Translate this page into:
Preparedness of public & private health facilities for management of diabetes & hypertension in 19 districts in India
For correspondence: Dr Vani Srinivas, ICMR-National Centre for Disease Informatics and Research, Bengaluru 562 110, Karnataka, India e-mail: vani.srinivas@icmr.gov.in
-
Received: ,
Accepted: ,
Abstract
Background & objectives
India has the second highest number of adults with diabetes in the world, and more than one-fourth of adults have hypertension. This article describes the preparedness of public and private health facilities for type 2 diabetes mellitus and hypertension management.
Methods
A cross-sectional survey of the health facilities was conducted in 19 districts of seven States in India, which included an assessment of both public and private health facilities. We used the Indian Public Health Standards and other relevant guidelines for assessment. The service domain score for four domains: equipment, medicine, diagnostics capacity, staff, including the availability of guidelines, and overall readiness score, was calculated following the Service Availability and Readiness Assessment manual of the World Health Organisation. The study considered a readiness score of ≥70 per cent to classify a facility as prepared for providing hypertension and diabetes services.
Results
Out of 415 health facilities covered in the survey, 75.7 per cent were public facilities. Most were primary care facilities (57.6%) and were located in rural areas (53.3%). The overall readiness score for providing hypertension and diabetes services was lowest for Sub-Centres (SCs; 61%) and Community Health Centres (CHCs; 59%), compared to other facilities. The readiness score for public Primary Health Centres (PHCs) and private primary care facilities (level 2) was 73 and 57 per cent, respectively. The readiness score of district hospitals, government private medical colleges, and other private tertiary care facilities was above 70 per cent, and they were considered prepared for services.
Interpretations & conclusions
PHCs were better prepared for diabetes and hypertension care than SCs, CHCs, and SDHs. By ensuring adequate human resources availability and uninterrupted supply of essential medicines, programme managers can further improve the preparedness of all public health facilities.
Keywords
Diabetes
hypertension
health facilities
India
non-communicable diseases
India has the second highest number of adults with diabetes (20-79 yr) in the world, and approximately three per cent of the total deaths in India in 2019 were attributed to diabetes1. As per the National non-communicable disease (NCD) monitoring survey (NNMS), 2017-18, the prevalence of diabetes and hypertension among adults aged 18 to 69 yr was 9.3 and 28.5 per cent, respectively2. India is also committed to the Sustainable Development Goal (SDG) to achieve target 3.4, aiming at a one-third reduction relative to 2015 levels in the probability of dying between 30 and 70 yr of age from cancers, cardiovascular diseases, chronic respiratory diseases, and diabetes by 20303. Thus, to tackle the rising burden of NCDs, a National NCD Monitoring Framework was developed and is targeting to provide 50 per cent availability of generic drugs to prevent heart attacks and strokes at the primary health care level and also ensure availability and affordability of quality, safe, and efficacious essential NCD medicines and basic technologies to treat and diagnose major NCDs in 80 per cent of public and private health facilities4. However, worldwide trends in NCD mortality assessment indicate slow progress, and the rate of decline in mortality in India is not sufficient to meet the SDG target5. To accelerate the progress, various initiatives have been taken by the government, such as population-based screening and opportunistic screening at health facilities6-8. These initiatives are contributing to the diagnosis of a large number of diabetes and hypertension cases across the country9. As diabetes and hypertension are contributing to a substantial NCD burden in India10, it is imperative to study the preparedness of various levels of health facilities for service delivery. A considerable reduction in mortality due to hypertension and diabetes requires the availability of essential medicines, trained staff, equipment, and diagnostic services11. A national-level survey can inform programme managers regarding the preparedness of health facilities.
This paper describes the preparedness of public and private health facilities for managing type 2 diabetes mellitus and hypertension and the scope for improving the service delivery across the different levels of health facilities in India.
Materials & Methods
This cross-sectional study was undertaken by the Indian Council of Medical Research-National Institute of Disease Informatics and Research (ICMR-NCDIR), Bengaluru. The study was approved by the ICMR-NCDIR Institutional Ethics Committee. All implementing agencies obtained their respective institutional ethics approvals. Written informed consent was obtained from all the facility-in-charge.
Study implementation
ICMR-NCDIR was the Central Coordinating Unit (CCU), and six State implementing agencies were involved in liaising with State authorities and collecting data.
