Translate this page into:
Prevalence of prehypertension in young military adults & its association with overweight & dyslipidaemia
Reprint requests: Dr Sougat Ray, Room 141, A Wing, Sena Bhawan, New Delhi 110 011, India e-mail: sougatray@hotmail.com
-
Received: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Estimation of prevalence of prehypertension in a population and its association with risk factors of cardiovascular disease is important to design preventive programmes. This cross-sectional study was carried out in a healthy military population to assess the prevalence of prehypertension and its association with risk factors such as overweight, abdominal adiposity and dyslipidaemia.
Methods:
The study included 767 participants (130 officers and 637 from other ranks). The blood pressure, serum triglycerides and serum cholesterol (total, HDL and LDL) were assessed along with anthropometric measurements such as height, weight, waist-hip ratio in apparently healthy military personnel. Information on smoking, alcohol intake, dietary habits and physical activity was collected using pretested questionnaire. Prehypertension was defined as systolic blood pressure (SBP) 120-139 mm Hg and diastolic blood pressure (DBP) 80-89 mm Hg.
Results:
The overall prevalence of prehypertension was high (about 80%). The prevalence of other risk factors such as overweight (BMI>23 kg/m2), serum total cholesterol > 200 mg/dl, serum LDL cholesterol > 130 mg/dl, serum HDL cholesterol <40 mg/dl, serum triglyceride > 150 mg/dl in the total group was 30, 22, 22, 67, and 14 per cent, respectively. Most of the personnel undertook moderate or heavy exercise. A significantly higher proportion of individuals with prehypertension had clinical and behavioural risk factors such as overweight, dyslipidaemia and adverse dietary practices like saturated fat and added salt intake. On multivariate logistic regression analysis, prehypertension had significant positive association with BMI>23 kg/m2 (OR 1.75), age (OR 1.89), serum triglyceride >150 mg/dl (OR 2.25)and serum HDL cholesterol <40 mg/dl (OR 1.51).
Interpretation & conclusions:
The high prevalence of prehypertension and its association with overweight and dyslipidaemia in this young, physically active military population indicates an urgent need for targeted interventions to reduce the cardiovascular risk.
Keywords
Cardiovascular risk
dyslipidaemia
overweight
prehypertension
The term ‘prehypertension’ was coined in 1939 in the context of early studies that linked high blood pressure recorded for life insurance purposes to subsequent morbidity and mortality1. These studies demonstrated that individuals with blood pressure >120/80 mmHg, but <140/90 mmHg, had an increased risk of hypertension, cardiovascular disease and early death from cardiovascular causes. This observation has been confirmed by a number of studies1–3. For example, meta-analysis of approximately 1 million individuals from 61 long-term epidemiological studies demonstrated that for each 20 mmHg increase in systolic blood pressure or 10 mmHg increase in diastolic blood pressure over 115/75 mmHg, there was a two-fold increase in mortality associated with coronary artery disease and stroke4.
This classification of blood pressure was later used by the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure5. The risk of cardiovascular disease in the individuals with prehypertension was observed to increase with concomitant burden of other risk factors such as obesity, diabetes mellitus and dyslipidaemia. The Report suggested that estimation and reduction of these risk factors in the population are desirable to reduce the overall risk of cardiovascular disease.
The prevalence of hypertension and cardiovascular disease is rapidly increasing in India. A survey conducted in nine States of India by the National Nutrition Monitoring Bureau reported the pooled estimate of prehypertension in rural men to be about 45 per cent6. A few studies from different regions of India have also indicated the prevalence of prehypertension in the range of 40-60 per cent78. Similar information, however, is not available in the Indian military personnel. Although military personnel are in general healthy, physically active and health conscious, psychosocial factors such as job related stress may increase the risk of prehypertension and cardiovascular disease. Ongoing nutrition transition with progressive shift to a westernized diet may further accentuate the risk.
Estimation of prevalence of prehypertension and its risk factors is important for designing strategies for the control and prevention of cardiovascular diseases9. This cross-sectional study (health interview and health examination survey (HIS/HES) was, therefore, conducted in a military population with the aim of estimating the prevalence of prehypertension and its association with risk factors such as overweight and dyslipidaemia.
