Translate this page into:
Perception towards electronic health records & uptake of digital health IDs among the urban residents in northern India: A mixed methods study
For correspondence: Dr Kathirvel Soundappan, Department of Community Medicine and School of Public Health, Postgraduate Institute of Medical Education and Research, Chandigarh 160 012, India e-mail: selvkathir@gmail.com
-
Received: ,
Abstract
Background & objectives
Ayushman Bharat Digital Mission (ABDM) envisages a unique digital health ID for all citizens of India, to create electronic health records (EHR) of individuals. The present study assessed the uptake of Digital Health IDs by the patient and general population, their attitude toward EHR, and explored the barriers to digital ID and utilizing electronic health records services.
Methods
A concurrent explanatory mixed methods study was undertaken in Chandigarh, India, with an analytical cross-sectional design as a quantitative part and a qualitative descriptive study. The study participants were 419 individuals aged ≥18 yr who attended the urban primary healthcare centre (n=399) and the community-based screening camps (n=20) between July 2021 and January 2022. Latent Class Analysis (LCA) was undertaken to identify hidden sub-population characteristics. In-depth interviews were done to identify the barriers to health ID uptake.
Results
The digital health ID uptake rate was 78 per cent (n=327). Among the study participants, those who were aware of EHR, those who wanted a national EHR system, those who were confident with the government on EHR security, and those who were willing to make national EHR accessible for research showed significantly higher digital health ID uptake than their counterparts. The themes identified under barriers of uptake from the qualitative interviews were lack of awareness, technology-related (including digital literacy) and utility-related.
Interpretation & conclusions
Increasing EHR awareness, digital health literacy, and enacting data protection laws may improve the acceptance of the digital health ecosystem in India.
Keywords
Electronic health records
health ID
India
latent class analysis
medical records
mixed methods study
As envisaged under the (Indian) National Health Policy 2017 as well as the National Digital Health Blueprint1,2, the Government of India launched the National Digital Health Mission (NDHM) on August 15, 2020 (renamed as Ayushman Bharat Digital Mission (ABDM) on September 27, 2021).3 The mission aims to create a unique digital health ID (ABHA- Ayushman Bharat Health Account) for all citizens of India and to create Electronic Health Records (EHRs) of patients so that these can be accessed anywhere across the country.EHR is an electronic version of an individual’s medical history that is maintained by the provider over time and may include all of the key clinical data relevant to that particular individual’s care under a particular provider, including demographics, progress notes, problems, medications and adherence, vital signs, past medical history, immunizations, laboratory data, radiology reports and other clinical data4.
Countries around the world have adopted EHR at multiple levels with varied outcomes. While Singapore successfully incorporated the EHR into their healthcare system, England reported difficulties in achieving similar success5. Continuous engagement of the medical professionals, one of the major end user stakeholders of EHR, right from the planning stage through the implementation, enabling ownership feel and involving doctors with information technology (IT) knowledge in critical roles of the EHR initiative contributed towards the success of the programme in Singapore. The size of the organization/country also plays a role in the effective implementation of the EHR programme5. For instance, a centralized push for EHR in an overall health system with a decentralized approach, influential stakeholders against the government’s EHR push, lack of committed IT partners owing to punitive contracts are a few reasons for the adverse outcomes in England5,6.
EHR usage for individual patients in India has been restricted to specific diseases7. Health facilities and patient groups such as people living with HIV/AIDS (PLHA) and Nikshay for tuberculosis patients under the vertical health programmes8. Though Electronic Medical Records (EMRs) have been used by multiple hospitals in India9-12, these remain confined within a particular hospital. Qualitative analysis of the issues faced by health workers in EMR settings has been explored13. Haryana, a State in India, introduced an EHR service under eUpchar ( https://eupchaarharyana.org.in/eupchaar/eupchaar/home) in 2015, linking certain public health facilities, wherein patients were provided unique identification numbers and their records could be accessed and updated among those facilities. However, the system has not been evaluated for portability and patient perception towards accessing and utilizing the services under the system14.
The introduction of digital health ID and EHR at the population level is new in India. Studies are available on population-based EHR ventures wherein centralized databases and data sharing between various healthcare facilities are enabled. However, literature on the people’s perception and uptake of EHR are not available in India. Such studies will provide public involvement in the EHR building process from the primary care level and inform the healthcare providers and programme managers about a patient-centred, acceptable, user-friendly development of EHRs in India.
