Translate this page into:
Prevalence & correlates of primary infertility among young women in Mysore, India
Reprint requests: Shri Paul C. Adamson, 513 Parnassus Ave, S-245, San Francisco, CA 94143-0454, USA e-mail: Paul.Adamson@ucsf.edu
-
Received: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
There are sparse data on the prevalence of primary infertility in India and almost none from Southern India. This study describes the correlates and prevalence of primary infertility among young women in Mysore, India.
Methods:
The baseline data were collected between November 2005 through March 2006, among 897 sexually active women, aged 15-30 yr, for a study investigating the relationship of bacterial vaginosis and acquisition of herpes simplex virus type-2 (HSV-2) infection. A secondary data analysis of the baseline data was undertaken. Primary infertility was defined as having been married for longer than two years, not using contraception and without a child. Logistic regression was used to examine factors associated with primary infertility.
Results:
The mean age of the women was 25.9 yr (range: 16-30 yr) and the prevalence of primary infertility was 12.6 per cent [95% Confidence Interval (CI): 10.5-15.0%]. The main factor associated with primary infertility was HSV-2 seropositivity (adjusted odds ratio: 3.41; CI: 1.86, 6.26).
Interpretation & conclusions:
The estimated prevalence of primary infertility among women in the study was within the range reported by the WHO and similar to other estimates from India. Further research is needed to examine the role of HSV-2 in primary infertility.
Keywords
HSV-2
India
infertility
reproductive health
sexually transmitted disease
The World Health Organization (WHO) estimates that 60 to 80 million couples worldwide currently suffer from infertility1. Infertility varies across regions of the world and is estimated to affect 8 to 12 per cent of couples worldwide23. Underlying these numbers exists a core group of couples, estimated to be 3 to 5 per cent, who are infertile due to unknown or unpreventable conditions. A prevalence of infertility above this level suggests preventable or treatable causes4. Infertility tends to be highest in countries with high fertility rates, an occurrence termed “barrenness amid plenty5”. Many studies have been conducted in the Africa, where the reported prevalence of infertility ranges from 9 per cent in Gambia to 30 per cent in Nigeria6.
Total infertility is divided into primary and secondary infertility. Definitions of primary infertility vary between studies, but the operational definition, put forth by the WHO, defines primary infertility as the “Inability to conceive within two years of exposure to pregnancy (i.e.- sexually active, non-contracepting, and non-lactating) among women 15 to 49 yr old7”. Secondary infertility refers to the inability to conceive following a previous pregnancy. Globally, most infertile couples suffer from primary infertility8.
Sexually transmitted infections (STIs) are generally considered the leading preventable cause of infertility worldwide, especially in developing countries26. STIs cause approximately 70 per cent of all pelvic inflammatory disease (PID) cases, which often result in tubal damage29. A large study conducted by the WHO in 25 countries, with over 5800 couples, found that over 85 per cent of the infertility among African women was attributable to infection, compared to only 33 per cent in women worldwide610.
Among Indian women reporting primary infertility and PID, STI prevalence was high3. The WHO estimates the overall prevalence of primary infertility in India to be between 3.9 and 16.8 per cent1. Estimates of infertility vary widely among Indian s0 tates from 3.7 per cent in Uttar Pradesh, Himachal Pradesh and Maharashtra11, to 5 per cent in Andhra Pradesh12, and 15 per cent in Kashmir13. Moreover, the prevalence of primary infertility has also been shown to vary across tribes and castes within the same region in India1114. However, it should be noted that many of these estimates use different definitions of infertility and consider different time periods, which makes direct comparisons difficult between any studies.
There are sparse data on the prevalence of primary infertility in India3 and almost none from southern India. The objectives of this study were to estimate the prevalence and describe the epidemiologic correlates of primary infertility within a sample of sexually active reproductive-age women in Mysore, the second largest city in the State of Karnataka, India.