Study design and setting
A cross-sectional survey of the health facilities was conducted in two phases. The first phase was conducted from September 15, 2021 to December 15, 2021, and the second phase was from February 1, 2023 to June 30, 2023. In consultation with the State and district NCD nodal officials, one State and a few districts in each region were randomly selected. The study was conducted in seven States and 19 districts of India, as depicted in supplementary figure.
Sampling and sample size
Primary level health facilities [Sub Centres (SC)-level 1 and Primary Health Centre (PHC) - Level 2] and secondary level public health facilities [Community health centres (CHC)-Level 3, Sub District Hospital (SDH)-Level 4 and District Hospital (DH) Level-5] were selected in three different blocks of each district. Three blocks from each district with different programmatic performance (high, moderate, and low) were selected based on Health Management Information System (HMIS) data for October 2021 (Phase-1) and April 2023 (Phase-2). The indicator for the selection of blocks was the total number of confirmed cases diagnosed with diabetes, hypertension, and both conditions during the month preceding the survey. This was done to prevent selecting only well-performing health facilities within the districts. Care was taken to identify the linked facilities within three blocks, assuming the referral and follow up were done between the facilities. The government (GMC), private medical colleges (level-6), and State-owned tertiary care facilities were selected purposively from each district for assessment. This was based on the availability of tertiary care facilities within the district.
Selection of private health facilities
Health facilities not owned or supported by the government and those that are for-profit were considered private health facilities. The facilities providing day care services, managed by Medical Graduates (MBBS) were considered private primary care facilities (level-2), and facilities managed by specialists (physician/s and surgeons) and within-patient or admission facilities (5 to 30 in-patient beds) were considered private secondary care facilities (level-3), private care facilities having >30 in-patient beds and <50 bed were considered private secondary care facilities (level-4). Large hospitals like medical colleges, corporates, or super-speciality hospitals, with the availability of all specialists and some super-specialists (cardiologists and endocrinologists), were considered tertiary care facilities (level-6).
A few private health facilities with a high case load were selected for assessment. Based on permission for assessment, the survey included these facilities.
Survey instruments
The primary and secondary level health facilities survey tools were developed referring to the National NCD programme guidelines and the Indian Public Health Standards (IPHS) 2012 and 2022 guidelines. The availability of human resources, medicines, equipment, and diagnostics varied across health facilities. IPHS standards were used to assess primary and secondary level facilities. The standards for assessment (diagnostic and equipment) for tertiary care facilities were based on the World Health Organization (WHO) standards12, and staff standards were based on the National Medical Council guidelines.
The tool also included information on in-and-out referrals, follow ups, and the number of cases treated in the outpatient departments (OPDs). The same study tool was used to assess public and private health facilities. A pilot study was undertaken for a week in October 2021 (Phase-1) and April 2023 (Phase-2) of the survey, and instruments were finalised based on the findings of pilot testing.
Quality assurance
The survey followed quality assurance mechanisms to ensure the completeness, correctness, and reliability of survey data. All investigators and data collectors were trained on study methods, tools, and ethical aspects of the study.
Data collection
The data were collected in handheld devices using the Computer Assisted Personal Interviews. Face-to-face interviews were done in health facilities. Information on the availability of human resources, training status, and NCD services was collected from the facility-in-charge; information on medicines and technologies was collected from the storekeeper or the pharmacist; and information on laboratory services was collected from the laboratory technicians. Equipment availability was assessed by field investigators by observation and review of records. Information on follow up and referral was collected from the facility-in-charge, and data collectors reviewed programme records. Information on various modes of follow ups (home visit, self-visit by patient, and telephonic follow up, etc.) was collected from the health facility-in-charge.
Data analysis
The data received at CCU were reviewed for their quality. The cleaned data sets were subject to analysis. The analysis specific to service readiness for CVDs and diabetes was carried out following the WHO’s Service Availability and Readiness Assessment (SARA) manual13, using Microsoft Excel 2016. The continuum of care component of this study was analysed using SPSS version 26.0 (USA Chicago).
The domain-wise scores and readiness scores for each type and level of health facility were calculated (steps are in Supplementary file). The domain and readiness scores for diabetes and hypertension were taken together for analysis. The steps for calculations have been given in the supplementary file. The study considered a readiness score of ≥70 per cent to classify a facility as prepared for providing hypertension and diabetes services.
