Translate this page into:
Outcomes of surgical interventions for the treatment of limbal stem cell deficiency
For correspondence: Dr Radhika Tandon, Cornea, Cataract & Refractive Services, Dr Rajendra Prasad Centre for Ophthalmic Sciences, All India Institute for Medical Sciences, New Delhi 110 029, India e-mail: radhika_tan@yahoo.com
-
Received: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
In the current scenario, with availability of different surgical procedures for limbal stem cell deficiency (LSCD), there exists no common consensus as to the standardization of the management protocol for the same. In addition, there also exists diversity in the views about the clinical diagnosis, ancillary investigations and clinical parameters. The objective of the present study was to evaluate the reported outcomes of surgical interventions for the management of LSCD.
Methods:
A systematic review of published literature on limbal stem cell transplantation (LSCT) was performed using Ovid Medline, Embase and PubMed for a duration of 2009 to 2019. Original studies including prospective, retrospective case series and randomized controlled trials, articles in English language, articles with access to full text and studies with more than or at least 10 patients were included in this review. Data related to clinical and visual outcomes were evaluated, and pool estimates of different surgeries were calculated using random-effects model and individually using Pearson’s Chi-square test.
Results:
A total of 1133 abstracts were evaluated. Finally, 17 studies were included for the analysis. Among these 17 studies, direct limbal lenticule transplantation was performed in five studies, of which autologous tissue from the fellow eye [conjunctival limbal autograft (CLAU)], allograft from a cadaver/live donor [keratolimbal allograft (KLAL)/conjunctival limbal allograft (CLAL)] and combination of CLAU plus KLAL were done in one, three and one studies, respectively. The ex vivo expanded cultivated limbal epithelial transplantation (CLET) was reported in six studies and simple limbal epithelial transplantation (SLET) in four studies. Two were comparative studies comparing CLET and CLAL (living-related CLAL) with cadaveric KLAL, respectively. Outcome analysis of the included studies showed significant heterogeneity. Calculated pool rate for various types of surgeries was calculated. The pool estimate for CLAL was 67.56 per cent [95% confidence interval (CI), 41.75-93.36; I2=83.5%, P=0.002]. For KLAL, this value was 63.65 per cent (95% CI, 31.38-95.91; I2=92.4%, P=0.000). Pool estimate for CLET was 78.90 per cent (95% CI, 70.51-87.28; I2=73.6%, P=0.001). Corresponding values for SLET were 79.08 per cent (95% CI, 74.10-84.07; I2=0.0%, P=0.619). CLAU and combination of CLAU plus KLAL were done in one study each; hence, statistical analysis could not be done. The functional outcome in terms of gain in visual acuity post-operatively was better in KLAL (P<0.005) and SLET group as compared to CLET group.
Interpretation & conclusions:
The present analysis suggests that though the anatomical success rates were almost identical between SLET, CLET, CLAL, and KLAL procedures, the functional success rates were better following KLAL and SLET procedures as compared to CLET. Decision for LSCT for cases of ocular burns based on either clinical judgement of the surgeon or individual diagnosis remains a suitable option.
Keywords
Chemical injury
cornea
limbal stem cell deficiency
limbus
ocular burns
ocular surface
transplantation
Limbal stem cells are essential for maintaining corneal transparency, as these cells constantly replenish damaged corneal epithelial cells1. Various factors can be attributed to limbal stem cell damage. These include physical, chemical, thermal and immunological insults, of which chemical injury contributes a major proportion. Limbal stem cell deficiency (LSCD) manifests in the form of chronic ocular surface inflammation with persistent epithelial defects, corneal vascularization and conjunctivalization eventually, leading to visual disturbance1. Management of ocular stem cell deficiency has slowly gained momentum with emerging techniques and surgical interventions2. Over the past several years, evidence-based research has suggested a potential role of diverse surgical modalities for replenishment and restoration of the architecture of the limbal stem cells and ocular surface. The treatment modalities have gradually evolved to the present surgical techniques to address the problems of LSCD and provide better outcomes.