Material & Methods
Study population: During November 2005-March 2006, young sexually active, non-pregnant women were recruited consecutively from CSI Holdsworth Memorial Hospital and Chitra's Hospital in Mysore, India. Detailed description of the recruitment of the study population is described elsewhere15. In total, 898 women were enrolled into a prospective study investigating the relationship between bacterial vaginosis (BV) and acquisition of herpes simplex virus-2 (HSV-2). Inclusion criteria for the women included age between 15 and 30 yr, sexually active (i.e. reporting unprotected vaginal intercourse at least once in the previous three months), non-pregnant and willingness to undergo a pelvic examination. The study was approved by the Committee for The Protection of Human Subjects at the University of California, Berkeley (Protocol #2005-4-95); and Asha Kirana Institutional Review Board, Mysore, India in compliance with all Federal regulations governing the protection of human subjects. All participants provided written informed consent.
Data collection: Trained study personnel interviewed participants using standardized questionnaires, and data regarding socio-demographics, behavioural and reproductive health characteristics were collected for the participant and their sexual partners. The study administered a validated questionnaire used in a previous study16. A trained clinician performed a pelvic examination and obtained biological specimens for STI screening. All women with STIs received free treatment according to 2005 CDC treatment guidelines17.
Laboratory assessment: A type-specific ELISA test was used to detect HSV-2 IgG antibodies (Focus Technologies, Cypress, CA, USA). Manufacturer's instructions were followed using an index value of >1.1 as positive HSV-2 specimen. Vaginal smears were assessed independently for BV by two trained technicians using the Gram stain Nugent score criteria of 0-3 for negative, 4-6 for intermediate, and 7-10 for positive18. Vaginal swabs were also cultured, using organism specific kits, for Trichomonas vaginalis, Candida species, and Neisseria gonorrhoeae, according to manufacturer's instructions (BioMed Diagnostics, OR, USA). All diagnostic tests were carried out in the microbiology laboratories of CSI Holdsworth Memorial Hospital and Vikram Hospital, Mysore.
Data analysis: Closely following the WHO definition of primary infertility, women were defined as having primary infertility if they were married (or with their main partner) for longer than two years, sexually active, not using modern contraception, and without children7. The prevalence of primary infertility and corresponding 95 per cent confidence intervals (CIs) were estimated. Secondary infertility was not measured.
Female characteristics were selected to test their association with our main outcome, primary infertility. Demographic variables including age in years and monthly household income were evaluated as continuous variables. Education, occupation, and religion were examined as categorical variables. Reproductive health variables including years sexually active, age at sexual debut, and number of unprotected sex acts in the prior three months were examined as continuous variables. The number of unprotected sex acts in the prior three months was transformed to the log scale to obtain a more symmetric distribution of the values. Complaints of current genital itching, burning with urination, and vaginal discharge were analyzed as binary variables. Upon physical examination, clinicians reported the presence of abnormal vaginal discharge and sores or boils as binary variables. Vaginal pH was recorded as a continuous variable, and considered to be high if the pH was >4.5.
All statistical analyses were conducted with Stata 9.0 (Stata Corporation, College Station, Texas, USA). Descriptive analyses were conducted using Pearson chi-squared or Fisher-exact tests for categorical variables and t tests for continuous variables. Logistic regression was used to calculate crude and age-adjusted odds ratios (OR) and corresponding 95 per cent CIs for selected covariates and primary infertility. All variables significant at the 10 per cent level in the age-adjusted model were included in the final multivariable model, which adjusted for possible confounders. Vaginal pH, age at sexual debut and age at menarche, were excluded from the multivariable analysis due to strong correlations with candidiasis and age in univariate analysis.
Results
Of the 996 eligible women, 898 (90.0%) completed all baseline procedures; one participant was excluded from analyses due to incomplete data, resulting in a sample size of 897. The mean age of participants was 25.9 ± 3.12 yr (median= 26 yr; range: 16-30 yr). Nearly all of the women reported being married (97.9%). Most women reported their primary occupation to be housewife (74.9%), and over half reported their religion as Hindu (60.1%). The mean income was  2,892 (CI: 2,709-3,075) or approximately US $ 66.
2,892 (CI: 2,709-3,075) or approximately US $ 66.
