Project Technical Officers (PTOs) conducted the FGDs (male PTOs - MG, GB, JPD, female PTO - BM). To ensure quality and uniformity, the PTOs received prior training, and pilot FGDs were conducted. No prior personal relationship existed between the research staff and the study participants. Before each FGD, the PTOs introduced themselves, outlined the purpose and process of the discussion, and obtained written informed consent from willing participants. A moderator facilitated each FGD while an assistant took notes of the discussion. The discussions were audio recorded and conducted at convenient locations, such as community halls and Anganwadi centres (Supplementary Figure).
Data analysis
The constructivist or interpretative worldview of the authors believes that truth is relative and context shapes its interpretation17. Hence, the data analysis and interpretation were carried out from this standpoint. The audio recordings were transcribed verbatim, anonymized, and translated to English after proofreading by four members (MG, GB, BM, JPD) to ensure accuracy and minimize content loss. A sample of the translations was cross-checked by a senior member (HM) for errors and typographical errors. Notes taken by the assistant were used to supplement the transcripts. Two members (HM, RG) independently carried out open coding of the transcripts line-by-line. All coded transcripts were critically reviewed for consistency and accuracy by senior members (HB, SDM). A grounded theory approach explored the respondents’ beliefs, practices and experiences. This approach was particularly relevant as this topic had not been previously studied in the population group18. Themes were not defined a priori but were extracted by clustering the codes. Senior members (AM, SP, GS) independently reviewed and refined the list of emerging themes. The interpretations and conclusions were discussed with all authors to ensure the credibility and conformability of the findings.
Results
A total of 28 FGDs were conducted, 16 in Maharashtra and 12 in Odisha. Four additional FGDs were conducted in Maharashtra, two per study block, as data saturation was not reached with the proposed six FGDs per block. A total of 359 individuals participated, of which 212 (59.1%) were females. Each FGD had 13 respondents (median) and lasted about 65 min. Around one fourth of the respondents had no formal education, and only about six percent had studied beyond higher secondary. More than half (55.4%) of the respondents were engaged in farming; about 18 per cent were labourers, while about 17.5 per cent were unemployed (Table I).
| Parameter | Maharashtra | Odisha | Total |
|---|---|---|---|
| Respondents, n (%) | 202 | 157 | 359 |
| Male | 90 (44.6) | 57 (36.3) | 147 (40.9) |
| Female | 112 (55.4) | 100 (63.7) | 212 (59.1) |
| FGD duration (min) | |||
| Mean | 72 | 56.7 | 64.4 |
| Range | 50-100 | 50-75 | 50-100 |
| Respondents per FGD | |||
| Median | 13 | 13 | 13 |
| Range | 9 to 16 | 8 to 16 | 8 to 16 |
| Age (yr) | |||
| Mean | 38.2 | 38.8 | 38.5 |
| Mean - male respondents | 35.5 | 37.3 | 36.2 |
| Mean - female respondents | 40.3 | 39.6 | 40 |
| Marital status, n (%) | |||
| Married | 179 (88.6) | 115 (73.2) | 294 (81.9) |
| Unmarried | 23 (11.4) | 42 (26.8) | 65 (18.1) |
| Level of education, n (%) | |||
| No formal education | 84 (41.6) | 10 (6.4) | 94 (26.1) |
| Primary | 13 (6.4) | 21 (13.4) | 34 (9.5) |
| Middle school | 30 (14.9) | 48 (30.6) | 78 (21.7) |
| High school | 42 (20.8) | 47 (29.9) | 89 (24.8) |
| Higher Secondary | 21 (10.4) | 23 (14.6) | 44 (12.3) |
| Graduate | 12 (5.9) | 8 (5.1) | 20 (5.6) |
| Occupation, n (%) | |||
| Farmer | 124 (61.4) | 75 (47.8) | 199 (55.4) |
| Labour | 63 (31.2) | 0 (0) | 63 (17.5) |
| Private job | 6 (3) | 7 (4.5) | 13 (3.6) |
| Student | 5 (2.5) | 17 (10.8) | 22 (6.1) |
| Unemployed | 4 (1.9) | 58 (36.9) | 62 (17.4) |
Our data revealed a variety of perspectives and practices regarding SBE across the two States. The findings were clubbed into the following broad categories: (i) knowledge about snake species and their nature of toxicity; (ii) non-scientific first aid techniques; (iii) factors influencing health-seeking behaviour; (iv) non-utilization of prevention methods; (v) traditional beliefs and practices, and (vi) gender aspects influencing practices. The findings of this study were collated in the form of two simplistic frameworks, namely, barriers to effective prevention for the communities and barriers to effective management for the communities, health systems and policymakers.