The choice of procedure for LSCD depends on the extent of the ocular surface involvement (partial vs. total), the laterality (unilateral or bilateral), absence or presence of ongoing inflammation or infection and associated secondary glaucoma. Partial LSCD can be treated by either denuding cornea at visual axis or resurfacing the cells from the unaffected healthy limbal epithelium3456. However, in cases with total LSCD, either autologous limbal lenticule from the fellow eye or allograft from the cadaver/live-related donors is required7891011121314151617. However, with the availability of different surgical procedures, there lies no common consensus as to the standardization of the management protocol for cases with LSCD. There also exists diversity in the views about the clinical diagnosis, ancillary investigations and clinical parameters. Conjunctivalization, vascularization and loss of transparency are the significant parameters used to establish the diagnosis. Impression cytology and ocular surface staining are among the ancillary investigations described in the past18.
In the present systematic review, surgical interventions including direct transplantation of the limbal lenticule either as an autologous tissue from the fellow eye [conjunctival limbal autograft (CLAU)]19 and a keratolimbal allograft (KLAL) from a cadaver and from live donor [conjunctival limbal allograft (CLAL)]2021222324 or the combination of the25 two were evaluated. In addition to direct transplantation of limbal lenticule, ex vivo expanded cultivated limbal epithelial transplantation (CLET)262728293031 and simple limbal epithelial transplantation (SLET)32333435 were evaluated, and the results of these surgical interventions were discussed. In the present review, though cultivated oral mucosal epithelial transplantation (COMET) studies have been described as this procedure has been reported to promote re-epithelialization and helped in reducing inflammation in patients with acute LSCD3637383940, COMET studies have not been included in the analysis.
The objective of this systematic review was to evaluate and compare the efficacy/outcomes of different surgical interventions for LSCD. This was done to analyze and strengthen evidence to facilitate the adoption of best clinical and surgical practices for the management of LSCD.
Material & Methods
The study was conducted in accordance with the PRISMA guidelines for systematic review41. Documentation of data was done following a set protocol before commencement of literature search.
Outcome measures: The primary objective was to determine the best acceptable practices for surgical management of LSCD. Data related to surgical outcomes were evaluated in terms of anatomical success (absence of persistent epithelial defect, vascularization and conjunctivalization) and functional success (improvement in visual acuity).
Methods followed for study selection: Electronic literature search using Ovid Medline, Embase and PubMed was performed for studies published from 2009 to 2018 using limbal stem cell, limbal stem cell deficiency, chemical injury or ocular burns, conjunctival limbal autograft transplantation, cultivated limbal epithelial transplantation, simple limbal epithelial transplantation, cultured ocular mucosal epithelial transplantation and limbal stem cell transplant as keywords. Search was further supplemented by retrieving cross-references. Studies which were published before 2009 were excluded from this analysis, as Cauchi et al42 published a review article on related literature till 2008. Recently, Shanbhag et al43 published a systematic review on outcomes of three different techniques of autologous limbal stem cell transplantation (LSCT) in unilateral LSCD.
Eligibility criteria: Original studies including prospective, retrospective case series and randomized controlled trials, articles in English language, those with access to full text and those with at least 10 or more patients were included in this review. Experimental, animal studies and correspondences letters were excluded.
A total of 1133 abstracts were identified through database search and 15 additional studies were found to be relevant after checking cross-references. Of the total 1148 articles, 21 records were selected for analysis after removing duplicate studies and studies not directly related to the review topic. Of these, four more articles were excluded, reason being animal/experimental studies and case reports with one or two patients only. Finally, 17 studies were incorporated in the final analysis for quantitative and qualitative assessment (Fig. 1).