The prevalence of primary infertility within this group of women at baseline was 12.6 per cent (n = 113; 95% CI: 10.5-15.0%). The mean monthly family income of the infertile group was higher than among the fertile group (P<0.05). Only two women reported ever using alcohol or cigarettes. Compared to fertile women, infertile women tended to be younger, sexually active for a shorter period of time, older at sexual debut, and had been with their sex partners for a shorter duration (Table I). Analysis of reported partner data did not show any differences between the two groups of women (data not shown).

Overall, infertile women were less likely to have abnormal vaginal discharge, or report burning during urination and vaginal itching (Table II). Women in the fertile group were more likely to have a vaginal pH level of 4.5 or higher (P=0.04). The prevalence of HSV-2 seropositivity among women with primary infertility was 19.5 per cent (22/113), compared to 10.3 per cent (81/784) among the fertile women (P<0.01); the overall prevalence of HSV-2 within this group was 11.5 per cent (103/897) (Table II). Among HSV-2 positive women with primary infertility genital lesions or ulcers were absent in 96.1 per cent (99 of 103) of the women.
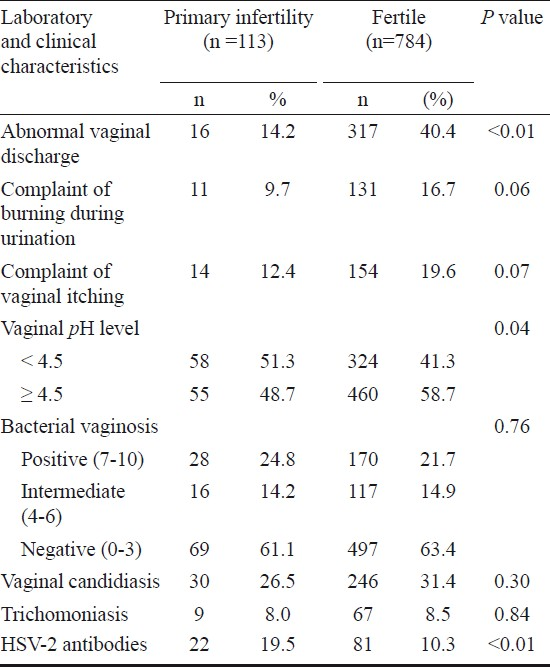
The prevalence of BV was 22.1 per cent (198/897) among the women, but did not differ between the two groups. Similarly, the prevalence of T. vaginalis did not differ between the two groups and the overall prevalence was 8.5 per cent (76/897). The prevalence of Candidiasis was 30.8 per cent (276/897), and was not statistically different between the two groups (Table II). No cases of N. gonorrhoeae infection were identified.
The age-adjusted logistic regression for selected variables is shown in Table III. Post-secondary education, unprotected sex acts in the previous three months, vaginal pH, abnormal vaginal discharge, and burning during urination were all associated with primary infertility in the age-adjusted analyses. In the multivariable model, abnormal vaginal discharge, HSV-2 seropositivity, unprotected sex acts in the previous three months, and vaginal pH were all significantly associated with primary infertility. However, vaginal pH was excluded from the multivariable model as this variable was highly associated with candidiasis.

Women with abnormal vaginal discharge were at decreased odds of infertility (adjusted OR: 0.25; 95% CI: 0.14, 0.45) compared to women without abnormal discharge, adjusting for other variables in the model. Similarly, increasing age was associated with decreased odds of primary infertility (aOR: 0.79; 95% CI: 0.73, 0.85). Women who were positive for HSV-2 antibodies were at increased odds of infertility (aOR: 3.41; 95% CI: 1.86, 6.26) compared to women who were seronegative. The log-transformed number of unprotected sexual acts in the previous three months was positively associated with primary infertility (aOR: 1.71; 95% CI: 1.23, 2.37).
Discussion
The WHO estimates of primary infertility in India are 3.9 per cent (age-standardized to 25-49 yr) and 16.8 per cent (age-standardized to 15-49 yr), using the “age but no birth” definition1. The prevalence of primary infertility in the current study of young women was 12.6 per cent, which is within the range reported by the WHO and similar to estimates from the Kashmir region113. Our prevalence estimate is higher than reports from other Indian regions1112. Estimates of infertility prevalence have been shown to vary across regions within a country; thus, our findings add to the limited data on infertility from south Indian populations.
