Translate this page into:
Pattern of episiotomy use & its immediate complications among vaginal deliveries in 18 tertiary care hospitals in India
Investigators listed in alphabetical order (Name of Centre): Chandra S. (Goa Medical College, Goa); Das M.C. (Guwahati Medical College, Guwahati); Das V. (Queen Mary's Hospital, Lucknow); Desai B.R. (JN Medical College, Belagari); Dhaliwal L.K. (PGIMER, Chandigarh); Habeebullah S. (JIPMER, Puducherry); Janakiram S.R. (Madurai Medical College, Madurai); Jhansi K.P. (SAT Hospital, Thiruvananthapuram); Madhini V. (IOG, Chennai); Mallik J.J. (SCB Medical College, Cuttack); Mittal S. (AIIMS, New Delhi); Mohanambal M. (RSRM Hospital, Chennai); Muthulakshmi M. (KMC Hospital, Chennai); Padbidri V.S. (KEM Hospital, Pune); Pagi S.L. (SSGH Medical College, Baroda); Salhan S. (SJ Hospital, New Delhi); Salvi V. (KEM Hospital, Mumbai); Subbiah V.N. (Government KGH Hospital, Chennai).
Reprint requests: Dr Shalini Singh, Division of Reproductive Biology & Maternal Health, Indian Council of Medical Research V. Ramalingaswami Bhawan, Ansari Nagar, New Delhi 110 029, India e-mail: shalinisingh.icmr@gmail.com
-
Received: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
In developed countries, efforts have been made to restrict episiotomy practice. However, in developing countries the episiotomy rates continue to be high. This study was conducted to evaluate the pattern of episiotomy use and its immediate complications among women delivering at tertiary level public hospitals in India.
Methods:
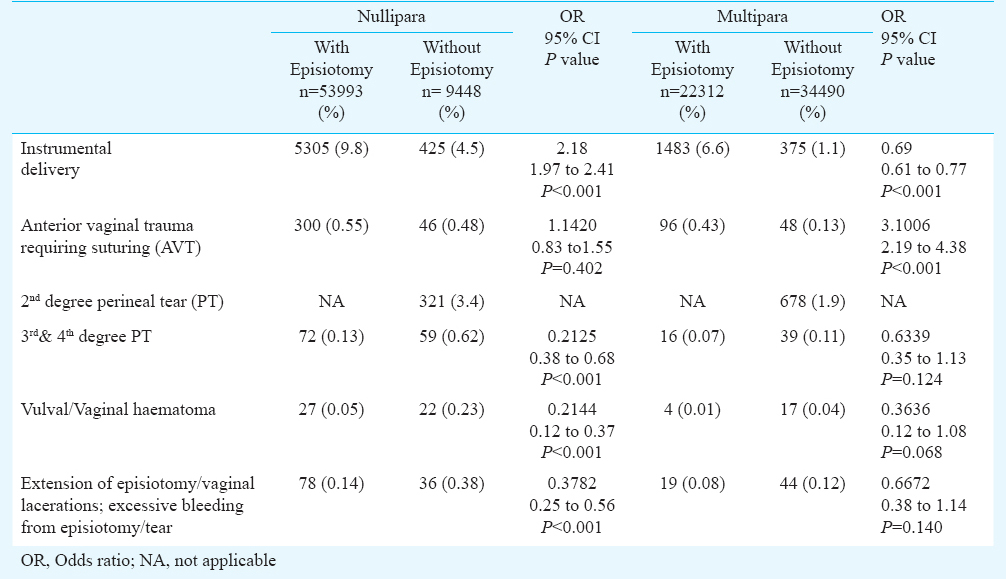
Prospective data of all women undergoing vaginal delivery including instrumental delivery were collected daily from the labour room registers of the 18 tertiary care hospitals on a structured proforma. Weekly data from all sites were sent to a central unit for compilation and analysis. Odds ratio was used to compare the proportion of genital trauma among women with and without episiotomy both in nulliparous and multiparous women.