Knowledge about snake species and their nature of toxicity
It was found that knowledge about different species of snakes varied considerably among the responders. When asked about the identifiable features of the ‘big four’, the response was positive and accurate. Distinctive features attributed were the hood and ‘U’ mark (known as Kathau sign in Oriya) for Indian cobra, coin-shaped markings on the ‘fat’ body of Russell’s viper, stripes for the common krait and thin red body for saw-scaled viper. Respondents belonging to the Madiya community, a Particularly Vulnerable Tribal Group (PVTG) in Aheri, aptly labelled the common krait as Narkakalle, meaning the one who enters the night like a thief (Supplementary Table).
Misconceptions, particularly regarding the venomous nature of the snakes, were reported. A majority of respondents considered the Indian rock python venomous. The misconception notably extended to the vine snake and the Forsten’s cat snake, considered mildly venomous for praying but not for humans. In Kasipur, respondents believed that all snakes, except water snakes, were venomous and hid in trees for camouflage.
Swelling of the bitten area, bleeding, and froth coming out of the mouth were reported as symptoms of venomous snakebite in Maharashtra, while severe head reeling, dizziness and fatigue were reported in Odisha. The same symptoms with a milder intensity were attributed to non-venomous snakebites in both States. The venomous nature was reported to impact the duration of symptoms.
“Symptoms are the same. But swelling and bleeding due to a venomous snake remains for at least 10-12 days. Non-venomous bite, everything goes down immediately” (31 yr male, Shahapur).
In Odisha, all the snake species dwelling near or in water were considered non-venomous, and non-venomous snakes were reported never to bite.
“The non-venomous (snake) will never bite. Only venomous does” (26 yr male, Khordha).
Respondents identified various locations, such as ditches, pits, tree trunks, burrows, ant hills, water bodies, paddy fields, piles of woods, tall grass, forested areas, and residential gardens, as preferred hiding places for snakes. Monsoon (June to September) was reported as the breeding season, leading to increased human-snake interactions.
“Some lay eggs, some give birth. This happens in the monsoons, so their number increases” (28 yr male, Shahapur).
Respondents from both States preferred to kill the biting snake. This was preceded by a notion that the dead snake must be presented at a healthcare facility.
“Without seeing the snake, the doctor cannot start the medication” (38 yr female, Aheri).
Non-scientific first aid techniques
Tying a tourniquet above the bite site was the preferred first aid to mitigate venom spread. In Maharashtra, a cloth or ribbon was commonly used, whereas in Odisha, a wheat or rice stem was preferred. Incising the bitten area with a blade or knife was reported to facilitate venom expulsion along with the blood.
In Kasipur, a first aid method involved repeated pouring of cold water over the victim’s head on the premises of a Naag Mandir (snake temple). This practice was mandatory before seeking any traditional treatment. Apart from a tourniquet, respondents provided first aid by calming the victim down and forcing the victim to lay in bed in a straight (supine) position. In Shahapur, especially after a night bite and if it was impossible to reach a healthcare facility, the village elders kept the victim awake.
“Calm the person down; keep talking and don’t let him/her sleep. If he/she is frightened, the venom will spread faster” (40 yr female, Shahapur; 42 yr male, Shahapur).
Factors influencing Health Seeking Behaviour
Most respondents in both States expressed their belief in the health system for snakebite management while also maintaining faith in traditional healers. In Maharashtra, prior positive treatment experiences, at-home services, and cost-free treatment influenced victims to seek traditional management. In Odisha, respondents shared instances where healers would refer the victims to the health system when their ability to manage the situation reached its limits.
“We go to the priest first. He tells us if there is a need to go to the hospital; He will tell us what kind of snake has bitten and whether he can or cannot treat” (54 yr male, Khordha).
In Maharashtra, a common practice involved combining modern medical treatment with traditional medicines for better outcomes. Challenges in seeking treatment from healthcare facilities in both States included non-available doctors and health staff, limited bed availability, and time-consuming and expensive commutes. Odisha faced additional issues of recurrent referrals without adequate amenities, even at higher centres. Lack of accountability was a critical factor undermining respondents’ confidence in the health system. Multiple high-risk consents were reportedly taken before initiating treatment at all study sites.
“They take our signature first and then give saline. They do not tell what is written” (48 yr male, Shahapur). “The doctor only says that this is a critical case and needs referral; victims die on the route to the hospital” (45 yr female, Khordha).
Respondents believed taking victims directly to higher centres was the right approach, as Primary Health Centres (PHCs) often referred them without providing treatment. However, utilization of health facilities was limited due to high treatment costs. Accessibility and availability of ambulances for transferring critical patients also impacted the uptake of healthcare services. Respondents highlighted the challenges of accessing medical care at night and the lack of mobile connectivity to call an ambulance.
“Snakebite occurs at night. We do not have any vehicles to go to the hospital. There is no mobile connectivity in the village to call an ambulance. So, we take gavthi upchar (traditional medicine) and take the victim to the hospital in the morning. The doctors shout about why we did not bring the victim earlier. How should we bring?” (50 yr male, Shahapur).