Our analysis revealed that HSV-2 seropositivity was significantly associated with primary infertility in this group of young, reproductive-age women in Mysore, India. Cherpes et al19 have also demonstrated an association between HSV-2 infection and PID. Two mechanisms were suggested for infertility caused by HSV-2 infection: lower-genital tract ulcerations caused by HSV-2 infection increase the spread of lower genital tract pathogens to the upper genital tract, thereby facilitating PID or HSV-2 infections may increase host inflammatory responses in the upper genital tract, leading to tubal damage19. Other studies have found HSV-2 DNA associated with low sperm counts and decreased sperm motility in men attending infertility clinics20–22. The majority of HSV-2 infections among men and women are asymptomatic, emphasizing the importance of screening and detection of HSV-2 infection20. The prevalence of HSV-2 infection was 11.5 per cent, and many of these women had concurrent T. vaginalis infection and BV, as reported elsewhere23. Consistent with previous studies, we found no association between primary infertility and Candida infection, T. vaginalis infection, and BV24.
Women with primary infertility reported higher levels of education, and these women also reported an older age at first sex, which may point to a delay in marital status and sexual debut associated with educational attainment. Further, infertile women reported higher family incomes than fertile women, consistent with previous findings in India11. It is likely that women from higher income families were able to access healthcare because they could afford to pay for services more than women from lower income families.
Among women in our study, unprotected sex acts were significantly associated with primary infertility, possibly by increasing the likelihood of contracting a STI from their partner. However, it is also possible that couples without children may be actively trying to conceive by increasing the number of unprotected sexual acts, which may account for this association.
Additionally, lower odds of infertility were associated with abnormal vaginal discharge among women in our study. While a biological explanation of this observation seems unlikely, one possible explanation is that women who have a history of abnormal vaginal discharge may be more likely to seek reproductive health services by enrolling in our study.
Our results should be interpreted in light of the following limitations. The definition of primary infertility used in our study differed from the definition put forth by the WHO in two main aspects. First, the age range of women in our study, 16-30 yr, was different than the range used by the WHO, 15-49 yr. Second, the administered study questionnaire only obtained information about current contraceptive use, and as such, we were unable to estimate the length of time the women had not been using contraception. However, national survey data showed that contraceptive use among young, married women is low and less than 13 per cent of married women reported ever using modern contraception before having their first child25. The data obtained through the questionnaire were also self-reported and retrospective in nature. Women were enrolled through outreach programmes in specific communities in Mysore and our results may not be generalizable to other populations. Another limitation was the cross-sectional analysis of baseline data; thus, it was not possible to determine temporality or causality of the associations between primary infertility and the select covariates. The HSV-2 ELISA test detected only IgG antibodies in the serum, which did not allow to determine if these infections were recent. Due to funding limitations, we were unable to test for C. trachomatis and were unable to examine its association with primary infertility.
Despite these limitations, our study also has several strengths including a large sample size and use of standardized laboratory diagnosis for STIs. HSV-2 seropositivity was found to be significantly associated with primary infertility in this group of women. Further research is needed to illuminate the associations between HSV-2 seropositivity and primary infertility, which may have clinical relevance. Our findings highlight the importance of infertility as a public health issue. These data can be used to guide future reproductive health programmes in the region.
Acknowledgment
This work was supported by the Fogarty AIDS International Training and Research Program at University of California, Berkeley [Grant 1-D43-TW00003-16]. The authors thank Maureen Lahiff and Lee Riley at UC Berkeley, who provided technical expertise and manuscript editing and Dr P.S.S. Sundar Rao for critical review of the final manuscript. Authors acknowledge Focus Technologies, Cypress, CA, USA, for providing HSV-2 Herpeselect ELISA kits. BioMed Diagnostics, White City, OR, USA for Trichomonas Vaginalis and Neisseria gonorrhoea test kits and Yeast growth medium, and Cipla, Mumbai, India, for oral Acyclovir.