In the first year of the NDHM (2020-21), the scheme was piloted in the country’s Union Territories (UTs)3. Chandigarh, being a UT, was a part of the project. Hence, the present study was conducted to assess the perception of the adults towards EHR and the uptake of digital health ID in Chandigarh.
Material & Methods
This study was undertaken at the department of Community Medicine and School of Public Health, Postgraduate Institute of Medical Education and Research (PGIMER), Chandigarh, India, after obtaining clearance from the Institutional Ethics Committee of PGIMER, Chandigarh. Verbal informed consent was taken from all participants before administering the questionnaire. The interviews were undertaken in person. Audio consent was taken considering the COVID-19 pandemic situation at that time since the investigators wanted to minimize physical contact in context to a written consent form. The consent was recorded using a voice recorder after the participants read and/or were informed about the study.
The present study was a concurrent mixed method investigation. A cross-sectional design was adopted for the quantitative component and in-depth interviews (IDIs) for the qualitative part were conducted. The study participants were the adults visiting the routine outpatient department (OPD) and the community-based screening camps conducted in the coverage area of a primary health centre (PHC; field practice of the department) in Chandigarh. Adults who did not have Chandigarh-based Aadhar numbers and those who had already completed the study during their previous encounters were excluded. A PHC from Chandigarh was chosen because the study was undertaken during the piloting phase of the ABDM (2020-21), in which the government of India was only implementing it in the Union Territories (UT). This specific PHC area was chosen as per the memorandum of understanding with the UT health authorities, where the department can undertake research, provide healthcare services and implement national health programmes. The study was conducted from July 2021 to January 2022. Assuming a digital health ID uptake of 50 per cent among the eligible community, with an absolute error of five per cent and 95 per cent confidence levels, we calculated a minimum sample size of 400. Adding 10 per cent for the non-response rate, a sample size of 440 was required. The sampling technique was consecutive sampling of consenting eligible adults. In order to improve the representativeness, we kept a limit of ten participants per day in the OPD and ten participants per outreach camp to be enrolled in the study. It was done to ensure people availing different healthcare services (curative and preventive) at specific clinics (e.g., NCD clinics, antenatal clinics, immunization clinics) and camps (community-based NCD screening camps) on different days during the data collection period were included. Purposive sampling of individuals who wilfully declined (10 participants) to join ABDM by refusing to create health IDs was done to conduct the in-depth interviews. The total number of interviews was decided based on the saturation of information (Principle of redundancy).
Study procedure
A trilingual (English, Hindi and Punjabi), semi-structured, tailored questionnaire was administered to the eligible participants to assess the socio-demography and access levels of EHR by a trained healthcare worker. This questionnaire was a modified version of the National Health System (NHS) tool used to gauge the patient as well as public perception towards EHRs and the purpose of EHR use in London, United Kingdom (UK)15. The items about the attitude of the people towards EHRs in the UK study were included in the present study since those items (e.g., access to EHR data, security of the EHR, etc.) were also relevant in the current context. The questionnaire was modified to fit the Indian settings and was pre-tested among 10 participants. In addition, items specific to the ABDM (erstwhile NDHM), people’s usual medical record storage practices and demographic profiles were also included in the questionnaire. An interview guide was formulated for conducting the in-depth interviews, and these were conducted by the investigators of the study (trained in qualitative research). In-depth interviews were conducted at a place and time convenient for the participants. All the consenting participants in the IDI agreed to participate and complete the interviews on the same day in the PHC/camp itself. A special consent was obtained for audio recording of the interview. Verbatim was obtained in Hindi and translated into English.
Statistical analysis
Quantitative data was captured in Epicollect5 and analyzed with STATA® software (version 17, STATA Corp.). The uptake of digital health ID is presented in number and proportion. The digital health ID uptake rate was computed as the proportion of persons who accepted and created digital health IDs among the ones who participated in the study. The association between sociodemographic factors and uptake of digital ID was assessed using univariate analysis (Chi-square test or Fisher’s exact test). In order to identify any hidden sub-population characteristics as a potential predictor of digital health ID uptake, latent class analysis (LCA) was conducted16.We included all variables to create three latent classes by running 50 iterations with a random start until a group of variables converged and the model was estimated. A P value of <0.05 was considered as significant. A thematic analysis of the qualitative data was done to identify and analyze the participants’ attitudes towards EHR and barriers to participating in ABDM. Audio-recorded interviews and field notes were transcribed and translated to English on the same day by the investigators, and manual content analysis was done to generate codes and themes, which were verified. Any discrepancy between the two investigators was resolved by consensus achieved through discussion.