Material & Methods
Assuming the prevalence of prehypertension to be 50 per cent, with 95 per cent level of confidence and 5 per cent absolute error and assuming the design effect of 2 for cluster sampling, the sample size was calculated to be 768. It was, therefore, decided to enroll 800 men in the study.
This study was conducted during the period 2005-2007 in an urban population in southern India, with an estimated military adult population of 15,000 (1600 officers and 13400 other ranks). Of a total of 70 units having a population of more than 300 each, 16 units were selected by random sampling. From the list of personnel in each unit, 50 participants were chosen in the two rank categories of officers (higher socio-economic stratum) and other ranks (lower socio-economic stratum) according to their proportion (officers: other ranks 1:5) in the total population. Thus, 9 officers and 41 personnel from other ranks were chosen from each unit with a total of 800 persons. Personnel known to be having ischaemic heart disease, hypertension, obesity and diabetes were excluded from the study. Of the total 800 persons, 33 were excluded for non availability or refusal to get examined and data on 767 individuals were finally available.The participants were interviewed and information regarding age, marital status, personal habits like smoking, alcohol intake, exercise profile and dietary habits like added salt intake, pickle intake, ghee/butter intake was collected using a pretested questionnaire.
A written informed consent was obtained from all the participants who responded to the questionnaire survey. The study protocol was approved by the institutional ethics committee before the start of the study.
The major biological risk factors identified in the World Health Report 200210 and included in STEPS Chronic Disease Risk Factor Surveillance11; overweight and obesity, raised blood pressure, raised blood glucose, abnormal blood lipids and its subset ‘raised total cholesterol’ were modified to be adopted in this study. Overweight was defined as BMI>23 kg/m2 and dyslipidaemia was measured by total cholesterol >200 mg%, HDL<40 mg%, LDL>130 mg% and triglyceride >150 mg%.
Standing height was measured to the nearest 0.1 cm using a wall mounted stadiometer (Chasmors Ltd., UK) and body weight was measured to the nearest 0.1 kg in an automated balance (SECA, Germany). Waist circumference was measured at the midpoint between lower most point of the costal margin and highest point of iliac crest with the subject standing, at the end of normal expiration. Hip measurement was done at the maximum circumference of the hip. BMI was determined as Quetlet's index (kg/m2). Blood pressure was measured early in the morning on the left arm with the use of an automated blood pressure monitor (Omron Hem - 608, Japan) in a sitting position twice after 5 min of rest in a quiet room. The mean of the two measurements was taken. ‘Prehypertension’ was defined as systolic blood pressure (SBP) 120-139 mm Hg and diastolic blood pressure (DBP) 80-89 mm Hg5. Blood was collected after an overnight fasting of 10-12 h for lipid profile. Plasma total cholesterol, triglycerides and HDL were measured using enzymatic kits (Autopak, India). LDL was calculated using the Friedewald formula12. The intra- and inter-assay CV established was <2 and <3 per cent, respectively for cholesterol and 2.5 and 3.5 per cent for triglycerides and HDL cholesterol, respectively13.
Statistical analyses were carried out using STATAversion 10 (College Station, Texas) software. Mean and SD were calculated for continuous variables and proportions were calculated for the categorical variables. Differences in the mean values of the subject characteristics in the two groups were analysed using student's t test and the differences in the distribution of risk factors in the two groups were assessed using chi square tests. Relationship of prehypertension with the risk factors was assessed using univariate as well as multivariate logistic regression analyses. Univariate logistic regression analyses were later adjusted for age. Multivariate logistic regression model was adjusted for potential confounders such as age, rank, BMI, serum total, HDL and LDL cholesterol levels and serum triglyceride level. Presence of prehypertension was considered as a dependent variable whereas risk factors such as BMI >23 kg/m2, total cholesterol >200 mg/dl, LDL>130 mg/dl, HDL<40 mg/dl, triglyceride>150 mg/dl, rank and age category were independent variables. Age was classified in 3 categories < 30, 31-40 and ≥ 41 yr.