Results:
Among 1,20,243 vaginal deliveries, episiotomy was performed in 63.4 per cent (n=76,305) cases. Nulliparaous women were 8.8 times more likely to undergo episiotomy than multiparous women. The various genital tract injuries reported were first degree perineal tear (n=4805, 3.9%), second degree perineal tear (n=1082, 0.9%), third and fourth degree perineal tear (n=186, 0.2%), anterior vaginal trauma requiring suturing (n=490, 0.4%), extension of episiotomy/vaginal laceration/excessive bleeding from episiotomy or tear (n=177, 0.15%), vulval/vaginal haematoma (n=70, 0.06%) and cervical tear (n=108, 0.08%). The combined rate of third and fourth degree perineal tears was observed to be significantly lower (P<0.001) among nullipara who received episiotomy (0.13%) compared to those who delivered without episiotomy (0.62%).
Interpretations & conclusions:
Significantly lower rates of third or fourth degree perineal tear were seen among nulliparous women undergoing episiotomy. The risk and benefit of episiotomy and its complications need to be evaluated through randomized clinical trials in the Indian context.
Keywords
Mediolateral episiotomy
perineal tear
vaginal deliveries
Episiotomy was introduced in the early 1920s, as a means to cut short second stage of labour and prevent to pernieal tears (PT) by widening the perineum1. Published literature from developed countries found no clear benefit of routine episiotomy2 while it reportedly increased frequency as well as severity of perineal damage3. Developed countries like Australia, Canada and Sweden made efforts to use episiotomy only for selected indications456. However, in developing countries, the episiotomy rates continue to be high. A survey conducted among eleven developing countries including India across the Global Network for Women's and Children's Health Research sites (2003) reported over 90 per cent episiotomy rates among nullipara though overall rate was about 40 per cent7. There is lack of data from India on the pattern of episiotomy use and its immediate complications among facility births. This study was conducted to evaluate the pattern of episiotomy use and its immediate complications among women delivering at tertiary level public hospitals in India.
Material & Methods
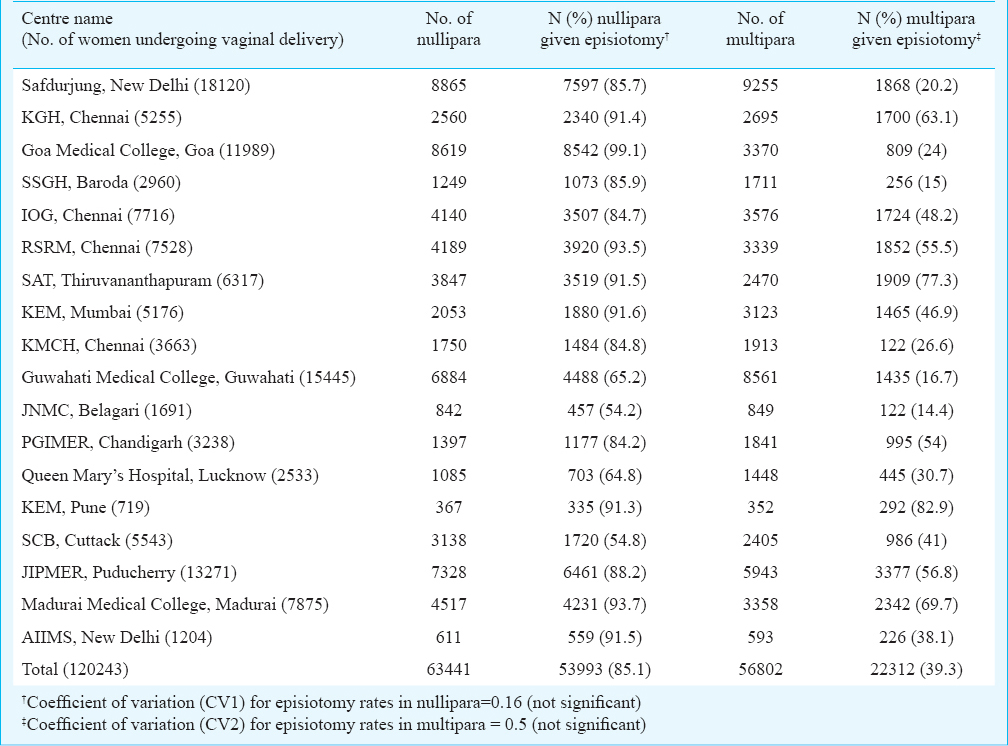
This observational study was carried out during January to December 2009 through the network of Human Reproduction Research Centers (HRRCs) of Indian Council of Medical Research (ICMR), New Delhi, located in the departments of Obstetrics and Gynaecology in 18 tertiary care hospitals in different parts of the country (Table I). The annual deliveries were more than 10,000 in seven hospitals, between 5000 to 10,000 in five and 1000 to 5000 in the remaining sites. The client population of these hospitals comprised mostly of lower and middle income groups.
