Translate this page into:
Performance of microscopy for detection of microsporidial spores from stool samples of HIV infected individuals with diarrhoea
+For correspondence: Smt. Sangeeta V. Kulkarni, Department of Microbiology & Clinical Pathology, National AIDS Research Institute (ICMR), Pune 411 026, India e-mail: svk51@hotmail.comsvk952000@yahoo.co.in
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
Intestinal microsporidiosis is the most common cause of chronic diarrhoea in treatment-naïve HIV infected patients1. Intestinal microsporidiosis due to Encephalitozoon (Septata) intestinalis and Enterocytozoon bieneusi are also most frequently reported among immunocompromised patients such as transplant recipients2–4. Laboratory diagnosis of microsporidiosis was initially based on the detection of microsporidial spores in stool specimens by light microscopy using special stains5. Electron microscopy, wherever possible, was also used for detection of microsporidia6–8.
Diagnosis of intestinal microsporidiosis has been markedly improved by the use of Weber's chromotrope stain and its modified procedure159, and fluorescence staining with fluorochromes such as Uvitex 2B or calcoflour white which binds to the chitin in the endospore layer of the microsporidial spore181011. Molecular technique such as polymerase chain reaction (PCR) became available later for confirmation of micropsoridia. Additionally, species specific PCR can be used to identify different species of microsporidia12–16. However, due to resource constraints, most laboratories rely on the use of microscopy of stool samples for diagnosis of intestinal microsporidiosis. Limited studies have been carried out in India on detection of microsporidia81718. We compared light microscopy with modified trichome stain, fluorescence microscopy using Uvitex 2B and PCR to detect microsporidia in HIV infected individuals with diarrhoea during January 2009 to May 2010 on consecutive HIV infected patients with diarrhoea admitted at Naidu Municipal Corporation Hospital, Pune. The study protocol was approved by the institutional ethics committee & Naidu Municipal Corporation Hospital.
The study included 331 patients [65 (51 males, 14 females)] HIV infected adults >18 yr and 266 HIV (uninfected individuals) with diarrhoea. This study was carried out only on HIV infected individuals with diarrhoea. Study patients were interviewed using the structured questionnaire. Diarrhoea was defined as two or more liquid or three or more soft stools per day All the patients had history of diarrhoea of <14 days and were treatment-naïve HIV-infected individuals. Stool samples were collected in wide mouth, leak proof, clean sterile containers and then transported to National AIDS Research Institute (NARI) within 4 h of collection. If there was a delay in the transportation, the samples were preserved at 4o C. The samples were immediately processed after receiving at NARI for microscopy by the conventional method8. Stool samples were stained by modified trichome and Uvitex 2B by the method described earlier468, and were subjected to light microscopy and fluorescence microscopy, respectively. A portion of the stool was stored at -70°C for further molecular analysis. DNA was extracted from frozen samples using the QIA amplication DNA tissue kit (Qiagen, Inc, Germany). PCR was performed using specific primers as described by Najla et al19.
The median duration of diarrhoea was found to be 3 days (IQR 2.75 - 5) and median number of episodes of diarrhoea was noted as 6 in HIV-infected individuals (n=65). The mean age was found to be 35.1 yr ranging from 18-60 yr. Male (n=51) outnumbered the females (n=14). The CD4 counts were available only for 35 patients [CD4 count 200-499 cells/μl (n= 29) and CD4 count ≥500 cells /μl (n=6)] Examination of 65 stool samples from 331 patients by light microscopy with modified trichome stain showed microsporidial spores (oval shaped, measuring 1-2 μm in diameter under oil immersion) in four samples. Fluorescence microscopy using Uvitex 2B also showed microsporidial spores in the same four (6.2%) HIV-infected individuals. PCR detected microsporidial spores in stool samples of five (7.7%) individuals including four found positive by light and fluorescent microscopy (Fig.). Of these five samples positive by PCR, three were identified as Enterocytozoon bieneusi and two were identified as Encephalitozoon intestinalis. A repeat light microscopy and fluorescent microscopy on one sample positive only by PCR did not yield positive results. Thus, the results, though limited by a small number of positives, indicate that trichome and Uvitex 2B stains work well for diagnosis of intestinal microsporidiosis. PCR as expected was more sensitive and yielded one additional positive sample.