Results
In two phases of data collection, 415 health facilities were covered, of which 75.7 per cent were public and 24 per cent were private (Table I). The number of facilities assessed varied across the States. More than half (57.6%) of the health facilities assessed were primary level (33.5%), followed by secondary (33.5%) and tertiary (10%) facilities. More than half (56.3%) of health facilities were in rural areas.
| State | No. of districts covered$ | Public health facilities | Private facilities | Total | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Primary; n (%) | Secondary; n (%) | Tertiary; n (%) | Pvt. primary/NGO/CSO | Pvt secondary/NGO/CSO | Pvt medical college | Pvt tertiary | ||||||
| SC/HWC | PHC/UPHC/HWC | CHC/UCHC | SDH | DH | Govt., Medical College# | |||||||
| Haryana | 2 | 4 (9.8) | 11 (11) | 7 (11.6) | 3 (14.2) | 2 (13.3) | 1 (7.14) | 0 | 9 (20.9) | 1 (25) | 3 (15.0) | 41 |
| Karnataka | 3 | 15 (21.7) | 12 (17.4) | 8 (11.6) | 7 (10.1) | 3 (4.3) | 5 (7.2) | 7 (10.1) | 6 (8.7) | 3 (4.3) | 3 (4.3) | 69 |
| Meghalaya | 2 | 11 (25) | 10 (22.7) | 6 (13.6) | 1 (2.3) | 2 (4.5) | 2 (4.5) | 6 (13.6) | 1 (2.3) | 0 | 5 (11.4) | 44 |
| Odisha | 4 | 23 (27.4) | 30 (35.7) | 13 (15.5) | 2 (2.4) | 3 (3.6) | 1 (1.2) | 3 (3.6) | 9 (10.7) | 0 | 0 (0.0) | 84 |
| Rajasthan | 3 | 18 (23.7) | 12 (15.8) | 11 (14.5) | 3 (3.9) | 2 (2.6) | 3 (3.9) | 9 (11.8) | 9 (11.8) | 0 | 9 (11.8) | 76 |
| Madhya Pradesh | 3 | 19 (33.9) | 11 (19.6) | 9 (16.1) | 5 (8.9) | 1 (1.8) | 1 (1.8) | 5 (8.9) | 5 (8.9) | 0 | 0 (0.0) | 56 |
| Chhattisgarh | 2 | 15 (33.3) | 14 (31.1) | 6 (13.3) | 0 | 2 (4.4) | 1 (2.2) | 3 (6.7) | 4 (8.9) | 0 | 0 (0.0) | 45 |
| Total | 19 | 105 (25.3) | 100 (24.1) | 60 (14.5) | 21 (5.1) | 15 (3.6) | 14 (3.4) | 33 (8) | 43 (10.4) | 4 (1) | 20 (4.8) | 415 |
$ Name of the districts covered in each State . Haryana (Faridabad and Bhiwani), Karnataka (Bangalore urban, Tumkur and Mysore), Rajasthan (Jodhpur, Ajmer and Alwar), Meghalaya (East Kashi Hills)and Odisha (Mayurbhanj) were covered in phase-1 of study. Meghalaya West Garo hills), Odisha, (Puri, Nayagarh and Ganjum), Madhya Pradesh (Sehore, Vidisha and Annupur) and Chhattisgarh (Durg and Kanker) were State and districtscovered in phase II of the study. #includes two State owned super specialty hospitals in Karnataka. @Out of 105 SC assessed, 55 (52.3%) were transformed to Health and Wellness Centre (HWC) and out of 100 PHC assessed, 64 (64%) were transformed to HWC. Urban Primary Health Centre (UPHC),SC, sub-centres; HWC, health and wellness centre; CHF, community health centre; SDH, sub-district hospitals; DH, district hospitals (DH)
Figure (A-F) provides details of the mean domain score and readiness index of different levels of health facilities providing diabetes mellitus (DM) and hypertension (HT) services.