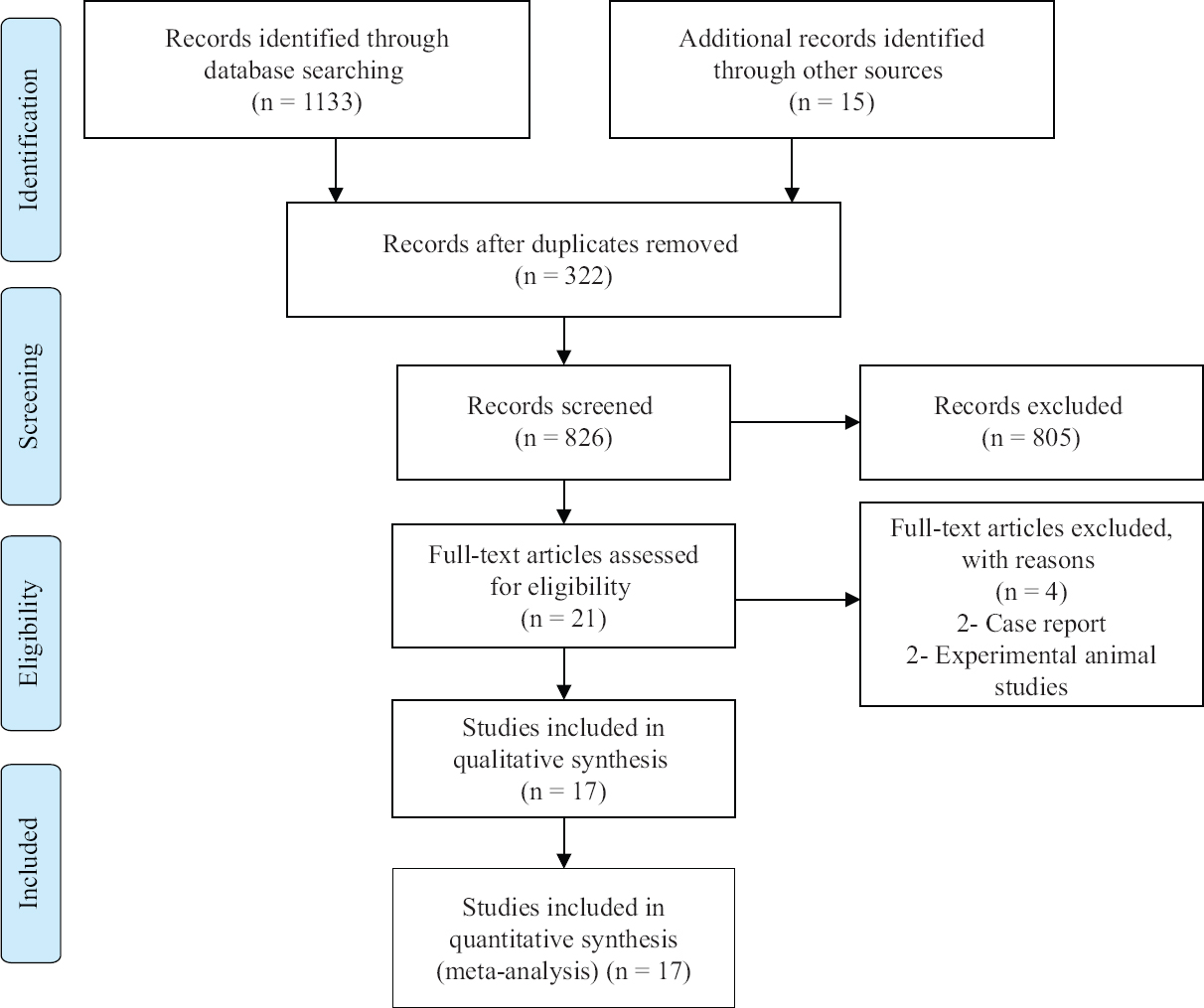
- Flowchart representing study selection process as per the PRISMA guidelines.
Interventions: Various surgical modalities of LSCT such as CLAU, CLAL, KLAL, CLET, COMET and SLET were evaluated.