Results
Sociodemography
The total number of participants in the study was 419, with a completion rate of 95.2 per cent. Among the study participants, 399 were adults visiting the PHC (265 were adults who availed healthcare services, and 134 were the accompanying persons), and 20 were from the two community-based NCD screening camps conducted in the study area during the data collection period. Of these, 224 (53.5%) were male, 164 (39.1%) belonged to the 18-44 yr age group, 139 (33.2%) were working, and 221 (52.7%) had a pre-existing disease condition (Table I).
| Variables | Total (n=419) | Made digital health ID (n=327), n (%) | Did not make digital health ID (n=92), n (%) |
|---|---|---|---|
| Sex | |||
| Male | 224 | 173 (77.2) | 51 (22.8) |
| Female | 195 | 154 (79) | 41 (21) |
| Age group (yr) | |||
| 18-44 | 164 | 120 (73.2) | 44 (26.8) |
| 45-59 | 97 | 80 (82.5) | 17 (17.5) |
| ≥60 | 158 | 127 (80.4) | 31 (19.6) |
| Occupation | |||
| Employed | 139 | 108 (77.7) | 31 (22.3) |
| Retired | 133 | 111 (83.5) | 22 (16.5) |
| Homemaker | 106 | 80 (75.5) | 26 (24.5) |
| Student | 41 | 28 (68.3) | 13 (31.7) |
| Presence of pre-existing disease | |||
| No | 198 | 150 (75.8) | 48 (24.2) |
| Yes | 221 | 177 (80.1) | 44 (19.9) |
| Hypertension | 119 | 94 (79) | 25 (21) |
| Diabetes | 93 | 78 (83.9) | 15 (16.1) |
| Musculoskeletal disorders | 22 | 16 (72.7) | 6 (27.3) |
| Thyroid disorder | 18 | 16 (88.9) | 2 (11.1) |
| CAD | 12 | 11 (91.7) | 1 (8.3) |
| Asthma | 9 | 8 (88.9) | 1 (11.1) |
| Skin disorders | 5 | 5 (100) | 0 (0) |
| Stroke | 4 | 3 (75) | 1 (25) |
| Others# | 12 | 9 (75) | 3 (25) |
None of the variables were found to have P <0.05. CAD, coronary artery disease; MSD, musculoskeletal disorders. #Others category: Psychiatric disorders (n=5), Past surgery (n=5), Cancer (n=3), Anaemia (n=1), Cataract (n=1)
Digital Health ID uptake
The uptake rate of digital health IDs was 78 per cent (n=327). Among those who did not create health IDs (n=92), 66.3 per cent (n=61) were not willing, 27.2 per cent (n=25) did not have either a mobile or Aadhar number available with them, 2.2 per cent (n=2) did not link their mobile with Aadhar, while one respondent said he did not have time and another said he had no idea about the health ID and hence will not make it.
Awareness and attitude towards HER
The awareness rate of EHR among the study participants was 28.2 per cent (n=118). Media (n=66, 55.9%), followed by healthcare workers (HCWs; n=47, 39.8%), the internet (n=33, 28%), and the Health Ministry website (n=14, 11.8%) were the major sources of information on EHR. Doctors (87.1%) followed by pharmacists (57%) were the HCWs to whom the participants were willing to give complete access to their health records with identifiers. The majority of the participants did not want to share their health records, even without personal identifiers, with drug companies (61.1%) and health charities (52.5%) (Table II).