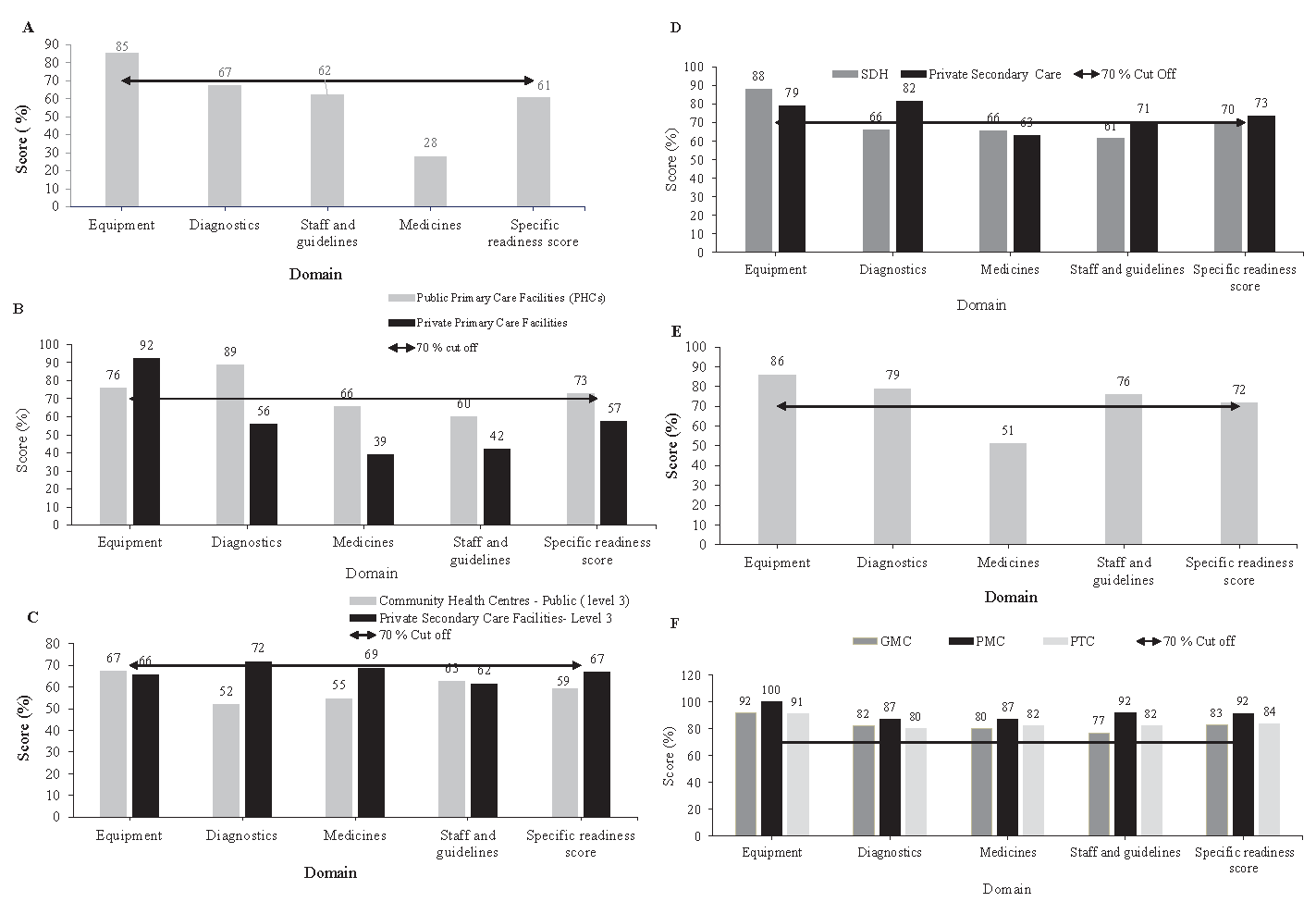
- Service domains score and mean readiness scores of health facilities that offered diabetes and hypertension care services to provide services related to diabetes mellitus(DM)and hypertension (HT)in India (2021 & 2023). (A) Sub-centres (SC) (level-1). (B) Primary health centres (PHC) and private primary care health facilities (level-2). (C) Community Health Centres (CHC) and private secondary care health facilities (level-3). (D) Sub-District Hospitals (SDH) and private secondary care health facilities (level-4). (E) District hospitals (DH) (level-5). (F) Government medical college (GMC), private medical college and private tertiary care (level-6).
The overall readiness score for providing services for hypertension and diabetes was between 57 per cent (lowest for private care facilities-level 1) and 92 per cent (private medical colleges, level-6).