Results
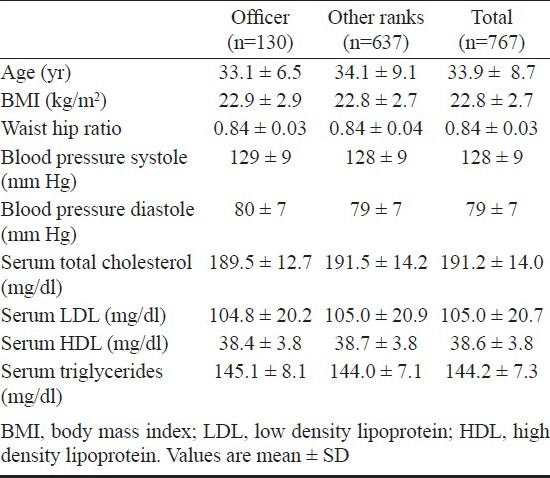
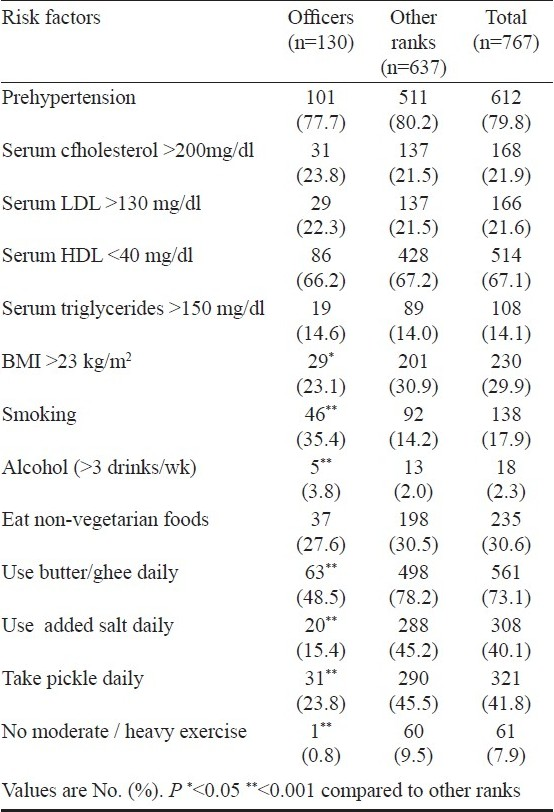
The study population comprised 17 per cent officers and 83 per cent other ranks. The average age of total group was 33.9 years (range 18-50 yr) with other ranks having slightly higher age than that of officers (mean ± SD 34.1± 9.1 vs 32.5±6.5 yr P<0.05). Of the 767 personnel, 431 (55%) were from the rural background and 670 (85%) were married. There were no significant differences between the mean values of blood pressure (systolic and diastolic), serum total, HDL and LDL cholesterol and serum triglyceride levels between the two rank groups though the mean BMI was slightly higher in other ranks than in officers (Table I). Overall prevalence of prehypertension was about 80 per cent. Almost 67 per cent of the total group had HDL cholesterol levels < 40 mg/dl though the prevalence of raised total and LDL cholesterol and serum triglycerides were within a range of 14-22 per cent. Prevalence of dyslipidaemia was not significantly different in the two rank categories. Less than a third of the total group had BMI >23 kg/m2 with the other ranks having a significantly higher prevalence of BMI> 23 kg/m2 than the officers (Table II). Overall, about 18 per cent personnel were smokers with a higher proportion of officers being smokers than the other ranks. Of the smokers,12 per cent had more than 20 cigarettes per day. Proportion of personnel that reported consuming alcohol >3 times a week was only 2.3 per cent with a higher proportion observed in officers than other ranks (Table II). Adverse dietary habits were observed in a large number of participants with about two thirds of the personnel taking butter or ghee daily and about 40 per cent reported using added salt or pickle regularly. Most of the military personnel undertook moderate or heavy exercise except one officer and 60 (9.5%) persons with other ranks who undertook only light exercise.
