Translate this page into:
Pattern of paediatric HIV status disclosure in coastal Karnataka
For correspondence: Dr Nishanth Krishna K, Department of Community Medicine, Father Muller Medical College, Father Muller Road, Kankanady, Mangaluru 575 002, Dakshina Kannada District, Karnataka, India e-mail: nishukrishna@hotmail.com
-
Received: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Karnataka is a high HIV prevalent State in India. Although benefits have been shown by disclosing the HIV status to the child, information regarding HIV status disclosure in Karnataka is limited. Hence, this study was conducted to estimate the proportion of children who had been disclosed of their HIV status and its pattern among those who visited the district antiretroviral therapy (ART) centre in coastal Karnataka.
Methods:
A cross-sectional study was conducted in an ART centre in a district hospital in coastal Karnataka between October 2014 and July 2015. Caregivers of paediatric HIV patients were approached and willing participants were administered a pre-formed, pre-tested semi-structured questionnaire developed for the study.
Results:
A total of 185 caregivers of the HIV-positive children were interviewed. Mean age of the children was 11±4 years. Only 107 (57.8%) children were aware of their HIV status. Of these, 95 were disclosed fully. Counsellors in rehabilitation centres were the most probable person to disclose and planned events. Children were told of their HIV status for their knowledge and were more likely to be disclosed if they were around 11-15 yr of age and staying in rehabilitation centres.
Interpretation & conclusions:
Older children were more likely to be disclosed of their HIV status by counsellors. Steps need to be taken to counsel and encourage caregivers to fully disclose the HIV status to the children at least when they attain the age more than 11 years.
Keywords
Disclosure pattern
HIV disclosure
HIV/AIDS
paediatric disclosure
paediatric HIV
According to UNAIDS, India has the third highest burden of HIV globally1. It is also one among the 22 ‘priority countries’ where the process of elimination of HIV is being hastened among the children aged less than 15 years1. In India, as per the estimates for 2015 children under 15 yr of age, it accounted for around 1.38 lakhs of all the HIV-infected individuals2. In November 2014, in Karnataka, a high HIV prevalent State of India, the estimated number of children living with HIV/AIDS (CLHIV) was 14,1953.
CLHIV are considered as ‘the missing faces of AIDS’4. Due to improvements in diagnosis and treatment, infants and young children with HIV are surviving into adolescence5. Without being told formally, some children may wonder about the reasons for their medicines and doctor visit. Children whose status is disclosed to them after puberty may have already engaged in risky behaviours6.
Systematic reviews highlighted that the proportion of children in resource-limited settings who were disclosed about their HIV status was generally found to be low78. The characteristics of child considered important for disclosure included the child's age, gender, education level, medication responsibilities, whether the children asked questions and their perceived ability to understand their diagnosis78. Older age, child's clinical status, whether receiving anti-retroviral therapy (ART), longer duration of enrolment in an ART clinic and lower CD4 count in a child were associated with higher chances of disclosure78. Furthermore, caregivers with a higher education, those who were more open about their own status, who were not the father of the child and with financial problems were more likely to disclose the HIV status to their child. Caregiver's beliefs about their child's ability to understand also influenced disclosure. Benefits such as improved medication adherence, less frustration in the child and caregiver, positive effects following disclosure have also been reported78.
In India, very few studies91011 have been undertaken regarding paediatric HIV status disclosure. Only one study has been done in Karnataka as part of a multicentre study, regarding the disclosure of HIV status and the pattern of disclosure of HIV status to CLHIV12. Hence, this study was undertaken to estimate the proportion of children who have been disclosed about their HIV status and to describe the pattern of HIV status disclosure, among the children visiting a district ART centre in coastal Karnataka.
Material & Methods
A cross-sectional study was conducted in an ART centre attached to a District General Hospital in Coastal Karnataka between October 2014 and July 2015. Sample size was calculated based on the pilot study, where the proportion of disclosure of HIV status was found to be 20 per cent. Expecting similar results, with an absolute precision of 5 per cent and 95 per cent confidence limits, a minimum sample of 175 individuals was needed for the study. Convenient sampling was done to recruit the study participants (Figure). Of the 594 CLHIV registered in the district, caregivers of 200 children aged 0-18 yr were approached for the study. Caregivers were excluded if their child was seriously ill. Necessary precautions were taken to avoid accidental disclosure to the child during the study. Ethical clearance was obtained from the Institutional Ethics Committee of the K. S. Hegde Medical Academy, Nitte University, Mangaluru and Karnataka State AIDS Prevention Society, Bengaluru.