More than three-fourths of all public and private health facilities reported being involved in the follow up of diabetes and hypertension patients (Table II). The most common mode of follow ups across all facilities was self-reporting by patients (61.4 to 100%), except for in SCs (29.5%). At SCs, the most common mode of follow up was home visits by health workers (60.4%). The availability of out-referral and in-referral registers across all levels and types of facilities was between 25 to 53.8 per cent and 14 to 61.5 per cent, respectively.
| Public health facilities | Private health facilities | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Primary; n (%) | Secondary; n (%) | Tertiary; n (%) | Pvt primary | Pvt secondary | Pvt medical college | Pvt tertiary | ||||
| Sub-centre/HWC | PHC/UPHC | CHC/UCHC | SDH | DH | Govt. medical college | |||||
| Reported follow up at health facility | 64 (61) | 77 (77) | 45 (75) | 16 (76.2) | 14 (93.3) | 12 (92.3) | 28 (82.4) | 38 (88.4) | 4 (100) | 16 (80) |
| Follow up method adopted by facilities | ||||||||||
| Home visit by health workers | 62 (59) | 30 (30) | 11 (18.3) | 5 (23.8) | 2 (13.3) | 1 (7.7) | 2 (5.9) | 1 (2.3) | 0 | 0 |
| Send SMS alerts/telephone to patient | 1 (1) | 8 (8) | 6 (10) | 2 (9.5) | 1 (6.7) | 0 | 1 (2.9) | 4 (9.3) | 0 | 4 (20) |
| Self-reported by patients | 31 (29.5) | 54 (5) | 38 (63.3) | 13 (61.9) | 12 (80) | 12 (92.3) | 27 (79.4) | 34 (79.1) | 4 (100) | 16 (80) |
| Availability of records | ||||||||||
| Out-referral registers | 55 (52.4) | 48 (48.0) | 27 (45.0) | 11 (52.4) | 4 (26.7) | 7 (53.8) | 7 (20.6) | 8 (18.6) | 2 (50) | 5 (25) |
| In referral registers | 20 (19) | 33 (33) | 18 (30) | 10 (47.6) | 6 (40) | 8 (61.5) | 6 (17.6) | 6 (14) | 1 (25) | 8 (40) |
| Reporting of NCD programme statistics# | 67 (63.8) | 84 (84) | 46 (76.7) | 17 (81) | 12 (80) | 6 (46.2) | NE | NE | NE | NE |
| Total | 105 (100) | 100 (100) | 60 (100) | 21 (100) | 15 (100) | 13 (100) | 34 (100) | 43 (100) | 4 (100) | 20 (100) |
#applicable for public health facilities only. NE, not expected for the level of facility. SMS, short message service; NCD, non-communicable diseases; Pvt, private
Most public health facilities (from SC to SDH) reported stockouts of essential medicines for managing diabetes and hypertension (Table III). Out of 105 SCs assessed, nearly one-third of health facilities (37/105; 35.2%) reported stockouts of tablet metformin, and nearly less than half (47/105; 44.8%) reported stockouts of tablet amlodipine.
| Public health facilities reporting stock outs$ of essential medicines | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| SC | PHC | CHC | SDH | DH | GMC | |||||||
| List of essential medicines | No. of facilities Stockouts; n (%)^ | Duration of stock-outs# | No. of facilities Stockouts; n (%) | Duration of stock-outs# | No. of facilities Stockouts; n (%) | Duration of stock-outs# | No. of facilities Stockouts; n (%) | Duration of stock-outs# | No. of facilities Stockouts n (%) | Duration of stock-outs# | No. of facilities Stockouts n (%) | Duration of stock-outs# |
| Antidiabetic medicines | ||||||||||||
| Tab glimepiride | 53 (50.5) | 3 | 12 (12) | 3 | 3 (5) | 1 | 1 (4.8) | 1 | 2 (13.3) | 8 | 0 (0.0) | 0 |
| Tab metformin | 37 (35.2) | 7 | 6 (6) | 2 | 5 (8.3) | 1 | 1 (4.8) | 1 | 0 | 0 | 1 (7.7) | 0 |
| Insulin injection | NE | 4 (4) | 2 | 4 (6.7) | 3 | 1 (4.8) | 1 | 0 | 0 | 0 (0.0) | 0 | |
| Antihypertensive medicines | ||||||||||||
| Tab atenolol | 72 (68.5) | 4 | 29 (29) | 5 | 16 (16) | 4 | 2 (9.5) | NR | 3 (20) | NR | 1 (7.7) | 4 |
| Tab. amlodipine | 47 (44.8) | 7 | 23 (23) | 5 | 3 (5) | 2 | 1 (4.8) | NR | 1 (6.7) | 1 | 0 (0.0) | 0 |
| Tab enalapril | 70 (66.7) | 5 | 30 (30) | 1 | 5 (8.3) | 3 | 2 (9.5) | 3 | 0 | 0 | 0 | 0 |
| Tab frusemide | 33 (31.4) | 1 | 25 (25) | 6 | 12 (12) | 5 | 2 (9.5) | 3 | 1 (6.7) | 0 | 0 (0.0) | 0 |
| Tab chlorothiazide | 44 (41.9) | NR | 45 (45) | 6 | 3 (5) | 6 | 6 (28.6) | 3 | 4 (26.7) | NR | 1 (7.7) | 1 |
| Total | 105 | 100 | 60 | 21 | 15 | 13 | ||||||
$The stock outs of medicine was assessed for last one year preceding the survey.# mean duration of stockouts in months. NE, not Expected at that level of facility; NR, not reported by health facilities.^ Out of 105 SCs, 53 (50.5%) reported stock outs of Glimepiride , for an average duration of 3 months