At the time of the study, all hospitals performed mediolateral episiotomy and none of the hospitals had a policy of selective episiotomy use. Prospective data of all women having vaginal delivery including instrumental delivery were abstracted daily from the labour room register by trained staff on a structured proforma. Weekly data from all sites were sent to a central unit for compilation and analysis. Data collected included parity, mode of delivery, immediate genital injuries such as anterior and posterior perineal trauma, cervical tear, extension of episiotomy, vulval and/or vaginal haematoma etc. Perineal tear (PT) was classified into four categories8: 1st degree- injury to perineal skin only; 2nd degree - injury to perineum involving perineal muscles but not involving the anal sphincter; 3rd degree - injury to perineum involving the anal sphincter complex; and 4th degree - injury to perineum involving the anal sphincter complex and anal epithelium. Immediate perineal complications following vaginal delivery such as anterior vaginal trauma requiring suturing (AVT), PTs including 1st, 2nd, 3rd and 4th degree, excessive bleeding from episiotomy or vaginal laceration, vaginal/vulval haematoma and extension of episiotomy/severe vaginal laceration were collectively termed as composite complications.
Data were entered in MS Excel and analyzed as simple proportions and percentages. Mathematical calculations were done using conventional statistical formulae. Descriptive and inferential principles were used to draw conclusions from the study. Fisher's exact test was used for categorical data. Correlation coefficient (r) was calculated to examine the relationship between episiotomy rates, instrumental delivery and complications. Odds ratio was used to compare the proportion of genital trauma among women with and without episiotomy both in nulliparous and multiparous women.
Results
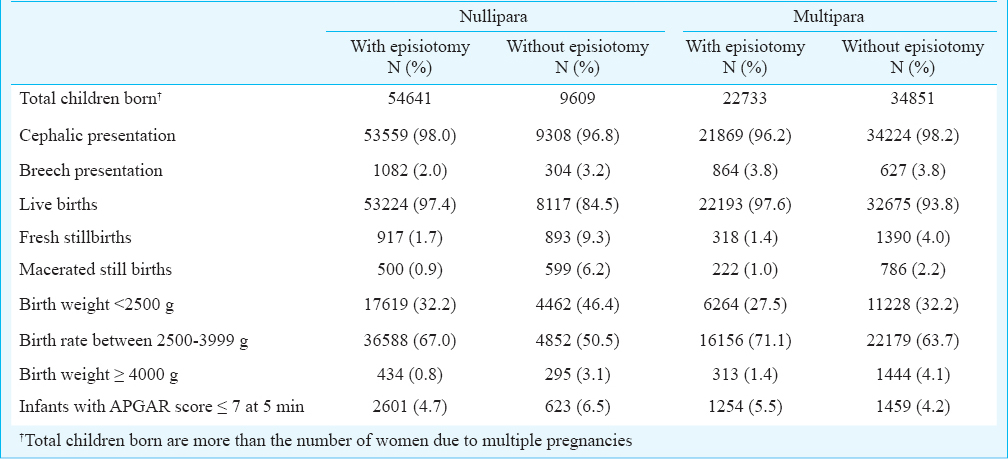
A total of 1,77,252 births took place during the study period. Of these, 1,20,243 (67.8%) were vaginal deliveries and 57,009 (32.2%) were caesarean sections. Episiotomy was performed in 76,305 (63.4%, 95% CI=63.2 to 63.7%) of the vaginal deliveries. The mean episiotomy rates among nullipara and multipara were 85.1 and 39.3 per cent, respectively (Table I). The coefficient of variation (CV) in episiotomy rates in nulliparous and multiparous women were 0.16 and 0.5, respectively which was not significant (Table I). Overall, nulliparous women were 8.8 times (95% CI= 8.59 to 9.08) more likely to undergo episiotomy than multiparous women (Figure). Table II describes the mode of presentation and birth outcome of children born of the women delivering with and without episiotomy segregated by parity.