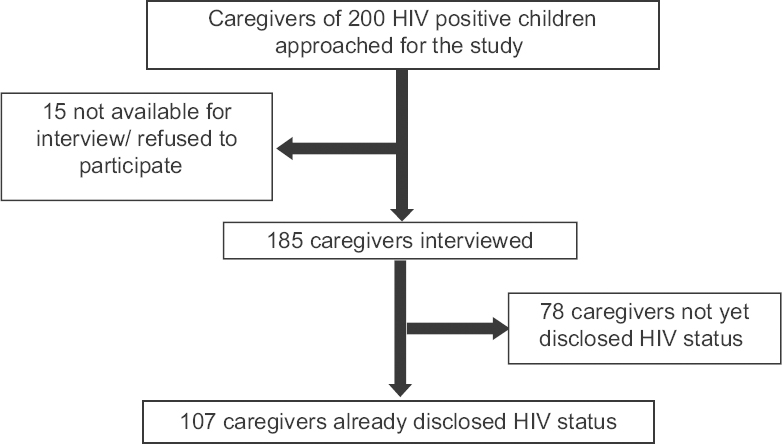
- Flowchart showing the recruitment of the study participants.
Method of data collection:Caregivers of all paediatric HIV patients attending the ART clinic were consecutively approached to assess eligibility. The data were collected after obtaining written informed consent. Data were collected by interview method, using a pre-formed, pre-tested by authors, semi-structured questionnaire, which was developed specially for the study. The questionnaire consisted of basic details of the children, basic details of the caregivers, clinical details of the children, status of disclosure and pattern of disclosure. This questionnaire was translated to the local language and retranslated to English to check for validity. Adherence was assessed by enquiring the caregivers on pill counts and missed doses and based on the response of the ART centre counsellors regarding their assessment of the child's adherence.
Definitions🙁i) Full disclosure: Where the caregiver has said that the child knows his/her HIV diagnosis13. (ii) Partial disclosure: Where the caregiver informs that the child has a serious, chronic illness without referring to the term HIV or when the child learnt about its HIV status on its own through various channels11. (iii) Caregiver: A person who lives with the child, participates in the child's daily care and is the most knowledgeable about the child's health13.
Statistical analysis:Frequencies and percentages were calculated for quantitative data. Chi-square and Fisher's exact tests were carried out to test significance. SPSS version 20.0 (IBM SPSS, Bengaluru), was used for the data analysis. During analysis, a cut-off of 10 yr was chosen to differentiate between adolescents and younger children, as per the WHO definition of adolescents14.
Results
Of the 200 children visiting the ART centre during the study period, 185 caregivers were available for the interview. The mean age of the children was 11±4 yr, and the median age at diagnosis of HIV was four years. The demographic details of the children are mentioned in Table I. There were four rehabilitation centres. Each caregiver in these centres had either one or two children under their care. A few of the children were staying with their parents in the rehabilitation centres.

Since around 64 per cent (n=118) of the children were double orphans and around 21 per cent (n=38) single orphans, it was not possible to assess the age, HIV infectivity status and educational levels of the biological parents. Based on the evaluation made by the ART centre staff into the probable mode of HIV infection of the child, vertical transmission was the most likely route. Ninety four per cent of the caregivers responded that the child was tested for HIV on the advice of a healthcare professional.