The median duration of the stockouts for the medicines ranged from one to seven months. The SCs had reported more stockouts of essential anti-diabetes and anti-hypertensive medicines compared to any other types of facilities. These medicines were better available at government medical colleges compared to any other levels of public health facilities.
Discussion
Our findings suggest that among public health facilities, PHCs, district hospitals, and government medical colleges in India were better prepared to manage services for diabetes and hypertension. Across all the facilities, the domain score for equipment was the highest, and for medicines it was the lowest. However, the availability of all medicines was better at tertiary care facilities (public and private) compared to other levels of public health facilities.
The previous National-level survey, (NNMS, 2017-18)14, State-specific surveys in Madhya Pradesh (2013)15 and Manipur (2021)16, had reported that PHCs were less prepared for diabetes and hypertension care. Our results showed that the readiness score of PHCs was better as compared to the previous studies.
Other studies in Kolar (2016-17)17 and Mysore (2017-18) districts of Karnataka, Kerala, and Odisha (2018)18-20 had reported challenges in follow up visits, regular care, supply of medicines, health personnel, and laboratory supplies. They also noted that NCD-related health and curative services were more available at district headquarters than at sub-district level facilities. India Hypertension Control Initiative (IHCI) project, in 24 intervention districts (2018-19), had demonstrated that 50 per cent of hypertensive patients don’t return for follow ups in public health facilities21.
Some of these findings differed from our study, as we found that most public health facilities reported regular patient follow up. Some other findings, such as the availability of better curative services at the district headquarters level, were in agreement with previous studies.
Earlier studies from South India (2018) reported less than 10 per cent of household survey respondents getting their diabetes and hypertension medicines from a government hospital or PHC, and nearly 76 per cent of patients were buying medicines from private pharmacies22. These findings are discordant with the findings of our study and the domain score for availability of medicines at PHCs was better (66%), even though not up to mark.
We found a shortage of specialists at the CHC-level and these findings were similar to the rural health statistics report of 2020-21, indicating a shortfall of physicians (82.2%) and surgeons (83.2.9%) at the CHC-level23. Similar studies conducted in the tribal districts (2015-18) of India reported significant gaps in the availability of a trained workforce, drugs, laboratory services, and lack of clinical protocols for service delivery24. Some of these findings are concordant with that of our study.
ICMR-India Diabetes Study (ICMR-INDIAB) reports evidence of an NCD epidemic spreading to rural areas in India in addition to the urban areas due to the changes in lifestyle25. Therefore, improving the preparedness of SCs will further enhance the primary care services closer to the homes of the people. The Government of India has already accelerated its efforts towards strengthening Comprehensive Primary Health Care (CPHC) for achieving Universal Health Care by committing resources and efforts through the Prime Minister’s flagship Ayushman Bharat Health and Wellness programme (AB-HWCs). These were recently renamed as ‘Ayushman Arogya Mandirsʼ26. During our assessment, the majority of PHCs (64%) were converted to Health and Wellness Centres (HWCs). This indicates that PHC-HWCs were better prepared to provide comprehensive services compared to SCs, as nearly half of them (52.3%) were transformed into HWCs. However, we found that diagnostic services were less available at district hospitals, indicating that secondary higher-level public health facilities were not fully prepared to manage complications of these two conditions. Efforts to strengthen diagnostic services are essential for the continuum of care, as there will be in-referrals of patients from peripheral public health facilities to DHs. Lessons from the India Hypertension Control Initiatives (IHCI) project can be adapted to ensure reliable drug supply and accurate information systems in primary health care facilities27,28.