Differences of opinions among respondents regarding the most effective mode of snakebite treatment are depicted in Figure 2.
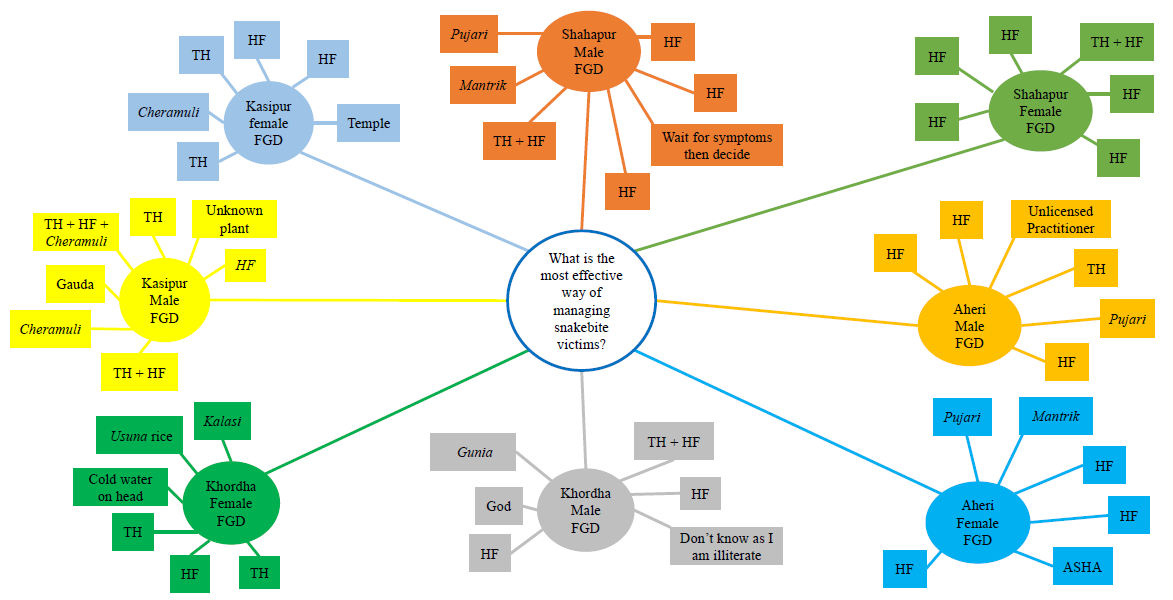
- Different perspectives regarding effective method for the management of snakebites among male and female respondents in selected FGDs in the study blocks. Note: Cheramuli, a medicinal plant; Usuna, a local rice breed; Gunia, Pujari, Kalasi, Gauda, & Mantrik are different names of traditional healers using non-herbal ways for managing snakebite victims. HF, health facility; TH, traditional healer.
Non-utilization of prevention methods
Respondents in both States demonstrated awareness of standard preventive measures, such as wearing gum boots in paddy fields, using a torch at night, and carrying a wooden stick while walking through tall grass. However, these methods were severely limited due to financial constraints and difficulties while working.
“We know people who were bitten on the legs while working. We know long boots should be used. But where do we get the money for them? Four of our family members work together in our field. We cannot buy four pairs. If we buy the cheap ones, they get soggy and heavy, and then we cannot work. So, what should we do?” (32 yr male, Kasipur; 36 yr male Aheri)
Moderator, “What about using a torch at night?”
“Few have it, maximum don’t. Now, some use mobile torches. But we don’t have electricity to charge our mobile regularly (laughs).” (29 yr male, Shahapur)
None of the respondents were aware of using mosquito nets against nighttime snakebites. In Maharashtra, respondents reported using Thimet powder (an insecticide containing Phorate as the active ingredient) as a snake repellent. In Odisha, black phenyl (a common disinfectant) was mentioned to have a similar effect.
In Maharashtra, snakebites during open defecation were not uncommon, especially among women who practiced open defecation in fields and forests between 4 AM and 6 AM, making them vulnerable to snake encounters. Participants in Odisha preferred going out for open defecation despite having toilets in their homes.
“Government people came and constructed the toilet in our homes. We did not ask for it. We prefer the open spaces” (43 yr male, Kasipur).
Traditional beliefs and practices
Snakes have been revered in the Indian population for centuries. This has given rise to many beliefs, myths, and misunderstandings regarding snakes, snakebites, first aid, management, and prevention. Our findings reveal that such myths heavily influenced people’s perspectives and practices.
Red chilli powder or spices were used to assess the victim’s taste sensation to distinguish venomous and non-venomous snakebites.
“Feed chilli to the victim. If the taste is gone, then it is venomous, and if the chilli is red hot, then non-venomous” (30 yr male, Aheri; 39 yr female, Shahapur; 47 yr male, Khordha; 43 yr female, Kasipur).