References
- World Health Organization. In: Infecundity, infertility, and childlessness in developing countries. DHS Comparative Reports No 9. Calverton, Maryland, USA: ORC Macro and the World Health Organization; 2004.
- [Google Scholar]
- Infertility: an international health problem. Int J Gynaecol Obstet. 1994;46:155-63.
- [Google Scholar]
- Population Council. Infertility. In: Looking back, looking forward: a profile of sexual and reproductive health in India. New Delhi: Population Council; 2004. p. :67-72.
- [Google Scholar]
- Quality of infertility care in poor-resource areas and the introduction of new reproductive technologies. Hum Reprod. 2001;16:215-9.
- [Google Scholar]
- Infertility and the provision of infertility medical services in developing countries. Hum Reprod Update. 2008;14:605-21.
- [Google Scholar]
- World Health Organization. In: Reproductive health indicators for global monitoring: Report of the second interagency meeting, 2001. Geneva: World Health Organization; 2001. p. :23.
- [Google Scholar]
- Global infertility and the globalization of new reproductive technologies: illustrations from Egypt. Soc Sci Med. 2003;56:1837-51.
- [Google Scholar]
- Patterns and predictors of infertility among African women: a cross-national survey of twenty-seven nations. Soc Sci Med. 1996;42:209-20.
- [Google Scholar]
- Prevalence of infertility in different population groups in India and its determinants. In: In: Statistics and demography. New Delhi: National Institute of Health & Family Welfare & Indian Council of Medical Research; 1986.
- [Google Scholar]
- Childlessness in Andhra Pradesh, India: Treatment-seeking and consequences. Reprod Health Matters. 1999;7:54-64.
- [Google Scholar]
- Epidemiologic and etiologic aspects of primary infertility in the Kashmir region of India. Fertil Steril. 1997;68:637-43.
- [Google Scholar]
- Prevalence of female infertility and its socio-economic factors in tribal communities of Central India. Rural Remote Health. 2007;7:456.
- [Google Scholar]
- Novel recruitment strategies to increase participation of women in reproductive health research in India. Globe Public Health. 2007;2:395-403.
- [Google Scholar]
- Alcohol use by men is a risk factor for the acquisition of sexually transmitted infections and human immunodeficiency virus from female sex workers in Mumbai, India. Sex Transm Dis. 2005;32:685-90.
- [Google Scholar]
- Sexually transmitted diseases treatment guidelines, 2006. MMWR Recomm Rep. 2006;55:1-94. (RR-11)
- [Google Scholar]
- Reliability of diagnosing bacterial vaginosis is improved by a standardized method of gram stain interpretation. J Clin Microbiol. 1991;29:297-301.
- [Google Scholar]
- The associations between pelvic inflammatory disease, Trichomonas vaginalis infection, and positive herpes simplex virus type 2 serology. Sex Transm Dis. 2006;33:747-52.
- [Google Scholar]
- Reactivation of genital herpes simplex virus type 2 infection in asymptomatic seropositive persons. N Engl J Med. 2000;342:844-50.
- [Google Scholar]
- Prevalence of sexually transmissible pathogens in semen from asymptomatic male infertility patients with and without leukocytospermia. Fertil Steril. 2007;87:1087-97.
- [Google Scholar]
- Detection of herpes simplex virus, cytomegalovirus, and Epstein-Barr virus in the semen of men attending an infertility clinic. Fertil Steril. 2003;79(Suppl 3):1566-70.
- [Google Scholar]
- The epidemiology of herpes simplex virus type-2 infection among married women in Mysore, India. Sex Transm Dis. 2007;34:935-7.
- [Google Scholar]
- Genital tract infections and infertility. Eur J Obstet Gynecol Reprod Biol. 2008;140:3-11.
- [Google Scholar]
- International Institute for Population Sciences (IIPS) and Macro International. In: National family health survey (NFHS-3), 2005-06: India. Vol I. Mumbai: IIPS; 2007. p. :120-30.
- [Google Scholar]