The present investigation indicates improved services have come in place over time, especially at the PHC level. The expanded care of services at HWCs ensured better diagnostic and equipment; however, the domain score for medicines, staff and guidelines was found to be less than 70 per cent at PHCs. These findings are useful for programme managers and policymakers. By ensuring an adequate, uninterrupted supply of essential medicines and required staff, the programme managers can further improve the preparedness of all levels of facilities for NCD care.
The strength of the current study was the assessment of all levels and all types of health facilities. Most of the earlier studies done in India had not involved the SCs, SDHs, and tertiary level facilities. This study provides information on the preparedness of all levels of public and private health facilities and indicates care domains to be improved for preparedness of services for diabetes and hypertension care in India.
The study was carried out in the selected geographical areas of seven States. Therefore, generalisability to other States could be limited since services, such as ensuring the free availability of drugs and diagnostics in public facilities, are subject to State-level policies and programme management. The pooled analysis was done for SC and SC-HWC, PHCs and PHC-HWCs. The disaggregated analysis of HWC and non-HWC facilities would have given different results. The number of private health facilities assessed was less compared to government health facilities.
The study concludes that PHCs were better prepared for diabetes and hypertension care than SCs, CHCs, and SDHs. By ensuring adequate human resources availability and uninterrupted supply of essential medicines, programme managers can further improve the preparedness of all levels of public health facilities to achieve SDG targets.
Acknowledgment
Authors acknowledge all the experts for providing input to improve the technical aspects of the study. Author acknowledges the support extended by State Health Departments and city municipal corporations for facilitating the surveys. Authors also acknowledge and thank Dr Sanjeev Kumar, Additional Professor, All India Institute of Medical Sciences, Bhopal, for facilitating data collection in three districts of Madhya Pradesh. Further, authors also acknowledge all the health facilities staff across the seven States for providing the required information to complete the survey.
Financial support &sponsorship
The study was supported by the NCD Division of the World Health Organization, India, Country Office, New Delhi [2021/1159110-0 /PO 202734269 (round -1) and 2023/1318974-0 /PO-203067469 (round -2)].
Conflicts of Interest
None.
Use of Artificial Intelligence (AI)-Assisted Technology for manuscript preparation
The authors confirm that there was no use of AI-assisted technology for assisting in the writing of the manuscript, and no images were manipulated using AI.
References
- IDF Diabetes Atlas 2021. Available from: https://diabetesatlas.org/atlas/tenth-edition/, accessed on June 2, 2024.
- National noncommunicable disease monitoring survey (NNMS) 2017-18. Available from: https://www.ncdirindia.org/nnms/, accessed on June 2, 2024.
- National Health Policy, 2017. Available from: https://mohfw.gov.in/sites/default/files/9147562941489753121.pdf, accessed on June 2, 2024.
- National action plan and monitoring framework for prevention and control of noncommunicable diseases (NCDs) in India. Developed through the WHO-Government of India 2012-13 Biennial workplan. Available from: https://cdn.who.int/media/docs/default-source/searo/india/health-topic-pdf/national-action-plan-and-monitoring-framework-prevention-ncds.pdf?sfvrsn=d7826a3f_2, accessed on on June 2, 2024.
- NCD countdown 2030: Worldwide trends in non-communicable disease mortality and progress towards sustainable development goal target 3.4. Lancet. 2018;392:1072-88.
- [CrossRef] [PubMed] [Google Scholar]
- Training module for staff nurses on population based screening of common non-communicable diseases. Available from: https://mohfw.gov.in/sites/default/files/Training%20Module%20for%20Staff%20Nurses%20on%20Population%20Based%20Screening%20of%20Common%20NCDs_0.pdf, accessed on June 2, 2024.