| Variable | Frequency | Percentage |
|---|---|---|
| Heard about EHR | 118 | 28.2 |
| Heard about ABDM | 149 | 35.6 |
| Access level of health records with name & address to doctors | ||
| Complete access | 365 | 87.1 |
| Partial access | 16 | 3.8 |
| No access | 38 | 9.1 |
| Access level of health records with name & address to pharmacist | ||
| Complete | 239 | 57 |
| Partial | 21 | 5 |
| No | 159 | 38 |
| Access level of health records with name & address to registration staff | ||
| Complete | 194 | 46.3 |
| Partial | 19 | 4.5 |
| No | 206 | 49.2 |
| Access level of health records with name & address to ambulance staffs | ||
| Complete | 200 | 47.7 |
| Partial | 26 | 6.2 |
| No | 193 | 46.1 |
| Access level of health records with name & address to other HCWs | ||
| Complete | 170 | 40.6 |
| Partial | 20 | 4.8 |
| No | 229 | 54.6 |
| Access level of health records to ABDM researchers | ||
| Complete access with name & address | 269 | 64.2 |
| Complete access without name & address | 28 | 6.7 |
| No access with or without name & address | 122 | 29.1 |
| Access level of health records to academic researchers | ||
| Complete access with name & address | 238 | 56.8 |
| Complete access without name & address | 31 | 7.4 |
| No access with or without name & address | 150 | 35.8 |
| Access level of health records to health charities | ||
| Complete access with name & address | 172 | 41.1 |
| Complete access without name & address | 27 | 6.4 |
| No access with or without name & address | 220 | 52.5 |
| Access level of health records to drug companies | ||
| Complete access with name & address | 137 | 32.7 |
| Complete access without name & address | 26 | 6.2 |
| No access with or without name & address | 256 | 61.1 |
ABDM, Ayushman Bharat digital mission; EHR, electronic health records; HCW, healthcare workers
Current health record practices
The health record practices of the participants did not have a significant association with digital health ID uptake (Table III).
| Health record practices | Total (n=419) | Made digital health ID, n (%) | Did not make digital health ID, n (%) |
|---|---|---|---|
| Record Maintenance | |||
| Do not maintain | 1 | 1 (100) | 0 (0) |
| Paper based | 413 | 324 (78.5) | 89 (21.5) |
| Scanned pictures in mobile phone | 137 | 107 (78.1) | 30 (21.9) |
| Scanned pictures in computer | 21 | 18 (85.7) | 3 (14.3) |
| Lost medical records | |||
| Yes | 96 | 77 (80.2) | 19 (19.8) |
| No | 255 | 194 (76.1) | 61 (23.9) |
| Don’t know | 68 | 56 (82.4) | 12 (17.6) |
| Health service use in last 6 months* | |||
| Yes | 399 | 315 (78.9) | 84 (21.1) |
| No | 20 | 12 (60) | 8 (40) |
| Forgot medical records | |||
| Yes | 57 | 42 (73.7) | 15 (26.3) |
| No | 338 | 264 (78.1) | 74 (21.9) |
| May be | 23 | 20 (87) | 3 (13) |
| Forgotten frequency | |||
| All the time | 1 | 1 (100) | 0 (0) |
| Most of the time | 13 | 10 (76.9) | 3 (23.1) |
| Sometimes | 66 | 51 (77.3) | 15 (22.7) |
| Doctors asked for old record | |||
| Yes | 308 | 241 (78.2) | 67 (21.8) |
| No | 104 | 81 (77.9) | 23 (22.1) |
| May be | 6 | 4 (66.7) | 2 (33.3) |
| Able to provide records | |||
| Yes | 364 | 284 (78) | 80 (22) |
| No | 46 | 36 (78.3) | 10 (21.7) |
| May be | 8 | 6 (75) | 2 (25) |
P*<0.05
Determinants of health ID uptake
Awareness of EHR and willingness to make their health records (complete or partial) a part of the national EHR ecosystem for personal use as well as for health services planning, policy and research were significantly associated with higher uptake of digital health ID. The confidence of the participants in the government’s ability to make EHR secure also had a significant effect on the digital health ID uptake. Overall, 83.7 per cent (n=262) of participants favoured building a national EHR system (Table IV).