In Odisha, a procedure called Bhanguni requires the victim to ingest the roots and leaves of a plant. Recurrent vomiting after ingestion indicated a nasty bite. It was believed that the venom came out with the vomit, prompting repeated ingestions. However, the healers never disclosed specific details of the plant. An herbal plant, Cheramuli, was frequently used in Odisha to reduce venom effects. No herbal plant use was reported from Maharashtra.
Participants in Aheri and Kasipur described a process where the snake is wounded for the purpose of taking it to a priest. After administering the traditional medicine, it is killed. Table II depicts people’s shared beliefs and practices in the study area.
| Beliefs regarding snakes | First aid | Treatment practices | Socio-cultural beliefs |
|---|---|---|---|
| Checkered keel back lives only in water. | Tying a bandage/cloth above the bite site tightly prevents venom from spreading. | Treatment after a bite is not required. Drinking the water in which the snake lives is the medicine itself. | After a snakebite, if the person feels the taste of red chilli or spices, it is non-venomous, and if there is no taste, it is venomous. |
| The severity of common Krait venom is directly proportional to the number of white lines on its body. | Cutting the bite site makes the venomous blood go out. | The victim should not sleep for the whole night after the bite as sleeping increases the spread of venom in the body. | If the stick or stones tied to the head of the victim after a snake bite fall off while walking or even during tying, then the victim will not survive. |
| If the sea snake is killed after the bite, symptoms will appear. |
Tying five small stones on the elbow/wrist reduces venom spread. The rocks should be removed only after the venom goes down. |
The first treatment is always at the priest; if the priest is unavailable, then the hospital. | The doctor cannot treat the patient if the dead snake is not taken to the hospital or if a photo of the biting snake is not shown. |
|
The Indian Sand Boa has two mouths. It walks in one direction for six months and then in the opposite direction for the next six months. The Sand Boa has medicinal properties and can cure cancer. So it is sold at the price of >2 million rupees. |
Tying a stick on the head of the victim does not allow the venom to go to the head. | Killing the snake before the Pujari starts treatment will not result in a complete cure. The snake should be only partially killed. After the treatment is started, then the snake should be killed entirely. | Snakes can smell a wooden stick enchanted with mantras by a Pujari from a long distance and stay away. |
| It is wrong to point a finger at the Brahminy Blind Snake. The more we show fingers, the more their number increases. | Herbal treatment applied while chanting mantras by the Naag Mantri is the best first aid before going to the hospital. | Treatment should not be taken from the priest if his wife is menstruating. | If a torch beam is put on the snake, it turns back and goes away. |
| The Indian Rock Python can eat humans. | The snake leaves its teeth in our skin. The embedded teeth can be removed by moving a long hair over the bite site. | To prevent the necrosis of the foot after Russell’s viper bite, the foot has to be kept in a deep hole dug in the soil, and the hole should be filled with burning charcoal. | Worshipping the Naagdevta (Snake God) is helpfulif snakes are frequently seen in dreams. |
| If the rat snake hits with its tail, then there is a lot of weight loss. | If a snake bites a woman, her bangles must be immediately broken. | The priest can tell the name of the biting snake by smelling the wound. | A woman is not allowed to go near the snakebite victim. |
| The vine snake flies from one tree top to the other and can change its colour as per the colour of the tree. If it bites us, then even the victim starts changing colours. | The venom’s spread is increased when it is green. After a bite, the victim must be removed from any green colour. | The venom comes out through vomiting after the medicine is given by the priest—the more vomiting, the more venom in the body. | If a menstruating woman goes near a victim or even if her shadow falls on the victim, then the victim either dies or forgets everyone around. |
| Only the people who treat snakebites can correctly identify venomous and non-venomous snakes. Others only guess. | Rice leaf or rice/wheat stem tied over the wound reduces the venom spread in the body. | More people die now after going to hospitals compared to the older times when only herbal medicine was available. | If a rat snake bites on a Saturday, it is considered lucky. |
| Because the Common Krait is black, it is always searching for light, and it comes to our homes at night to look at the light. | Applying homemade cow ghee will reduce the venom effects on the body. | After a snakebite, Usuna rice (double boiled rice) and non-veg food should be avoided completely and only Arua rice (plain rice) has to be consumed for 21 days. | If the snake is hurt by throwing a rock or stone, it remembers that incident and keeps a watch. Then it comes and bites the person in the night. |
| Krait bite has to be treated before sunrise, or else the victim dies. | Tourniquet/bandage/cloth tied above the bite site should be so tight that even air should not pass in between. | Slappinga Gunia to the person who brings the snakebite information will reduce the venom in the victim’s body. | Doing a Pranam (bowing down respectfully) will calm down the snake, and it will go away after biting. |
| The Common dotted garden skink is considered a snake, and if it bites, the victim dies before taking five steps (the name pachpavli literally translates to five steps). | - | Pour water on the victim’s head while chanting Lord Shiva’s name. If the victim gets cold, venom has come out of the body. | Bite by a water snake gives an odour to the body. After that, no other snake will ever bite you. |
| The banded krait’s venom rises in the body as the sun rises in the sky, and the victim is dead by sunset. | - | Chermuli, Gada, and Umbhiri trees help reduce the body’s venom. | Snakes bite people who have done evil deeds or have bad luck. |
| If a male Cobra is killed, the female Cobra captures photographs of the killer in her eyes and then takes revenge. | - | Arakha (Calotropis gigantea) milk is applied at the place of the bite to reduce venom. | Putting a towel or cloth on the head of the snake prevents snakebite. |
| The non-venomous water snake (called Malundi) pushes its tail into a child’s mouth and feeds on the milk given to the child. The mouth of the child becomes infected when this happens. Malundi can detect a new-born by smell. | - | Magnets can be used to extract venom from the victim’s body. | Snakes only attack people who walk straight. If your walk is crooked, snakes don’t attack. |
| If a Brahminy Blind Snake is killed, then five/six snakes come to kill you. | - | - | - |
Gender aspects influencing practices
The findings of this study did not reveal any specific gender differences in the knowledge of the respondents. However, many traditional beliefs influenced the first aid and health-seeking behaviour across States.