Study selection & data extraction: Three authors have done eligibility assessment independently in an unblended standardized manner. Wherever full manuscript was available, it was carefully reviewed by all the three reviewers. Any disagreement between the three was resolved by unanimous consensus. While extracting data, relevant parameters, i.e. author’s name, name of the journal, year of publication, type of study design and various factors, that can affect outcomes were noted carefully.
Assessment of methodological quality of the selected studies: As per the PRISMA guidelines, methodological quality of each component study was evaluated. Score was given depending upon the answers to certain questions, such as, whether operating surgeon concealed to the reviewer of outcomes or not, whether dropouts were <15 per cent or not, whether follow up intervals were pre-specified or patients’ charts were just reviewed and whether detailed description of outcomes were there or not41. Scoring was done as 2, 1 and 0 for clearly affirmative, probably affirmative or clearly negative answer, respectively.
Statistical analysis: Stata 15.0 (StataCorp LLC, College Station, TX 77845, USA) statistical software was used for analysis. The pooled estimates [95% confidence interval (CI)] for anatomical success after LSCT (absence of persistent epithelial defect, vascularization and conjunctivalization)1 were calculated using random-effects model for CLAL, CLET, KLAL and SLET procedures. Random-effects model was used to pool the various studies results as per the type of surgical interventions. Outcome analysis of the included studies was evaluated by calculating pool estimate value with 95 per cent CI. Data from all the included studies were divided and subdivided depending upon the type of intervention, i.e. CLAL, KLAl, CLET and SLET. However, CLAU and combination of CLAU plus KLAL were done in one study each; hence, the pooled estimate could not be calculated for these two. However, anatomical success after LSCT (absence of persistent epithelial defect, vascularization and conjunctivalization) and functional success (improvement in visual acuity) were compared between various surgical groups using Pearson’s Chi-square test.
Results
The surgical outcomes in terms of anatomical and functional (visual) success were assessed in details for seventeen eligible studies1920212223242526272829303132333435.
Study quality: All 17 studies (100%) achieved adequate follow up and had mentioned detailed description of outcome criteria, dropouts were <15 per cent and pre-specified and follow up parameters were mentioned. The quality score ranged from 6 to 7 points with mean and median value of 6.05 and 6, respectively.
Owing to statistical heterogeneity, the outcomes of different type of surgeries were analyzed separately by calculating pooled estimate. Hence, the outcomes of surgical interventions are summarized in a descriptive manner as well. The demographic and descriptive characteristics of the included studies are shown in the Table.
| Authors | Eye laterality | Type of study | Intervention | Number of patients | Mean age (yr) | Mean follow up (months) | MC primary pathology | Number of patients with MC primary pathology (n) | Primary success (%) | Secondary success (%) | Failure (%) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Baradaran-Rafii et al19 | U/L LSCD | Retrospective | CLAU | 34 | 27.3 | 17.2 | Chemical injury | 25 | 88 | 88 | 11.8 |