| Variables | Total (n=419) | Made digital health ID, n (%) | Did not make digital health ID, n (%) |
|---|---|---|---|
| Heard of EHR* | |||
| Yes | 118 | 101 (85.6) | 17 (14.4) |
| No | 301 | 226 (75.1) | 75 (24.9) |
| Heard of ABDM | |||
| Yes | 149 | 124 (83.2) | 25 (16.8) |
| No | 270 | 203 (75.2) | 67 (24.8) |
| Records be a part of National EHR* | |||
| Yes, complete records | 214 | 172 (80.4) | 42 (19.6) |
| Yes, partial records | 144 | 122 (84.7) | 22 (15.3) |
| No | 60 | 32 (53.3) | 28 (46.7) |
| Records be a part of National EHR for health services planning & policy* | |||
| Yes with name & address | 189 | 152 (80.4) | 37 (19.6) |
| Yes without name & address | 163 | 131 (80.4) | 32 (19.6) |
| No | 67 | 44 (65.7) | 23 (34.3) |
| Records be a part of National EHR for research* | |||
| Yes with name & address | 172 | 138 (80.2) | 34 (19.8) |
| Yes without name & address | 168 | 138 (82.1) | 30 (17.9) |
| No | 79 | 51 (64.6) | 28 (35.4) |
| Worry about security of records under National EHR | |||
| Yes | 251 | 194 (77.3) | 57 (22.7) |
| No | 168 | 133 (79.2) | 35 (20.8) |
| Govt able to make EHR secure* | |||
| Yes | 369 | 298 (80.8) | 71 (19.2) |
| No | 49 | 29 (59.2) | 20 (40.8) |
| Security of EHR compared to current method | |||
| Less secure | 62 | 44 (71) | 18 (29) |
| Equally secure | 135 | 100 (74.1) | 35 (25.9) |
| More Secure | 221 | 183 (82.8) | 38 (17.2) |
| Possible risks to National EHR security | |||
| Low | 257 | 206 (80.2) | 51 (19.8) |
| Moderate | 122 | 91 (74.6) | 31 (25.4) |
| High | 40 | 30 (75) | 10 (25) |
| Favour of development of National EHR* | |||
| Yes | 313 | 262 (83.7) | 51 (16.3) |
| No | 21 | 13 (61.9) | 8 (38.1) |
| Undecided | 85 | 52 (61.2) | 33 (38.8) |
P* <0.05. Govt, government
Latent class analysis
Three sub-groups (latent classes- LC) were identified by the LCA after testing various combinations of variables within the study population based on the following variables: EHR awareness, ABDM awareness, willingness to make their EHR part of the national EHR system for self-use, for policy-making or planning, for research use, feel that EHR is secure, overall in favour of EHR and allow doctors to access their EHR. The probability of each variable belonging to LCs is depicted in Figure 1 as proportions. The latent class 1 group of participants who had the least probability of being aware of EHR and ABDM were not willing to share their health records in EHR for policy and research and were not in favour of EHR creation for India. Latent class 2 characteristics included those equally unaware of EHR and ABDM, similar to latent class 1 but who were willing to allow EHR for self-use, policy, and research, felt secure about EHR in India, overall in favour of EHR and willing to allow the doctors to access complete records from their EHR. Latent class 3 characteristics included being well aware of EHR and ABDM, and also willing to allow EHR for self-use, policy, and research, feeling secure about EHR in India, overall in favour of EHR and willing to allow the doctors to access their EHR. A total of 77 (18.4%), 229 (54.6%) and 113 (27%) were classified under latent classes 1, 2 and 3, respectively. Compared to latent class group 1, group 2 [Prevalence Ratio (PR): 3.15; 95% Confidence interval (CI): 1.8-5.51] and group 3 (PR: 4.9; 95% CI: 2.42-9.93) had significantly higher uptake of digital health ID, while no significant difference between LC 2 and 3 was noted. Thus, LCA denotes that a favourable attitude towards the applications and security of the EHR ecosystem may lead to better uptake of digital health IDs and, subsequently, participation in the national EHR.
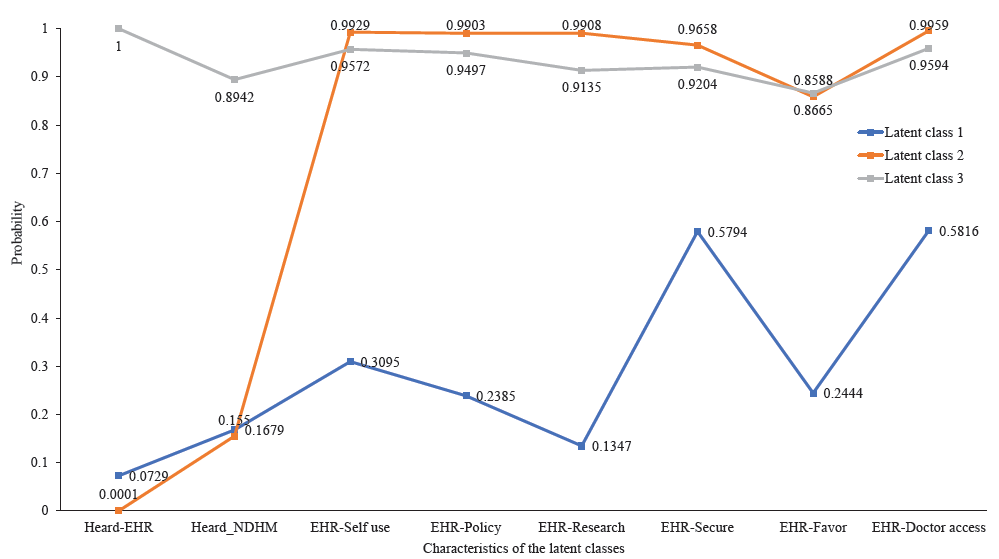
- Margin plot of the three latent class created in the study. EHR, electronic health records; NDHM, National Digital Health Mission.