If a snake bit a man, women were forbidden to touch him, especially if she wore green clothing. If the male victim was shifted to a room, women were not allowed to enter that room. If a menstruating woman goes near a victim or even if her shadow falls on the victim, it results in either immediate death or complete memory loss. These restrictions also prohibited the wife from taking her husband to a healthcare facility.
“See, we are not allowed to enter the room or even touch. We call other people; they do whatever is required. It is a bit better now in some places, but previously, we were not allowed to go in the ambulance or vehicle as well.”
Moderator, “This is only in case of snakebite or all the diseases?”
“No, only snake, scorpion, and other poisonous animal bites. If a woman goes close to a man, then the poison spreads faster, so we avoid it completely. We don’t want the blame!”
A solution was reported in Shahapur–
“The only way to meet the male is to break all the bangles first and then go inside. Do not do anything before that.”
The traditional healers even refused to see a patient when the healer’s wife was menstruating and denied treatment to menstruating female victims. Women respondents had to shift to a dilapidated hut outside the village during menstruation. Women have had snakebites while they were staying in these huts.
“A few years back, a snake bit a woman in the menstrual hut. She was taken to a priest. He did not see her. They took her to another priest in the next village. There, his wife was having periods. He refused. The poor lady had to be taken to a government hospital 200 km away. The family lost all their money on the transport and treatment.”
Discussion
This study highlights multiple challenges that rural communities in Maharashtra and Odisha districts face in overcoming SBE. Knowledge gaps, sociocultural beliefs, and inaccessible and inadequate health systems complicate treatment-seeking behaviour and push the communities to avail easily accessible and affordable traditional care. Lack of respectful care at health facilities, repeated referrals and financial constraints reduce healthcare service uptake. Gender plays a crucial role in healthcare seeking from traditional healers, and cultural beliefs restrict women’s participation in caregiving. Non-scientific first aid techniques and non-utilization of prevention methods pose major challenges. Together, they create a series of barriers at the community and health system level that hamper the implementation of SBE reduction strategies.
Lack of awareness regarding snakes, their venomous nature, and symptoms of envenomation is a repeatedly reported finding in high-burden regions12,19. SBE predominantly affects rural communities, particularly those engaged in agriculture, as their occupation makes them vulnerable to increased human-snake conflict20. This study was primarily focused on this population to understand their perspectives and beliefs that shape the burden of SBE. The findings reveal that misconceptions still exist among communities regarding venomous and non-venomous snake species. There is a lack of clarity on the differences in signs and symptoms of snakebite as well, prompting the communities to hold off the treatment until clear symptoms appear and last for at least some hours, leading to loss of precious time. This, coupled with barriers to reaching the health facility, potentially converts a snakebite case to a fatality21. There is an urgent need to educate rural communities on the clear signs and symptoms of venomous bites and the importance of seeking timely care. Community engagement is the key to the success of such programmes, and involving leaders, teachers, prominent individuals, and public and private organizations that the communities know and trust can accentuate their impact9,12.
However, improving the utilization of the public healthcare system in controlling SBE should not be discounted. Anti-venom (ASV) is the only remedy for venomous snakebites. Challenges in administering ASV in India, either due to non-availability or lack of confidence in the Medical Officer, render the facility useless, and referrals to higher centres become a necessity22. In rural areas, doctors are generally unavailable at night time23. The ability of doctors to calculate ASV dosage and manage anaphylaxis creates further challenges24. Current medical education in India does not adequately train doctors for SBE management, particularly in using ASV24. Though the community prefers the public healthcare system, the lack of infrastructure, roads, connectivity and timely ambulance service pushes them towards traditional methods. Including medical officer training on SBE management in the induction programme, along with the provision of simplified treatment protocols and availability of ASV, can improve the treatment at PHCs and reduce referrals24,25. India has significantly expanded its ambulance network and that has played a vital role in reducing SBE mortality26. However, improving the situation of roads and mobile connectivity requires multi-sectoral involvement and is beyond the scope of the health system alone20, resulting in a higher number of in-transit deaths8.