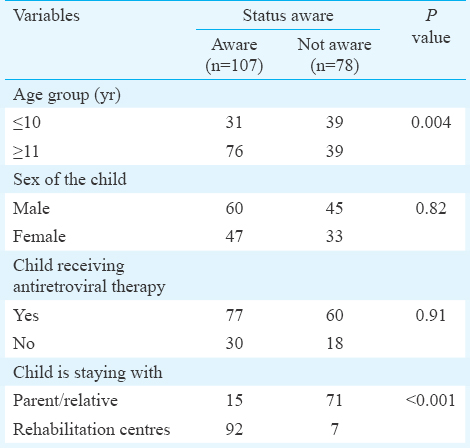
Among the 185 children, only 107 [57.8%; confidence interval (CI), 50.8-64.9%] children were aware of their HIV status, either fully or partially. The mean age of the child at the time of disclosure of HIV status was 9.75±1.86 yr with the minimum age at disclosure being five years and maximum being 15 yr. Table II depicts that the children were more likely to be told of their HIV status if they were aged 11 yr or older (P=0.004). Further analysis showed that children in the 11-15 yr age group constituted a majority in the above-mentioned age group. The children were more likely to be aware of their HIV status if they were residing in rehabilitation centres compared to those staying with their family (P< 0.001) (Table II). Among the children staying with their families, single mothers were more likely to disclose the HIV status to the child, when compared to those living with both parents, single fathers or relatives. However, this was not found to be significant.
On a sub-group analysis among the children who were disclosed (n=107), 89 per cent of the children had been disclosed fully as a planned event. In an equal proportion, HIV status was disclosed because the caregivers felt that it was the child's right to know about their HIV status. The pattern of disclosure of HIV status is described in Table III. Further analysis showed that the counsellors had disclosed the HIV status to the child because the caregivers felt that they may not be able to answer the questions posed by the children or because they did not know the process of disclosure. Among the children who were aware of their HIV status and were living with their families, partial disclosure of HIV status was more likely although this was not found to be significant.
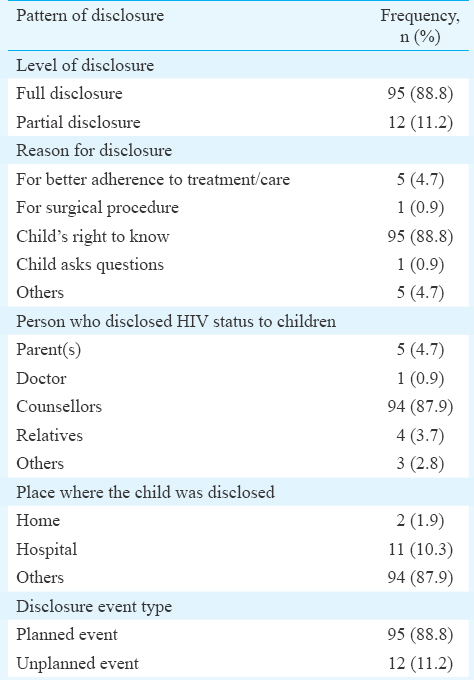
The most common reaction of the child to the disclosure process was sadness/worry (n=61, 57%) followed by no specific emotional reaction in 30 per cent. The remaining 13 per cent were angry when they came to know about their status. However, irrespective of their initial emotional reaction, the adherence to treatment or care either improved or was the same following disclosure in 106 of the 107 disclosed children. The emotional reactions of the caregivers were also similar to the children, wherein 42 and 45 per cent were sad and had no specific emotional change respectively, following the disclosure process. When the disclosure was done by the parents or relatives, they were relieved or happy following full disclosure.
Among the children who were aware of their HIV status, the level of disclosure was most likely to be full if the reason for disclosure was for better self-care (79, 83.2%). Partial disclosure was more likely if the children had learnt about the reasons for their medications on their own (8, 66.7%). Furthermore, it was observed that the children were more likely to be disclosed fully if they were aged 11-15 yr, a healthcare worker (counsellor) had disclosed to the child in a rehabilitation centre and were staying in a rehabilitation centre (P <0.001). The age, sex, whether the child was on ART or not did not influence the level of disclosure.
Among the children who had not been told about their HIV status (n=78), non-disclosure of HIV status was more likely if the child was staying with the parents/relatives. The most common reason for non-disclosure was that the caregivers felt that the child was too young and immature to be told about his/her HIV status (58%), particularly if the child was less than 10 yr of age.
Discussion
Our study revealed that majority of the children were in the 11-15 yr age group with a male predominance. Three-fourth of the children were receiving ART, and more than half of them were residing in the rehabilitation centres as nearly 85 per cent of the children were either single or double orphan. Only 58 per cent of the children were aware of their HIV status with 95 of them being fully aware of their HIV status. Children were more likely to be disclosed when they were 11-15 yr of age.