Barriers to digital health ID uptake
The qualitative analysis of in-depth interviews revealed a lack of awareness, apprehension towards the digital technology and perceived limited utility as the major themes for barriers to the uptake of digital health IDs (Fig. 2). A few verbatim of the non-acceptors of the digital health ID under the above themes are provided in the Box.
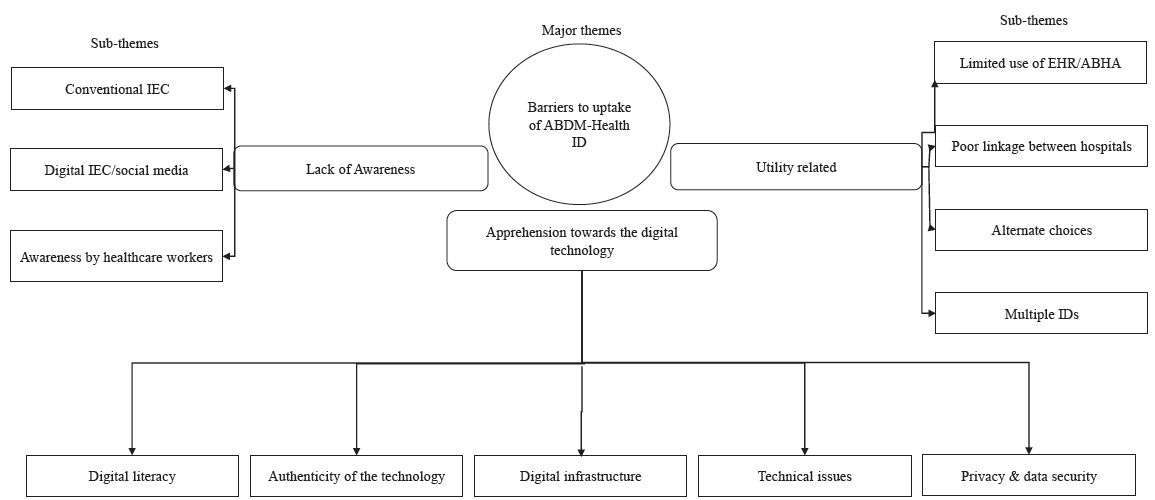
- Thematic analysis of the ‘barriers to uptake of ABDM-Health ID’. ABHA, Ayushman Bharat Health Account; IEC, Information, Education and Communication.
Discussion
The digital health ID uptake rate was 78 per cent among the participants from Chandigarh. As of December 2023, 50.39 crores of ABHAs have been created across India.17 Chandigarh reported an ABHA coverage rate of 55 per cent. Among the larger States, Andhra Pradesh reported coverage of 77.6 per cent, the highest in the country17. The differential finding may be due to the period of this study. It was conducted during the pilot phase of the ABDM; thus, administrative focus and impetus were there on this specific programme, which might have plateau over time. The higher proportion of digital health ID uptake (80.4%) among the elderly population (>60 yr) underlines the role played by healthcare workers in assisting and enabling the elderly to create digital health IDs. The role of families and young individuals in enabling older individuals to access and avail the digital health services has also been explored to be useful in previous studies18,19. Hence, it would be prudent to include the family members of the elderly within the target population for creating awareness about digital health IDs and EHRs.
Awareness regarding the EHR was low among the participants approaching the PHC in this study which was a significant determinant of digital health ID uptake. Furthermore, the media was found to be the major source of awareness for the participants who had heard about EHR. Qualitatively, awareness (rather a lack of it) about EHR was identified as a major barrier to digital health ID uptake, with refusers quoting the lack of communication through mass media. The same was observed in univariable analysis and the LC. Social media was seen as a reliable source by certain refusers as they had the option to read both the pros and cons from social media. These findings suggest that awareness of the EHR is essential, and multiple channels of communication should be used.
The security of health records in the EHR system was a major concern expressed in this study. A study from the UK20 reported that 47 per cent of the people felt that EHR is less secure than the conventional method of health records storage. The confidence in the government’s ability to keep the EHR secure significantly impacted the digital health ID uptake in this study. Reduced confidence in government entities to ensure the safety of EHR data has also been expressed in UK20. In the USA, over a period of time, participants showed a decreasing trend in privacy and security concerns regarding EHR usage21.