Our study reveals that besides the dysfunctional health system, faith, availability, and low cost were the drivers of seeking traditional methods. Heavy reliance on traditional healers has been documented previously in India27, Pakistan28 and Bangladesh29. The use of Rouvolfia serpentina for SBE management has also been reported30. Other plants used are not disclosed, and their utility and biological plausibility remain unexplored. Based on findings of this study, the beliefs that require further studies to confirm their utility include sitting around the victim to calm them down, possibly to reduce the heart rate and slow down venom circulation, breaking bangles in a woman after snakebite, possibly for impending swelling or use of spices to check for ageusia/dysgeusia after a cobra bite.
Compared to studies from Kenya31, Brazil32 and Nepal33, most respondents in this study did not mention fear of snakes and snakebite as a reason for wanton killing of snakes. Cultural beliefs and misconceptions, similar to a study from Sri Lanka34, primarily influenced the fate of snakes. Pressure Immobilization Bandaging (PIB) is an effective first aid strategy after snakebite35. The use of tourniquets is not an uncommon finding and has been reported previously along with its harmful effects7,8. Farmers are used to working barefoot, and difficulties in working with gum boots, which become wet and heavy, increase their burden34. This, along with the cost, reduces their utilization in SBE prevention. Stigma against menstruation is an important gender-based issue that has put women at a disadvantage in seeking treatment. The poor conditions of menstrual huts have been documented21; however, constructive action against this practice has been challenging to achieve.
Our study reinforces SBE as a multifaceted public health issue. To facilitate understanding, especially for community members, we collated our findings to present two barrier frameworks that impact the prevention and outcomes of SBE (Fig. 3). The frameworks not only present the challenges but also indicate potential areas of intervention.
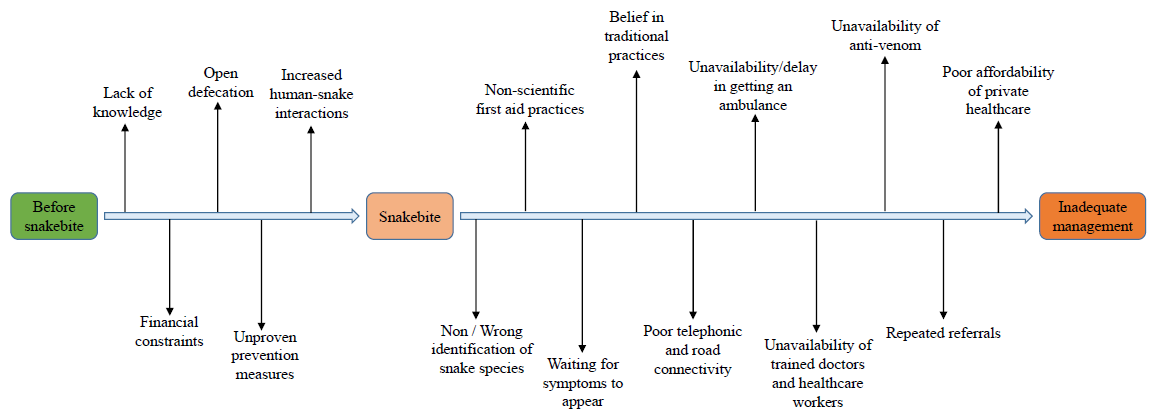
- The barriers to prevention and barriers to effective management frameworks highlighting potential avenues for intervention.
The barrier to prevention framework tries to collate all the challenges in preventing snakebites. It was concerning that respondents were unaware of cost-effective prevention measures, such as sleeping on beds and using mosquito nets36. About 8 per cent of snakebites occur during open defecation37. Although the Government of India incentivizes toilet construction, lack of water and reluctance to use toilets undermine these efforts, making a strong case for community education. Furthermore, the use of substances like Thimet has been reported in Maharashtra7. Various compounds like naphthalene, sulfur, gourd vines, cedar oil, lime, and coal tar have been shown to have no snake-repellent effect38. Reliance on unproven substances increases their vulnerability to snakebites and the ill effects of pesticide exposure. Most snakebite victims are engaged in agrarian activities, making habitat modification for reducing human-snake interactions an uphill task. Escalating land use, deforestation, and climate change have resulted in an exponential increase in human-wildlife conflict39, especially in the tribal-population-dominated regions40. Engaging biodiversity professionals, including herpetologists and the local forest department authorities, in controlling such interactions is necessary for improving prevention efforts.