When the risk factors were analyzed in relation to the presence of prehypertension, the mean values of serum total, HDL and LDL cholesterol, triglycerides, BMI and W/H ratio were observed to be higher in the prehypertensives than in the normotensives (data not shown). Similarly, a higher proportion of individuals with prehypertension had the clinical and behavioural risk factors such as BMI>23 kg/m2, total cholesterol >200 mg/dl, serum LDL cholesterol >130 mg/dl, serum HDL cholesterol <40 mg/dl, serum triglyceride >150 mg/dl, than those with normotension (Fig.).
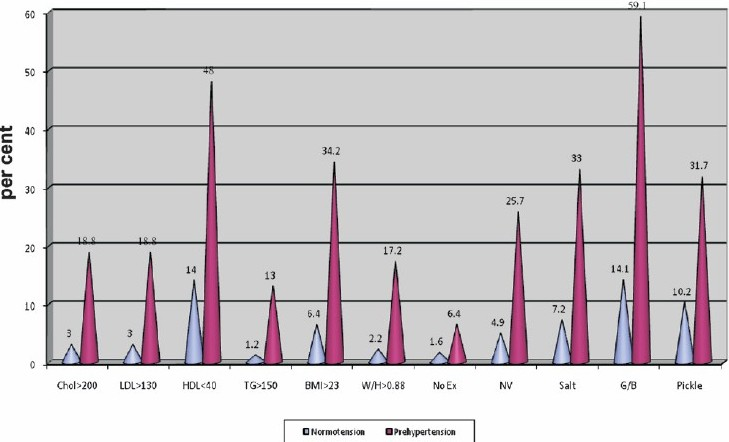
- Proportion of individuals with normotension and prehypertension having clinical and behavioural risk factors. Chol>200, serum cholesterol >200 mg/dl, LDL>130 - serum LDL cholesterol >200 mg/dl, HDL < 40 - serum HDL cholesterol level <40 mg/dl, TG >150- serum triglyceride >150 mg/dl, BMI >23-body mass index> 23kg kg/m2, W/H >0.88, waist hip ratio >0.88, NoEx, nomoderate /heavy exercise; NV, non-vegetarian food intake, G/B, ghee/butter intake, pickle, pickle intake. The proportions of individuals with high risk clinical and behavioral risk factors in the normotensive and prehypertensive group were significantly different (all P<0.001) except the proportion of individuals not doing moderate/heavy exercise.
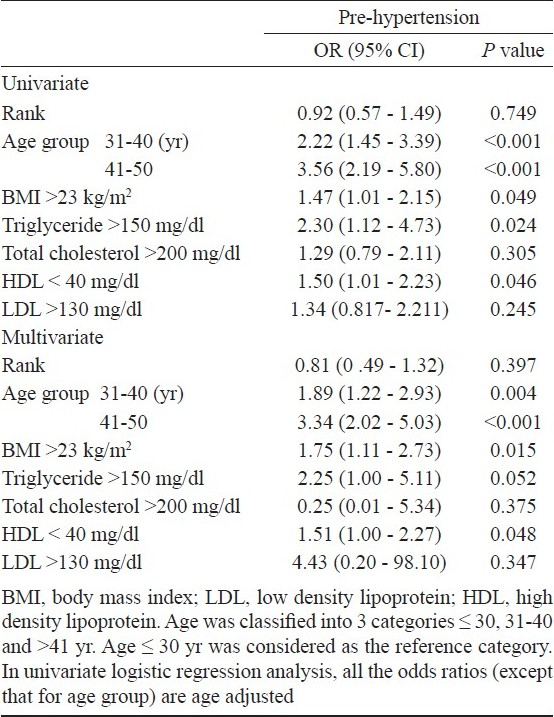
Using univariate logistic regression analysis, after adjustment for age, prehypertension was also found to be associated with BMI >23 kg/m2 (OR 1.47, 95% CI:1.01- 2.15, P=0.049), serum HDL cholesterol <40 mg/dl (OR1.50, 95% CI:1.01-2.23, P=0.046), serum triglyceride >150 mg/dl (OR 2.30, 95% CI:1.12- 4.73, P=0.024) and age (OR for age group 31-40 -2.22, 95% CI: 1.45-3.39, P<0.001 and OR for age group 41-50 -3.56, 95% CI:2.19-5.80, P<0.001). These relationships were confirmed with the multivariate logistic regression analysis (Table III).