Apprehensions towards technology usage, trust in technology, inexperience, lack of digital literacy and privacy concerns were found to be barriers to adopting EHRs. Digital health literacy has been reported to be low in India (20%)22, and there is a lack of studies on this topic. Perceived lack of utility for digital health IDs and EHRs by the participants is another barrier, as it does not provide any incentives or motivation. The government of India is introducing an incentive scheme for healthcare institutes to create and link health records digitally under the ABDM from 2023 to improve EHR usage23. In a study conducted on EMR in Chandigarh, participants reported a positive attitude towards the digitized settings as it had reduced their time in giving the previous history24. Avoidance of repetition of examination and history taking was also reported as a potential positive factor for EHR acceptance in the UK20.
The present study participants were willing to give doctors and pharmacists complete access to their health records, with identifiers, similar to the findings of a previous study from Korea25. Most of our study participants were accommodative to share their health records with the researchers, while the majority refused to give access to any records to the drug companies. Similarly, research-related EHR access was accepted by a majority in the UK (81.38%). Refusing access to drug companies could be due to its potential for breach of privacy and associated commercial exploitation20.
In our study settings, 74.7 per cent of the participants were in favour of setting up a national EHR, while in the UK, a slightly lower proportion was supportive of such an initiative (62.47 and 55%, respectively)15,20. Allowing individuals to access their own digitalized health records has been reported as a potential benefit of the EHR26, as well as improving patient-centred care27. This could be explored in India’s digital health architecture.
The present study is the first to assess the patient and public perception towards EHRs in India in a programmatic setting. The mixed methods design has helped to identify and triangulate the major barriers to health ID uptake and EHR reluctance. Though the cross-sectional study design limits the temporality of association between the potential determinants identified, creation of the digital ID is a one-time event, and all participants who had accepted and created the digital health ID did so during the time of the data collection after enrolling in this study. Hence, the data which we collected under the variable regarding awareness of EHR was for the period prior to the creation of the digital health IDs. Hence, this may not be considered a limitation in the context of the current study. However, this limitation is applicable to EHR practices carried out by the participants. Limited generalizability of the findings to other Indian States, since the study was undertaken among people from a single PHC area, is another limitation. This was because the study was undertaken during the piloting phase of the ABDM (2020-21), in which the Government of India was implementing it in the UTs only. There is also potential selection bias since it was not a household-based study following probability sampling but rather undertaken majorly among those adults approaching an urban PHC. Although the authors modified and pre-tested the NHS-EHR tool in the current settings, it was not validated in India, which is another limitation. We applied LCA to identify the hidden population group characteristics that enabled the digital health ID uptake. However, the following limitations of the LCA apply to the current study as well: (a) reification, which indicates that some or all the identified sub-groups of the population by the LCA may not always exist in actual settings28,29; (b)class assignment is not infallible30; and (c) unknown impact of the study sample size on the latent classes29. ‘Naming fallacy’ can also occur in LCA when the classes are specifically named, while it does not accurately describe the classes30.
In conclusion, EHR awareness is a major determinant for the uptake of digital health IDs among urban residents of Chandigarh. Overall, a favourable attitude towards the applications and security of the EHR ecosystem among the public will lead to better uptake of digital health IDs and may increase participation in the national EHR. Campaigns in mass media and social media, as well as legal provisions addressing the above concerns, need to be conducted. Furthermore multi-centric studies involving various States of India must be undertaken to improve the generalizability of the current findings and to identify further context-specific determinants in those States. Nationally representative, serial cross-sectional surveys must be conducted to understand the pattern and trends of perception among the people as the EHR is rolled out and expanded in Indian settings. Digital health literacy and incentivization of EHR for its adoption need to be studied in the Indian context, which may impact the EHR ecosystem in the long run.
Acknowledgment
Authors acknowledge the healthcare workers who assisted in the data collection and rolling out the ABDM.
Financial support & sponsorship
This research was funded by the IJCM-Ford Foundation Grant 2021 (01/2021).
Conflicts of Interest
None.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing of the manuscript and no images were manipulated using AI.
References
- National Health Policy 2017. Available from: https://mohfw.gov.in/sites/default/files/9147562941489753121.pdf, accessed on November 28, 2020.
- Final Report on National Digital Health Blueprint (NDHB). Available from: https://mohfw.gov.in/?q=reports, accessed on November 28, 2020.