The barrier framework for effective SBE management describes the challenges at the community level, in transit and in the healthcare system. This bite-to-outcome journey is similar to the three-delay model on pregnancy-related mortality41. Steps in this framework provide a potential opportunity to intervene to break the barrier chain. Improving SBE outcomes requires collaboration among education, public works, telecommunication, social justice, medical education, and public health agencies42. A study from Nepal reported that majority of the traditional healers were willing to gain SBE knowledge and collaborate with the health system to improve SBE outcomes30. A study from Cameroon demonstrated that utilizing the potential of conventional healers in propagating health education is well accepted and reciprocated43. The Community of Practice (COP) model includes healers, volunteers and former patients along with subject experts, NGOs and health authorities44. Such a comprehensive and inclusive health system and community engagement model has the potential to bring in a multifaceted implementation strategy for SBE control45.
The present study focussed only on the community perspective, resulting in a potential bias while reporting against the health system. The study was part of Phase I of the ICMR National Snakebite Project. This limitation would be addressed during further phases16. The barrier framework presented is a mere collation of the information provided by the respondents in the FGDs and does not have strong data backing. Future studies to evaluate these frameworks are required for their validation.
Implications of this study
The National Action Plan for Prevention and Control of Snakebite Envenoming (NAPSE) in India will be implemented across all high-burden regions. The findings of the present study, though contextual, provide crucial regional inputs from Maharashtra and Odisha not only for the national programme but also for future research (Box). In light of the emerging evidence from this and similar studies across diverse populations in India, national implementation strategies for the control of SBE could be revised for better acceptability and effectiveness.
Acknowledgment
Authors acknowledge the members of the Technical Advisory Committee: Drs J. Menon, Y. Kalkonde, D. Majumdar, M.Vyawahare, K. Bhide, and J. K. Chakma for their critical inputs. District and Taluka Health Officers at the study sites are acknowledged for their aid in project implementation. Authors acknowledge Public Health Departments in Maharashtra and Odisha States for providing administrative permissions for the study.
Financial support & sponsorship
This study received financial support from the Indian Council of Medical Research, New Delhi (no: 58/6/NTF-Snakebite/2019-NCD-II). Author RKG received financial support from the DBT-Wellcome India Alliance clinical and public health intermediate fellowship (Grant no. IA/CPHI/18/1/503933).
Conflicts of Interest
None.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of AI-Assisted Technology for assisting in the writing of the manuscript and no images were manipulated using AI.
References
- Addressing the burden of snakebite envenoming. Available from: https://apps.who.int/iris/bitstream/handle/10665/279476/A71_R5-en.pdf, accessed on July 11, 2022.
- Global mortality of snakebite envenoming between 1990 and 2019. Nat Commun. 2022;13:6160.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Strengthening global snakebite data for WHO’s goal for 2030. Lancet. 2024;403:907-8.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnosis of envenomation by Russell’s and Echiscarinatus viper: A clinical study at rural Maharashtra state of India. J Family Med Prim Care. 2019;8:1386-90.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Long-term health effects perceived by snakebite patients in rural Sri Lanka: A cohort study. PLoS Negl Trop Dis. 2022;16:e0010723.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Perceptions, awareness on snakebite envenoming among the tribal community and health care providers of Dahanu block, Palghar District in Maharashtra, India. PLoS One. 2021;16:e0255657.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- A prospective study of snakebite in a tertiary care hospital in south-western Nepal. Trans R Soc Trop Med Hyg. 2023;117:435-43.
- [CrossRef] [PubMed] [Google Scholar]
- Approaches for implementing society-led community interventions to mitigate snakebite envenoming burden: The SHE-India experience. PLoS Negl Trop Dis. 2021;15:e0009078.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Burden and risk factors for snakebite in India: Protocol for a systematic review. F1000Res. 2020;9:25.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Disentangling snakebite dynamics in Colombia: How does rainfall and temperature drive snakebite temporal patterns? PLoS Negl Trop Dis. 2022;16:e0010270.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Multifaceted community health education programs as powerful tools to mitigate snakebite-induced deaths, disabilities, and socioeconomic burden. Toxicon X. 2023;17:100147.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Trends in snakebite deaths in India from 2000 to 2019 in a nationally representative mortality study. Elife. 2020;9:e54076.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Snakebite mortality in the world. Bull World Health Organ. 1954;10:35-76.
- [PubMed] [PubMed Central] [Google Scholar]
- Clustering the envenoming of snakebite in India: The district level analysis using health management information system data. Clin Epidem Global Health. 2020;8:733-8.
- [CrossRef] [Google Scholar]
- National snakebite project on capacity building of health system on prevention and management of snakebite envenoming including its complications in selected districts of Maharashtra and Odisha in India: A study protocol. PLoS One. 2023;18:e0281809.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Worldviews, research methods, and their relationship to validity in empirical software engineering research. 2013 Joint Conference of the 23rd International Workshop on Software Measurement and the 8th International Conference on Software Process and Product Measurement, Ankara, Turkey, 2013, p. 81-89.