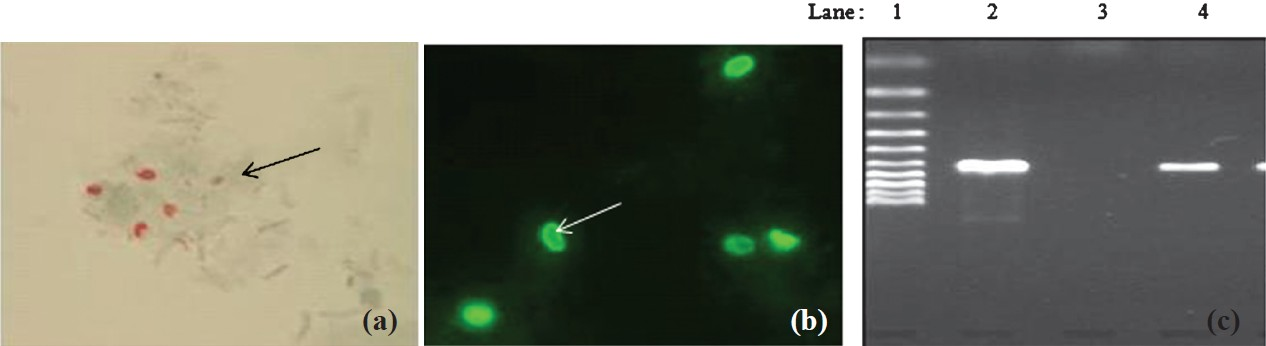
- (a) Stool smear stained with modified trichome stain showing microsporidial spores (arrow); (b) Stool smear stained by Uvitex 2B & examined with UV light. spores of microsporidia show typical elongated shape (arrow); (c) Agaraose gel electrophoresis of PCR product agarose gel electrophoresis of polymerase chain reaction (PCR product. Lane1: Marker 100 bp, Lane 2: positive sample, Lane 3: negative control and Lane 4: positive control).
In conclusion, with well trained laboratory staff both the Uvitex 2B and modified trichome stain can be used for microsporidia detection. PCR can increase sensitivity and species identification. The study was limited by small sample size and small number of positives and hence warrants additional testing on a large number of samples.
Authors thank Naidu hospital staff for providing support for recruitment of patients and collection of samples. Authors also acknowledge the Director, NARI, Pune, for extending support for the study.
References
- Comparison of Chromotrope 2R and Uvitex 2B for the detection of intestinal microsporidial spores in stool specimens of HIV patients attending Nekempte Hospital, West Ethiopia. Ethiop Med J. 2009;47:233-7.
- [Google Scholar]
- Genetic identification of intestinal microsporidia species in immunocompromised patients in Tunisia. Am J Trop Med Hyg. 2009;80:24-7.
- [Google Scholar]
- First cases of microsporidiosis in transplant recipients in Spain and review of the literature. J Clin Microbiol. 2011;49:1301-6.
- [Google Scholar]
- Disseminated infection with a new genovar of Encephalitozoon cuniculi in a renal transplant recipient. J Clin Microbiol. 2010;48:2651-3.
- [Google Scholar]
- Intestinal microsporidiosis in diarrheal patients infected with human immunodeficiency virus-1 in Addis Ababa Ethiopia. Jpn J Infect Dis. 2006;59:306-10.
- [Google Scholar]
- Detection and species identification of microsporidial infections using SYBR Green real-time PCR. J Med Microbiol. 2011;60:459-66.
- [Google Scholar]
- Morphological, molecular, and phylogenetic characterization of Nosema ceranae, a microsporidian parasite isolated from the European honey bee, Apis mellifera. J Eukaryot Microbiol. 2009;56:142-7.
- [Google Scholar]
- Electron microscopy identification of microdporidia (Enterocytozoon bieneusi) and Cyclospora cayentanesis from stool samples of HIV infected patients. Indian J Med Microbiol. 2004;22:119-22.
- [Google Scholar]
- Identification of Enterocytozoon bieneusi by PCR in stools of Tunisian immunocompromised patients. Pathol Biol (Paris). 2011;59:234-9.
- [Google Scholar]
- Detection of intestinal microsporidiosis in diarrhoeal patients infected with the human immunodeficiency virus (HIV-1) using PCR and Uvitex-2B stain. Ethiop Med J. 2005;43:97-101.
- [Google Scholar]
- Emerging microsporidian infections in Russian HIV-infected patients. J Clin Microbiol. 2011;49:2102-8.
- [Google Scholar]
- Molecular study of microsporidiosis due to Enterocytozoon bieneusi and Encephalitozoon intestinalis among human immunodeficiency virus-infected patients from two geographical areas : Niamey, Niger and Hanoi, Vietnam. J Clin Microbiol. 2007;45:2999-3002.
- [Google Scholar]
- Detection of microsporidia in local HIV-positive population in Malaysia. Trans R Soc Trop Med Hyg. 2011;105:409-13.
- [Google Scholar]
- Microsporidiosis in south Africa: PCR detection in stool samples of HIV positive and HIV-negative individuals and school children in Vhembe district, Limpopo Province. Trans R Soc Trop Med Hyg. 2007;101:547-54.
- [Google Scholar]
- Presence of Enterocytozoon bieneusi associated with intestinal coccidia in patients with chronic diarrhea visiting an HIV center in Haiti. Am J Trop Med Hyg. 2008;79:579-80.
- [Google Scholar]
- PCR for the diagnosis and species identification of microsporidia in patients with keratitis. Clin Microbiol Infect. 2011;17:476-8.
- [Google Scholar]
- Enteric opportunistic parasites among HIV infected individuals: associated risk factors and immune status. Jpn J Infect Dis. 2007;60:76-81.
- [Google Scholar]
- Genetic identification of intestinal microsporidia species in immunocompromised patients in Tunisia. Am J Med Hyg. 2009;80:24-7.
- [Google Scholar]