- Operational guidelines: Prevention, screening and control of common Non-Communicable Diseases: Hypertension, Diabetes, Common Cancers (oral, Breast, cervical). (Part of comprehensive Primary health Care). Available from: https://mohfw.gov.in/sites/default/files/Operational%20Guidelines%20on%20Prevention%2C%20Screening%20and%20Control%20of%20Common%20NCDs_1.pdf, accessed on June 2, 2024.
- National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases & Stroke (NPCDCS) operational guidelines (revised: 2013-17). Available from: https://mohfw.gov.in/sites/default/files/Operational%20Guidelines%20of%20NPCDCS%20%28Revised%20-%202013-17%29_1.pdf, accessed on June 2, 2024.
- Ayushman Bharat health and wellness centres. Realizing universal health care. Available from: https://nhm.gov.in/infocus/HWCs_Booklet_English_updated_5_April_2022.pdf, accessed on June 2, 2024.
- Operational guidelines: National programme for prevention and control of non-communicable diseases (2023-2030). Available from: https://mohfw.gov.in/sites/default/files/NP-NCD%20Operational%20Guidelines.pdf, accessed on June 2, 2024.
- Assessing national capacity for the prevention and control of noncommunicable diseases: report of the 2019 global survey. Available from: https://www.who.int/publications/i/item/9789240002319, accessed on June 2, 2024.
- WHO list of priority medical devices for management of cardiovascular diseases and diabetes. Available from: https://www.who.int/publications/i/item/9789240027978, accessed on June 2, 2024.
- Service availability and readiness assessment (SARA): an annual monitoring system for service delivery: implementation guide, version 2.2. Available from: https://www.who.int/publications/i/item/WHO-HIS-HSI-2015.5, accessed on February 4, 2025.
- Preparedness of primary and secondary health facilities in India to address major noncommunicable diseases: Results of a national noncommunicable disease monitoring survey (NNMS) BMC Health Serv Res. 2021;21:757.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Assessment of primary care facilities for cardiovascular disease preparedness in Madhya Pradesh, India. BMC Health Serv Res. 2015;15:408.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Preparedness of healthcare facilities of Manipur in the management of noncommunicable diseases: A cross-sectional study. Indian J Public Health. 2022;66:245-50.
- [CrossRef] [PubMed] [Google Scholar]
- Challenges in primary care for diabetes and hypertension: An observational study of the Kolar district in rural India. BMC Health Serv Res. 2019;19:1-11.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- A narrative review of gaps in the provision of integrated care for noncommunicable diseases in India. Public Health Rev. 2020;41:8.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Health system preparedness in noncommunicable diseases: Findings from two states Odisha and Kerala in India. J Family Med Prim Care. 2018;7:565-70.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Managing diabetes mellitus with comorbidities in primary healthcare facilities in urban settings: A qualitative study among physicians in Odisha, India. BMC Fam Pract. 2021;22:99.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- India hypertension control initiative – Hypertension treatment and blood pressure control in a cohort in 24 sentinel site clinics. J Clinical Hypertension. 2021;23:720-9.
- [Google Scholar]
- Preparedness for delivering non-communicable disease services in primary care: Access to medicines for diabetes and hypertension in a district in south India. BMJ Glob Health. 2018;2:e000519.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Rural Health Statistics, 2020-21. Available from: https://mohfw.gov.in/sites/default/files/rhs20-21_2.pdf, accessed on June 2, 2024.
- Preparedness of primary & secondary care health facilities for the management of non-communicable diseases in tribal population across 12 districts in India. Indian J Med Res. 2022;156:260-68.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- ICMR-INDIAB Collaborative Study Group. Metabolic non-communicable disease health report of India: the ICMR-INDIAB national cross-sectional study (ICMR-INDIAB-17) Lancet Diabetes Endocrinol. 2023;11:474-89.
- [CrossRef] [PubMed] [Google Scholar]
- Ayushman Bharat Health and Wellness Centres. Accelerating towards health for all. 2018 - September 2019. Available from: https://nhsrcindia.org/sites/default/files/2021-09/Accelerating%20towards%20health%20for%20all_April_2018-Sept2019.pdf, accessed on June 2, 2024.
- The India hypertension control initiative-early outcomes in 26 districts across five states of India, 2018-2020. J Hum Hypertens. 2023;37:560-7.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Improving the availability of antihypertensive drugs in the India hypertension control initiative, India, 2019-2020. PLoS One. 2023;18:e0295338.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]