| Barreiro et al20 | U/L+B/L | Retrospective | CLAL (live related) | 34 | 37.3 | 18.9 | Chemical | 34 | 47.4 | 82.1 | 52.6 |
| Scocco et al21 | B/L | Retrospective | CLAL (live related) | 32 | 33.62 | 48.7 | SJS | 14 | 84.6 | 46.2 | 15.4 |
| Baradaran-Rafii et al22 | B/L | Retrospective | KLAL | 45 | 26.7 | 26.1 | Chemical | 36 | 73.4 | 84.8 | 26.6 |
| Chan et al25 | U/L | Prospective, interventional case series | CLAU + KLAL | 11 | 31.6 | 35.8 | Chemical | 6 | 82 | 73 | 18 |
| Vazirani et al26 | U/L | Retrospective | CLET | 70 | 24 | 17.5 | Chemical | 28 | 75 | 66.6 | 25 |
| Sangwan et al27 | U/L | Retrospective | CLET | 200 | 24.1 | 36 | Chemical | 162 | 71 | 60.5 | 29 |
| Prabhasawat et al28 | U/L+B/L | Prospective | CLET | 18 | 44.7 | 26.1 | Chemical | 13 | 77.9 | 73.7 | 26.3 |
| Rama et al29 | U/L+B/L | Prospective | CLET | 112 | 46.5 | 34.9 | Chemical | 109 | 89.7 | 41.07 | 10.3 |
| Shortt et al30 | U/L+B/L | Prospective | CLET | 10 | 46.1 | 13 | Chemical | 4 | 60 | 60 | 40 |
| Ramírez et al31 | U/L+B/L | Prospective | CLET | 19 | 51.6 | 36 | Non-IF cause* | 9 | 80 | 50 | 20 |
| Vazirani et al32 | U/L | Retrospective | SLET | 68 | 22 | 12 | Chemical | 62 | 83.8 | 64.7 | 16.2 |
| Basu et al33 | U/L | Prospective | SLET | 125 | 62.5 | 18 | Chemical | 125 | 76 | 75.2 | 18.4 |
| Basu et al34 | U/L | Prospective case series | SLET | 30 | 15 | 27.6 | Chemical | 30 | 80 | 62.5 | 23.3 |
| Gupta et al35 | U/L | Prospective case series | SLET | 30 | G1:29.1 G2:9.1 |
12 12 |
Chemical | 38.8 83.3 |
70 83.3 |
71.4 71.4 |
30 16.7 |
| Comparative, prospective interventional studies | |||||||||||
| Titiyal et al23 | U/L | Prospective | CLAL (G1) versus KLAL (G2) | 20 | G1:18.1 G2:17 |
6 | Chemical/thermal burns | 20 | G1:70 G2:20 |
G1:80 G2:40 |
G1:30 G2:80 |
| Parihar et al24 | B/L | Prospective | CLET (G1) versus KLAL (G2) |
40 50 eyes |
G1:46 G2:48 |
12 | Chemical/thermal burns | 32 | G1:86.96 G2:91.67 |
G1:76 G2:72 |
G1:NA G2:NA |
U/L, unilateral; B/L, bilateral; CLAU, conjunctival limbal autograft i.e., direct transplantation of the limbal tissue lenticule (autologous tissue); KLAL/CLAL, keratolimbal allograft/conjunctival limbal allograft i.e., allograft from a cadaver/live donor; CLET, ex vivo expanded cultivated limbal epithelial transplantation; SLET, simple limbal epithelial transplantation; COMET, cultivated oral mucosal epithelial transplantation; SJS, Steven-Johnson syndrome; IF, inflammatory; G1, group 1; G2, group 2; LSCD, limbal stem cell deficiency; MC, multiple sclerosis
Calculated pool rate for various types of surgeries was calculated. The pool estimate for CLAL was 67.56 per cent (95% CI, 41.75-93.36; I2=83.5%, P=0.002) as depicted in Fig. 2. For KLAL, the values were 63.65 per cent (95% CI, 31.38-95.91; I2=92.4%, P=0.001) as depicted in Fig. 3. Pool estimate for CLET was 78.90 per cent (95% CI, 70.51-87.28; I2=73.6%, P=0.001) as depicted in Fig. 4. Corresponding values for SLET were 79.08 per cent (95% CI, 74.10-84.07; I2=0.0%, P=0.619) as depicted in Fig. 5. CLAU and combination of CLAU plus KLAL were done in one study each; hence, statistical analysis could not be done.