- Update on Ayushman Bharat Digital Mission. Available from: https://pib.gov.in/PressReleaseIframePage.aspx?PRID=1813660, accessed on September 19, 2024.
- Electronic Health Records. Available from: https://www.cms.gov/Medicare/E-Health/EHealthRecords, accessed on November 16, 2020.
- The dynamics of institutional pressures and stakeholder behavior in national electronic health record implementations: a tale of two countries. J Inf Technol. 2019;34:292-332.
- [Google Scholar]
- Implementation and adoption of nationwide electronic health records in secondary care in England: Final qualitative results from prospective national evaluation in “early adopter” hospitals. BMJ. 2011;343:d6054.
- [Google Scholar]
- Electronic health records and outpatient cardiovascular disease care delivery: Insights from the American college of cardiology’s PINNACLE India quality improvement program (PIQIP) Indian Heart J. 2018;70:750-52.
- [Google Scholar]
- National Tuberculosis Elimination Program. Available from: https://nikshay.in/Home/AboutUs, accessed on November 27, 2020.
- Assessing the implementation of a mobile App-based electronic health record: A mixed-method study from South India. J Educ Health Promot. 2020;9:102.
- [Google Scholar]
- Electronic health record use in an affluent region in India: Findings from a survey of Chandigarh hospitals. Int J Med Inform. 2017;103:78-82.
- [Google Scholar]
- Adoption of electronic health records: A roadmap for India. Healthc Inform Res. 2016;22:261-9.
- [Google Scholar]
- C-DAC EHR/EMR Systems. Available from: https://www.cdac.in/index.aspx?id=hi_ehr_ehr_emr_systems, accessed on November 28, 2020.
- A case study of an EMR system at a large hospital in India: Challenges and strategies for successful adoption. J Biomed Inform. 2011;44:958-67.
- [Google Scholar]
- Implementing e–Upchaar: Hospital management information system for public health facilities in Haryana. Electron physician. 2020;12:7694-702.
- [Google Scholar]
- Patient and public views on electronic health records and their uses in the United Kingdom: Cross-sectional survey. J Med Internet Res. 2013;15:e160.
- [Google Scholar]
- Practitioner’s guide to latent class analysis: methodological considerations and common pitfalls. Crit Care Med. 2021;49:e63.
- [Google Scholar]
- ABDM Insight. Available from: https://dashboard.abdm.gov.in/abdm/, accessed on December 28, 2023.
- Obstacles to using online health services among adults age 50 and up and the role of family support in overcoming them. Isr J Health Policy Res. 2020;9:42.
- [Google Scholar]
- Digital health platforms for the elderly? Key adoption and usage barriers and ways to address them. Technol Forecast Soc Change. 2023;189:122319.
- [Google Scholar]
- Patient and public views about the security and privacy of electronic health records (EHRs) in the UK: results from a mixed methods study. BMC Med Inform Decis Mak. 2015;15:1-15.
- [Google Scholar]
- Trends in public perceptions of electronic health records during early years of meaningful use. Am J Manag Care. 2015;21:e487.
- [Google Scholar]
- Digital health literacy among the ageing population: A comparative cross-sectional study between rural and urban Telangana, India. Med J Armed Forces India. 2024;80:313-19.
- [Google Scholar]
- Ayushman Bharat Digital Mission. Available from: https://abdm.gov.in/DHIS, accessed on December 30, 2022.
- Stakeholders’ perceptions of the implementation of a patient-centric digital health application for primary healthcare in India. Healthc Inform Res. 2021;27:315-24.
- [Google Scholar]
- Individual willingness to share personal health information with secondary information users in South Korea. Health Commun. 2020;35:659-66.
- [Google Scholar]
- Exploring patients’ perceptions of accessing electronic health records: Innovation in healthcare. Health Informatics J. 2017;25:203-15.
- [Google Scholar]
- How the use of a patient-accessible health record contributes to patient-centered care: Scoping review. J Med Internet Res. 2021;23:e17655.
- [Google Scholar]
- Latent class analysis and latent profile analysis. In: Jason LA, Glenwick DS, eds. Handbook of methodological approaches to community-based research: Qualitative, quantitative, and mixed methods. New York, US: Oxford University Press; 2016. p. :143-51.
- [Google Scholar]
- Latent class analysis: An alternative perspective on subgroup analysis in prevention and treatment. Prev Sci. 2013;14:157-68.
- [Google Scholar]