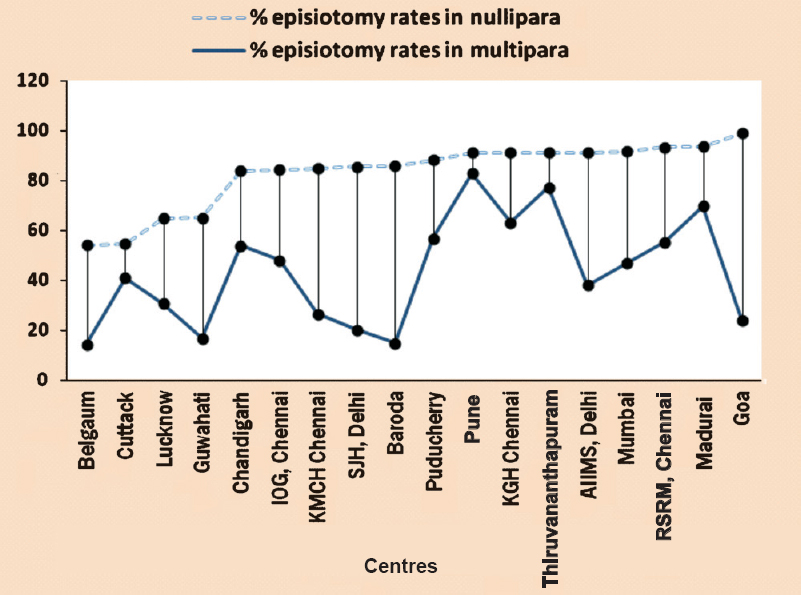
- Distribution of episiotomy rates in multipara with ascending rates of episiotomy in nullipara.
The overall rate of instrumental delivery was reported to be 6.3 per cent (Table III). The rate of composite complications was 5.7 per cent which included first degree PT (n=4805, 3.9%), second degree PT (n=1082, 0.9%), third and fourth degree PT (n=186, 0.2%), AVT (n=490, 0.4%), extension of episiotomy/vaginal laceration/excessive bleeding from episiotomy or tear (n=177, 0.15%) and vulval/vaginal haematoma (n=70, 0.06%). The rate of cervical tear was 0.08 per cent. The site-wise distribution of episiotomy use, instrumental vaginal delivery and composite complication rates among vaginal deliveriesis provided in Table III. The correlation of overall episiotomy use and instrumental deliveries with perineal complications in participating sites was not significant.
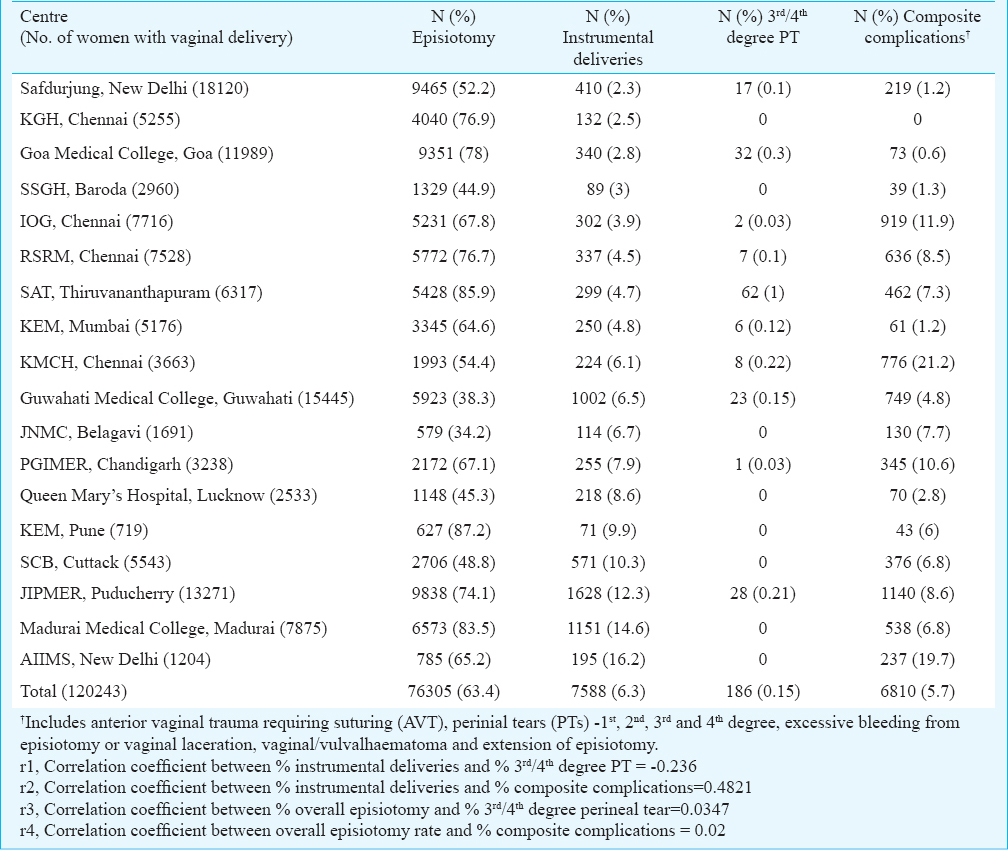
Women were classified in two groups - nulliparous and multiparous to analyze the effect of episiotomy on perineal complications. The presence or absence of tearing (anterior vaginal or perineal) and other complications in both nulliparous and multiparous women is summarized in Table IV. The combined rate of third and fourth degree perineal tears was observed to be significantly lower (P<0.001) among nullipara who received episiotomy (0.13%) compared to those who delivered without episiotomy (0.62%). Significantly lower rates of vulval/vaginal haematoma (OR=0.4575, 95% CI=0.28 to 0.73, P=0.001) and other complications like extension of episiotomy or vaginal lacerations, excessive bleeding from episiotomy or tear (OR=0.6978, 95% CI=0.51 to 0.93, P=0.017) were noted in all those women given episiotomy.
Discussion
Episiotomy is one of the most commonly employed procedures for women delivering in tertiary level public hospitals in India with an overall episiotomy rate of about 70 per cent9. The episiotomy rate among nullipara (85%) in our study was similar to that reported in a population based cross-sectional study from Chennai (83.4%)10.
We compared our results with published literature reporting mediolateral episiotomy and found conflicting evidence on the role of episiotomy in preventing perineal tears. The policy of restrictive episiotomy use at John Radcliffe Hospital in Oxford during 1980-1984 resulted in a decrease in the episiotomy rate from 73 to 45 per cent but an increase in second degree perineal tears from 7 to 20 per cent. However, third degree perineal tear rate remained unchanged at 5 per cent11. Sleep et al12 randomized 1000 women during spontaneous vaginal delivery to either restricted or liberal approach without an overall increase