More than half of the children were aware of their HIV status in our study. This was similar to the findings of other studies78. The proportion of children aware of their HIV status in a study done in New Delhi was only 14 per cent9, whereas in another north Indian study it was only 41 per cent10. This might be because in both these studies, the disclosure was done by parents unlike in our study. The proportion of children aware of their HIV status varied across studies. A few studies in resource-limited settings also had similar results13151617. However, American studies had better proportion of disclosed children181920.
The proportion of the children who had been disclosed of their HIV status was highest between 11 and 15 yr of age. Systematic reviews done showed comparable results, with older children being more likely to be told about their HIV status78. In the study from north India, the mean age of disclosure was around nine years10. A couple of studies showed an earlier age of disclosure2122, where the disclosure was done at a mean age of about nine years, other studies as the one done by Arrivé et al23 reported a delayed age at disclosure. Consistent with the north Indian study10, the sex of the child and paternal/maternal orphan status did not influence the disclosure. In addition, there was no significant relationship between the treatment status and the disclosure status in our study as seen in a study in Kenya21.
Our study showed that in most cases the caregivers relied on counsellors to disclose the HIV status to the child. In one study10, the disclosure was done by either or both the parents in a majority of the children. Disclosure of HIV status was done as a discrete event at their homes unlike in our study, where the disclosure was done as a process in the rehabilitation homes. Our finding was unlike the results found by other studies, where the disclosure was done by relatives (grandmother)22, a parent/caregiver2324 among other studies. This might be due to the fact that a majority of the children in our study were either single/double orphan and were staying in rehabilitation centres.
A few children had gained partial knowledge regarding HIV from the posters and pamphlets at the ART centre, similar to the findings in a report25. With education being made mandatory for children, they learn to read and gain partial knowledge regarding HIV from the educational materials at the ART centre.
As mentioned in one of the reviews8, the adherence to medication had improved in the disclosed children as reported by the caregivers in our study, unlike the study in Kenya21 where non-adherence increased following disclosure. Akin to the findings of a study26, adherence had improved in our study following disclosure. Haberer et al27 also found that non-disclosure was a barrier to medication adherence.
The limitations of this study were that the children who visited the link ART centres for their medications and the children not on ART could not be interviewed. The caregivers/children attending the ART centre could be the ones who were adherent to treatment, and there was a chance that children on irregular treatment might have been missed. The sample size may not have been adequate as it has been calculated using the pilot study data. The caregivers’ reports could not be confirmed by child interviews. Furthermore, what exactly was disclosed at different ages could not be studied and no quantitative data were available for improved adherence.
In conclusion, our study showed that the caregivers relied on the counsellors in the rehabilitation centres to disclose the HIV status to the child after the child was 11-15 yr of age. The family members of the children should be encouraged and counselled to disclose to their own wards as it could be beneficial to both. Further studies on a larger scale are required to assess the details disclosed to the child at specific age and other HIV status disclosure patterns.
Acknowledgment
Authors thank the staff of the ART centre for assisting in recruiting the caregivers and in the data collection.
Financial support & sponsorship: Authors acknowledge financial support from the Indian Council of Medical Research, New Delhi by approving the study for MD/MS Thesis grant.
Conflicts of Interest: None.
References
- 2011. UNAIDS. UNAIDS Data Tables 2011. Geneva, Switzerland: UNAIDS; Available from: http://www.unaids.org/en/media/unaids/contentassets/documents/unaidspublication/2011/JC2225_UNAIDS_datatables_en.pdf
- 2015. National AIDS Control Organisation. India HIV Estimations. Available from: http://www.naco.gov.in/upload/2015%20MSLNS/HSS/India%20HIV%20Estimations%202015.pdf
- 2012-13. National AIDS Control Organisation. HIV Sentinel Surveillance. Technical Brief Available from: http://www.naco.gov.in/upload/NACP-IV/HSSTECHNICALBRIEF/HIVSentinelSurveillanceTechnicalBrief.pdf
- 2011. Guideline on HIV disclosure counselling for children up to 12 years of age. Geneva: WHO; Available from: http://www.whqlibdoc.who.int/publications/2011/9789241502863%5Feng.pdf
- Pediatric HIV disclosure: A process-oriented framework. AIDS Educ Prev. 2013;25:302-14.