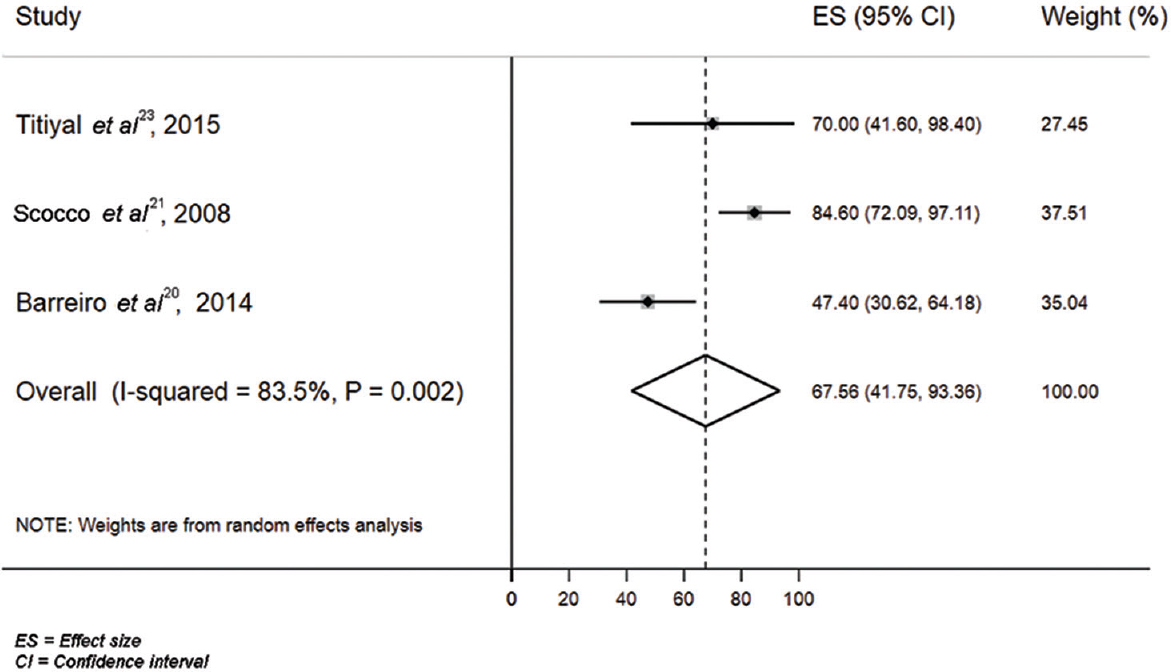
- Clinical outcome pooled estimate for conjunctival limbal allograft surgery.
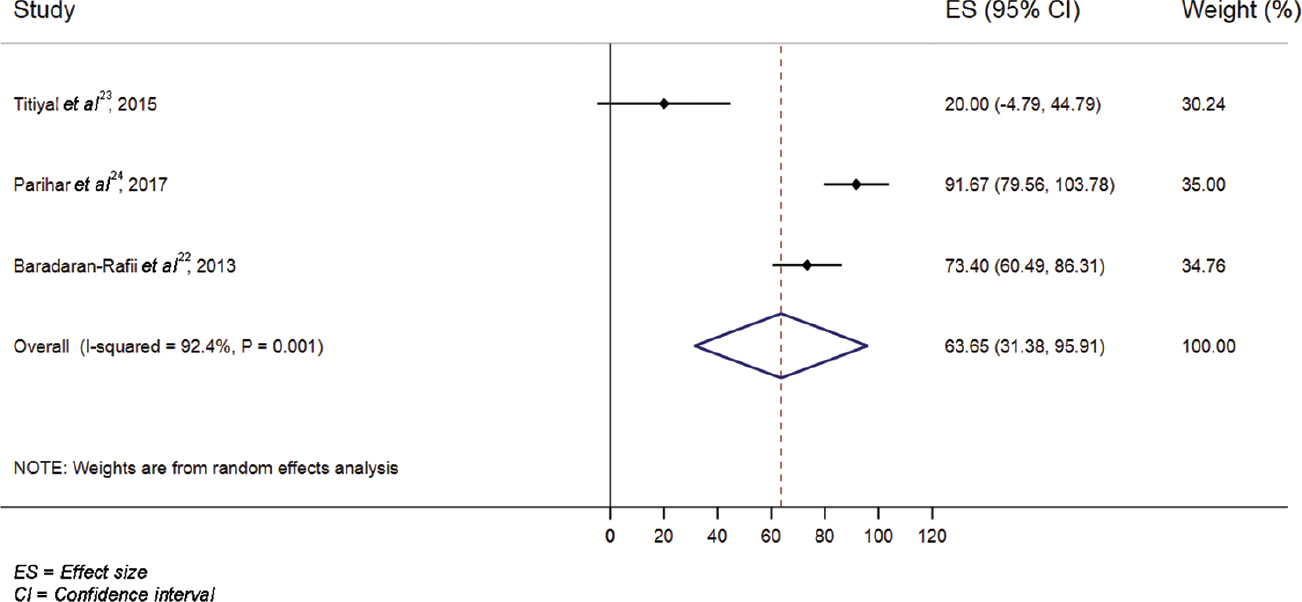
- Clinical outcome pooled estimate for keratolimbal allograft surgery.