Discussion
The study indicates a high prevalence of prehypertension in an apparently healthy military population which is a cause for concern as these individuals are at high risk of developing hypertension and cardiovascular disease in later life. The prevalence of prehypertension observed in this study was much higher than the estimates reported by the studies in other parts of the country4514. For example, a study in an industrial population in northern India reported a prevalence of prehypertension to be 44 per cent14 whereas a study among urban residents in Chennai indicated a 47 prevalence of prehypertension in adults >18 yr7. A study in rural population in Assam also indicated the prevalence of prehypertension to be 54 per cent15. It is possible that the prevalence of prehypertension in the present study is inflated because the hypertensive individuals were excluded from the study. The relative proportion of prehypertensive individuals in nonhypertensive population, therefore, appears to be higher. Nevertheless, the high burden of prehypertension indicates an impending epidemic of cardiovascular disease in this population. It is important to note that the present study included relatively younger individuals of ≤ 50 yr. The mean age of participants in the other Indian studies was higher than this study because those studies included all the adults >18 yr. Considering the fact that prehypertension had strong positive association with age, it may be speculated that the prevalence of prehypertension would have been even higher if the study had included adults >50 yr. The high prevalence of prehypertension in these young physically active adults with a relatively low prevalence of overweight and obesity is a cause of concern because of the higher risk of cardiovascular disease in this productive age group.
Most of the individuals with prehypertension had at least one additional risk factor such as overweight or dyslipidaemia which is known to enhance the cardiovascular risk. Earlier studies have also indicated that prehypertension generally coexists with other risk factors. For example, NHANES II data from the United States showed that 90 per cent of individuals with prehypertension had at least one or other cardiovascular risk factor16. Women's Health Initiative study in 60,785 women showed that important cardiovascular risk factors including prevalence of diabetes mellitus and hypercholesterolaemia increased across rising categories of blood pressure17. Studies from India have also indicated that increasing age, BMI, waist hip ratio and impaired glucose tolerance/diabetes were independent risk factors for hypertension and prehypertension4814. Our study corroborates these observations as a higher proportion of participants with prehypertension had biochemical and behavioural risk factors when compared to the normotensive individuals though only age, BMI, serum triglyceride and HDL cholesterol levels were significant predictors of prehypertension in multivariate logistic regression analysis.
A large proportion of prehypertensive individuals were found to be indulging in adverse dietary practices such as added salt and pickle intake, and using ghee/butter in their meals. The low prevalence of smoking and alcohol intake > 3 times/week could be because of under-reporting of these behaviours. It is well recognized that higher salt intake is associated with higher blood pressure and reduction in salt intake lowers blood pressure. For example, the Intersalt study which investigated the association between 24 h sodium excretion and blood pressure revealed that a higher sodium intake by 100 mmol/day (2.3 mg/day) was reflected in higher SBP/DBP by approximately 3-6/0-3 mm Hg18. Several studies have demonstrated the efficacy of dietary approaches, alone or in combination with other lifestyle modifications, to reduce BP in both prehypertensive and hypertensive persons. The Dietary Approaches to Stop Hypertension (DASH) eating plan, which uses a diet rich in fruits, vegetables, legumes, nuts, and low-fat dietary products and low saturated fats, induced a significant lowering of BP, which was reduced even further when dietary sodium was restricted19. The PREMIER trial20 studied the combined effects of diet, physical activity, and weight reduction in 3 groups of prehypertensive and hypertensive subjects over an 18-month period. The group that received several group and individual counselling sessions with the DASH diet, showed the highest average BP fall of 9.5/6.2 mm Hg15. It is thus essential to design interventions to reduce salt and saturated fat intake in this vulnerable population and examine their effect on their blood pressure.