- [Google Scholar]
- Centre for Disease Control. CDC Global Health-Stories - A New Model of Care for Children. Available from: http://www.cdc.gov/globalhealth/stories/care_for_children.htm
- Disclosure of HIV status to children in resource-limited settings: A systematic review. J Int AIDS Soc. 2013;16:18466.
- [Google Scholar]
- Disclosure of their HIV status to infected children: A review of the literature. J Trop Pediatr. 2013;59:84-9.
- [Google Scholar]
- Disclosure of the HIV infection status in children. Indian J Pediatr. 2009;76:805-8.
- [Google Scholar]
- Patterns of diagnosis disclosure and its correlates in HIV-Infected North Indian children. J Trop Pediatr. 2011;57:405-11.
- [Google Scholar]
- 2012. Disclosure of children's HIV status in four high prevalence States in India. Available from: http://www.snehagram.org/files/publications/studies1_April_2012.pdf
- Disclosure of HIV status: Perspectives from infected children in India. Int J Infect Dis. 2016;45(Suppl 1):265.
- [Google Scholar]
- Prevalence and pattern of disclosure of HIV status in HIV-infected children in Ghana. AIDS Behav. 2011;15:1121-7.
- [Google Scholar]
- HIV/AIDS: Definition of key terms. Available from http://www.who.int/hiv/pub/guidelines/arv2013/intro/keyterms/en/
- Factors associated with HIV/AIDS diagnostic disclosure to HIV infected children receiving HAART: A multi-center study in Addis Ababa, Ethiopia. PLoS One. 2011;6:e17572.
- [Google Scholar]
- Patterns of disclosure of HIV status to infected children in a Sub-Saharan African setting. J Dev Behav Pediatr. 2011;32:307-15.
- [Google Scholar]
- Communication between HIV-infected children and their caregivers about HIV medicines: A cross-sectional study in Jinja district, Uganda. J Int AIDS Soc. 2014;17:19012.
- [Google Scholar]
- Barriers to medication adherence in HIV-infected children and youth based on self- and caregiver report. Pediatrics. 2012;129:e1244-51.
- [Google Scholar]
- Impact of disclosure of HIV infection on health-related quality of life among children and adolescents with HIV infection. Pediatrics. 2009;123:935-43.
- [Google Scholar]
- Psychosocial implications of HIV serostatus disclosure to youth with perinatally acquired HIV. AIDS Patient Care STDS. 2011;25:257-64.
- [Google Scholar]
- A cross-sectional study of disclosure of HIV status to children and adolescents in Western Kenya. PLoS One. 2014;9:e86616.
- [Google Scholar]
- Disclosure of HIV/AIDS diagnosis to HIV-infected children in Thailand. J Paediatr Child Health. 2006;42:283-8.
- [Google Scholar]
- HIV status disclosure and retention in care in HIV-infected adolescents on antiretroviral therapy (ART) in West Africa. PLoS One. 2012;7:e33690.
- [Google Scholar]
- Patterns of HIV status disclosure to perinatally HIV-infected children and subsequent mental health outcomes. Clin Child Psychol Psychiatry. 2002;7:101-14.
- [Google Scholar]
- 2009. Facilitating HIV testing and disclosure with children and adolescents. India HIV/AIDS Alliance. Available from: http://www.allianceindia.org/wp-content/uploads/2014/07/2014_AllianceIndia_Facilitating-HIV-Testing-and-Disclosure-with-Children-and-Adolescents.pdf
- Barriers and facilitators to antiretroviral medication adherence among HIV-infected paediatric patients in Ethiopia: A qualitative study. SAHARA J. 2009;6:148-54.
- [Google Scholar]
- Excellent adherence to antiretrovirals in HIV+ Zambian children is compromised by disrupted routine, HIV nondisclosure, and paradoxical income effects. PLoS One. 2011;6:e18505.
- [Google Scholar]