in severe perineal trauma and there were both more posterior tears and more intact perineums in the restricted group. In another study, perineal suturing rates were compared among nullipara and multipara who were randomized to either routine or restrictive episiotomy use13. No difference in perineal suturing rate was found among nullipara. However, the multipara had significantly higher rates of intact perineum and benefited from restrictive episiotomy policy13.
A randomized controlled trial conducted by Argentina Episiotomy Trial Collaborative Group14 found that the relative risk of severe perineal trauma was similar in both routine and selective groups irrespective of parity; 28 per cent fewer women in selective group required perineal suturing. They concluded that episiotomy rate of 30 per cent which was seen in the selective group was justified. They also reported an increase in the anterior tears in the selective group. In our study, a higher rate of anterior perineal trauma was observed in women who received episiotomy; however, this increase was significant only for multipara.
In a Cochrane systematic review of eight randomized controlled trials15 (six studies with mediolateral and two with median episiotomy practice) comparing effects of selective versus routine use of episiotomy, an overall less severe perineal trauma (RR= 0.67, 95% CI= 0.49 to 0.91), less posterior perineal trauma (RR 0.88, 95% CI 0.84 to 0.92), less suturing (RR 0.71, 95% CI 0.61 to 0.81) and fewer healing complications at seven days (RR 0.69, 95% CI 0.56 to 0.85) in the restrictive episiotomy group were reported. It concluded that evidence did not support routine episiotomy.
In our study, a higher rate of second degree perineal tear was seen among nullipara as compared to multipara who delivered without episiotomy. The third or fourth degree perineal tear rate was significantly lower among nullipara given episiotomy but not in multipara. A study from a tertiary care center in south India10 reported 1.6 per cent second degree perineal tear among multipara with routine use of episiotomy which was comparable to our results. After applying a policy of restricted episiotomy use; there was an increase in second degree perineal tear from nil to 13 per cent and from 1.6 to 10 per cent among nullipara and multipara, respectively. Third and fourth degree perineal tear also increased from nil to 2 per cent only in the nullipara10. An observational study from public hospitals in Hong Kong indicated that the policy of routine episiotomy was associated with a significantly lower occurrence of any type of perineal tear and severe-degree (third or fourth degree) tear in nulliparous women than those without16.