There were certain limitations of the study. First, the cross-sectional design of the study does not allow any inference to be drawn with respect to the causal relationship among variables. Secondly, the study sample was a select group of young military adults and the findings may not be generalized to the whole population. Thirdly, though it is speculated that job related stress may be one of the causes of high prevalence of prehypertension, the factors causing stress were not assessed in this study. In addition, the sample size of the present study was probably small for a highly prevalent problem of prehypertension. The conclusions of the study, therefore, need to be interpreted with caution.
In conclusion, our the study provides important information on the high burden of cardiovascular risk factors such as prehypertension, overweight and dyslipidaemia, in an apparently healthy and physically active young military adults. Lifestyle modifications such as reducing intake of saturated fats and salt in diet and reducing smoking can achieve a downward shift in the overall blood pressure, thus reducing the risk of hypertension and cardiovascular disease.
References
- Impact of high normal blood pressure on the risk of cardiovascular disease. N Engl J Med. 2001;345:1291-7.
- [Google Scholar]
- Prehypertension: epidemiology, consequences and treatment. Nat Rev Nephrol. 2010;6:21-30.
- [Google Scholar]
- Prehypertension and the risk for cardiovascular disease in the Japanese general population: the Jichi Medical School Cohort Study. J Hypertens. 2010;28:1630-7.
- [Google Scholar]
- Range of normal blood pressure: a statistical and clinical study of 11,383 persons. Arch Intern Med. 1939;64:409-44.
- [Google Scholar]
- National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: National High Blood Pressed Education Program c0 oordinating Committee.The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 Report. JAMA. 2003;289:2560-72.
- [Google Scholar]
- National Nutrition Monitoring Bureau (NNMB) In: Diet and nutritional status of population and prevalence of hypertension among adults in rural areas. NNMB Technical Report 24: Hyderabad: NNMB; 2006. p. :35-7.
- [Google Scholar]
- Prevalence & risk factors of pre-hypertension & hypertension in an affluent north Indian population. Indian J Med Res. 2008;128:712-20.
- [Google Scholar]
- Is the ‘rule of halves’ in hypertension still valid? - Evidence from the Chennai Urban Population study. J Assoc Physicians India. 2003;51:153-7.
- [Google Scholar]
- Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) JAMA. 2001;285:2486-97.
- [Google Scholar]
- The World Health Report 2002 - Reducing Risks, Promoting Healthy Life. Available from: http://www.who.int/whr/2002/en/
- [Google Scholar]
- STEPwise approach to surveillance (STEPS). WHO 2006. Available from: http://www.who.int/chp/steps/en/
- [Google Scholar]
- Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18:499-502.
- [Google Scholar]
- A simple, cost-effective quality assurance model for measurement of lipids in a large epidemiological study. Nat Med J India. 2008;21:279-83.
- [Google Scholar]
- Cardiovascular risk factor prevalence among men in a large industry of northern India. Natl Med J India. 2005;18:59-65.
- [Google Scholar]
- Hypertension in the native rural population of Assam. Natl Med J India. 2004;17:300-4.
- [Google Scholar]
- Prehypertension and mortality in a nationally representative cohort. Am J Cardiol. 2004;94:1496-500.
- [Google Scholar]
- Prehypertension and cardiovascular disease risk in the Women's Health Initiative. Circulation. 2007;115:855-60.
- [Google Scholar]
- The INTERSALT Study: background, methods, findings, and implications. Am J Clin Nutr. 1997;65(Suppl 2):626S-42S.
- [Google Scholar]
- A clinical trial of the effects of dietary patterns on blood pressure.DASH Collaborative Research Group. N Engl J Med. 1997;336:1117-24.
- [Google Scholar]
- Premier: a clinical trial of comprehensive lifestyle modification for blood pressure control: rationale, design and baseline characteristics. Ann Epidemiol. 2003;13:462-71.
- [Google Scholar]