- Using grounded theory method to capture and analyze health care experiences. Health Serv Res. 2015;50:1195-210.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Assessing knowledge and awareness regarding snakebite and management of snakebite envenoming in healthcare workers and the general population: A systematic review and meta-analysis. PLoS Negl Trop Dis. 2023;17:e0011048.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Barriers and enablers of community engagement practices for the prevention of snakebite envenoming in South Asia: A qualitative exploratory study. Toxicon X. 2023;17:100144.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Analysis of news media-reported snakebite envenoming in nepal during 2010-2022. Monteiro WM, editor. . PLoS Negl Trop Dis. 2023;17:e0011572.
- [Google Scholar]
- Challenges in diagnosing and treating snakebites in a rural population of Tamil Nadu, India: The views of clinicians. Toxicon. 2017;130:44-6.
- [CrossRef] [PubMed] [Google Scholar]
- Profile of snakebite envenoming in rural Maharashtra, India. J Assoc Physicians India. 2008;56:88-95.
- [PubMed] [Google Scholar]
- A study of the current knowledge base in treating snake bite amongst doctors in the high-risk countries of India and Pakistan: Does snake bite treatment training reflect local requirements? Trans R Soc Trop Med Hyg. 2008;102:1108-14.
- [CrossRef] [PubMed] [Google Scholar]
- Doctors for tribal areas: Issues and solutions. Indian J Community Med. 2016;41:172.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Transporting snakebite victims to appropriate health facility to save lives through emergency ambulance service in India. Int J of Infec Dis. 2016;45:225.
- [CrossRef] [Google Scholar]
- Snakebite: Admissions at a tertiary health care centre in Maharashtra, India. S Afr Med J. 2010;100:456.
- [CrossRef] [PubMed] [Google Scholar]
- Snake Bite: Treatment seeking behaviour among Sindh rural population. JAMC 2000:12.
- [Google Scholar]
- Annual incidence of snake bite in rural Bangladesh. Lalloo DG, editor. PLoS Negl Trop Dis. 2010;4:e860.
- [CrossRef] [Google Scholar]
- Attitudes, knowledge and practices of traditional snakebite healers in Nepal: implications for prevention and control of snakebite. Trans R Soc Trop Med Hyg. 2023;117:219-28.
- [CrossRef] [PubMed] [Google Scholar]
- Scientific and traditional conceptions of snakes in kenya: herpetologists as teacher mentors. Herpetological Review. 2009;40:158-62.
- [Google Scholar]
- Students’ attitudes toward and knowledge about snakes in the semiarid region of Northeastern Brazil. J Ethnobiology Ethnomedicine. 2014;10:30.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Public perceptions of snakes and snakebite management: Implications for conservation and human health in southern Nepal. J Ethnobiology Ethnomedicine. 2016;12:22.
- [CrossRef] [Google Scholar]
- Awareness and perceptions on prevention, first aid and treatment of snakebites among Sri Lankan farmers: A knowledge practice mismatch? J Occup Med Toxicol. 2014;9:20.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Knowledge of first aid methods and attitude about snake bite among medical students: A cross sectional observational study. J Occup Med Toxicol. 2018;13:26.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Prevention of krait bites by sleeping above ground: Preliminary results from an observational pilot study. J Occup Med Toxicol. 2017;12:10.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Guidelines for the Management of Snakebites, 2nd edition. Available from: https://www.who.int/publications/i/item/9789290225300, accessed on July 24, 2023.
- Assessing the efficacy of five commonly used snake and gecko repelling agents when applied outdoors. Available from: https://repository.up.ac.za/handle/2263/81025, accessed on July 24, 2023.
- Applying species distribution models in public health research by predicting snakebite risk using venomous snakes’ habitat suitability as an indicating factor. Sci Rep. 2020;10:18073.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Prioritizing the health and well-being of the indigenous communities in India. Asia Pac J Public Health 2024:10105395231226298.
- [CrossRef] [Google Scholar]
- Too far to walk: Maternal mortality in context. Soc Sci Med. 1994;38:1091-110.
- [CrossRef] [PubMed] [Google Scholar]
- National programme for prevention & control of snakebite in India: Key challenges & recommendations. Indian J Med Res. 2023;157:271-5.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Developing a buruli ulcer community of practice in Bankim, Cameroon: A model for buruli ulcer outreach in Africa. PLoS Negl Trop Dis. 2018;12:e0006238.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Assessing communities of practice in health policy: A conceptual framework as a first step towards empirical research. Health Res Policy Sys. 2013;11:39.
- [CrossRef] [Google Scholar]
- Empowering health care systems and communities for snakebite envenoming control in India. Asia Pac J Public Health. 2023;35:535-7.
- [CrossRef] [PubMed] [Google Scholar]