Independent association of episiotomy with obstetric anal sphincter injuries (OASIS) was estimated from birth records in Finland from 2004-2011using a cross-sectional and then a matched pair analysis17. The incidence of OASIS among nullipara with episiotomy was 2.3 and 1.0 per cent among women without episiotomy, and 0.6 and 0.2 per cent, respectively among multipara. A matched pair analysis showed a reduction in adjusted odds ratio of OASIS associated with episiotomy due to confounding by indication. The authors have concluded that the association between episiotomy and OASIS needs to be interpreted with caution in observational studies17. Therefore, a hospital policy of selective episiotomy might result in an increase in perineal tear but an overall reduction in rate of perineal suturing. The influence of maternal factors such as tight perineum, early bearing down, provider factors such as perineal support, flexion of head during delivery, good nursing care and perineal massage in late pregnancy for the prevention of perineal tears need to be evaluated further as some studies indicate protective role of perineal protection strategies1819.
The major limitation of this study was its observational study design with collection of only hospital level data. Late complications such as infection, pain, dyspareunia, etc. Could not be recorded. Indication for performing episiotomy was also not available in the records. A major strength of this study was direct information collected from labour room records and large sample size, which reflects the current episiotomy practice in public hospitals in India. The incidence of immediate perineal complications among vaginal deliveries has not been reported from tertiary care hospitals in India. This data will be useful to design interventional studies. It will also contribute towards developing guidelines for episiotomy use in the Indian context.
In this study population significantly lower rates of third or fourth degree perineal tear were seen among nullipara undergoing episiotomy. The risk and benefit of episiotomy and its indications especially for nullipara need to be evaluated through randomized clinical trials. There is also a need to evolve evidence based practice guidelines for use of episiotomy in India.
Acknowledgment
The authors acknowledge Dr Abha Agarwal, National Institute of Medical Statistics, New Delhi for providing statistical inputs.
Conflicts of Interest: None.
References
- Changes in episiotomy practice: evidence-based medicine in action. Expert Rev of Obstet Gynecol. 2010;5:301-9.
- [Google Scholar]
- Benefits and risks of episiotomy: an interpretative review of the English language literature, 1860-1980. Obstet Gynecol Surv. 1983;38:322-38.
- [Google Scholar]
- Benefits and risks of episiotomy: A review of the English-language literature since 1980. Part II. Obstet Gynecol Surv. 1995;50:821-35.
- [Google Scholar]
- Rates for obstetric intervention among private and public patients in Australia: population based descriptive study. BMJ. 2000;321:137-41.
- [Google Scholar]
- Reducing the frequency of episiotomies through a continuous quality improvement program. Can Med Assoc J. 1995;153:275-82.
- [Google Scholar]
- Changed pattern in the use of episiotomy in Sweden. Br J Obst Gynaecol. 1999;106:95-101.
- [Google Scholar]
- Episiotomy rates from eleven developing countries. Int J Gynaecol Obstet. 2005;91:157-9.
- [Google Scholar]
- Normal labor and delivery. In: Cunningham F, Leveno KJ, Bloor S, Hauth J, Rouse DJ, Spong C, eds. William's obstetrics (23rd ed). New York: McGraw-Hill; 2011.
- [Google Scholar]
- Changes in the management of labour: 2. Perineal management. Can Med Assoc J. 1987;136:1045-9.
- [Google Scholar]
- Does episiotomy prevent perineal trauma and pelvic floor relaxation? Online J Curr Clin Trials 1992 Jul 1: Doc No 10
- [Google Scholar]
- Argentina Episiotomy Trial Collaborative Group. Routine vs selective episiotomy: a randomised controlled trial. Lancet. 1993;342:1517-8.
- [Google Scholar]
- The practice of episiotomy in public hospitals in Hong Kong. Hong Kong Med J. 2006;12:94-8.
- [Google Scholar]
- The association of episiotomy with obstetric anal sphincter injury - a population based matched cohort study. PLoS One. 2014;9(9):e107053.
- [Google Scholar]
- Factors associated with perineal lacerations requiring suture in vaginal births without episiotomy. Obstet Gynecol. 2014;123(Suppl 1):63S-4S.
- [Google Scholar]
- Is it possible to never perform episiotomy during vaginal delivery? Obstet Gynecol. 2014;123(Suppl 1):38S.
- [Google Scholar]