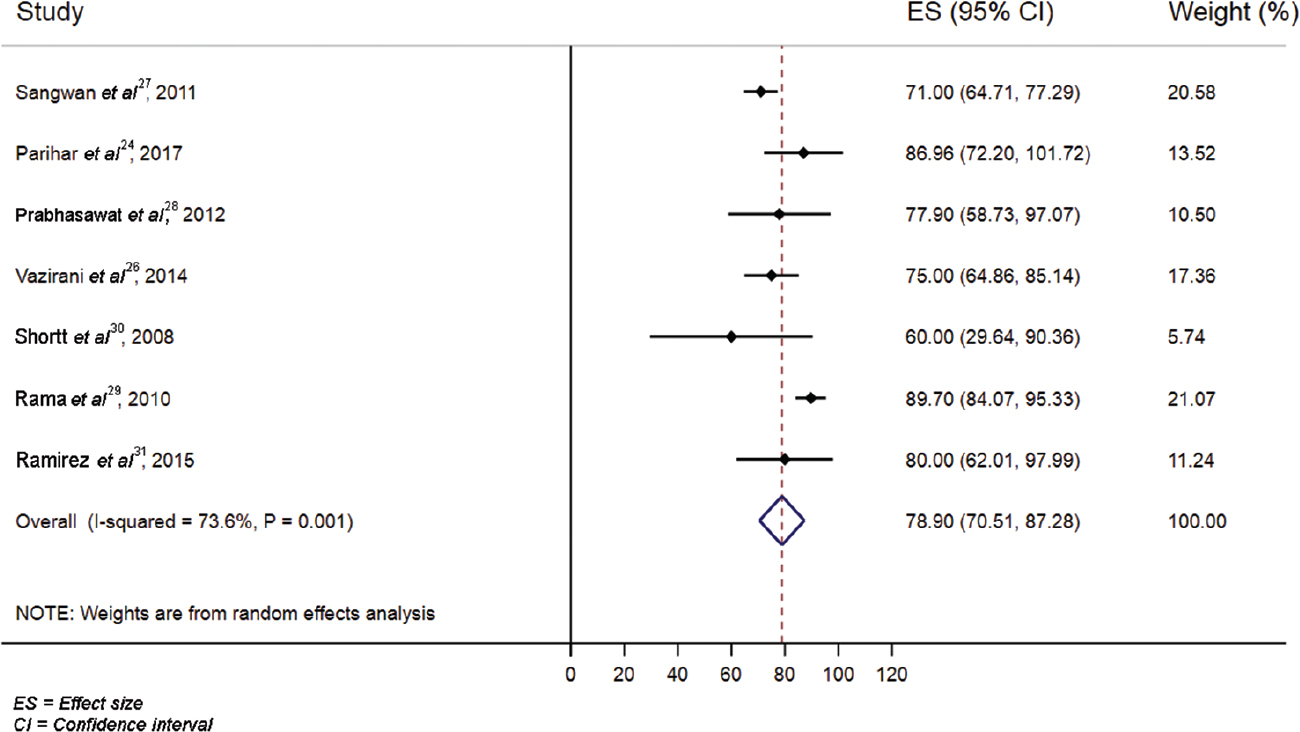
- Clinical outcome pooled estimate for cultivated limbal epithelial transplantation surgery.
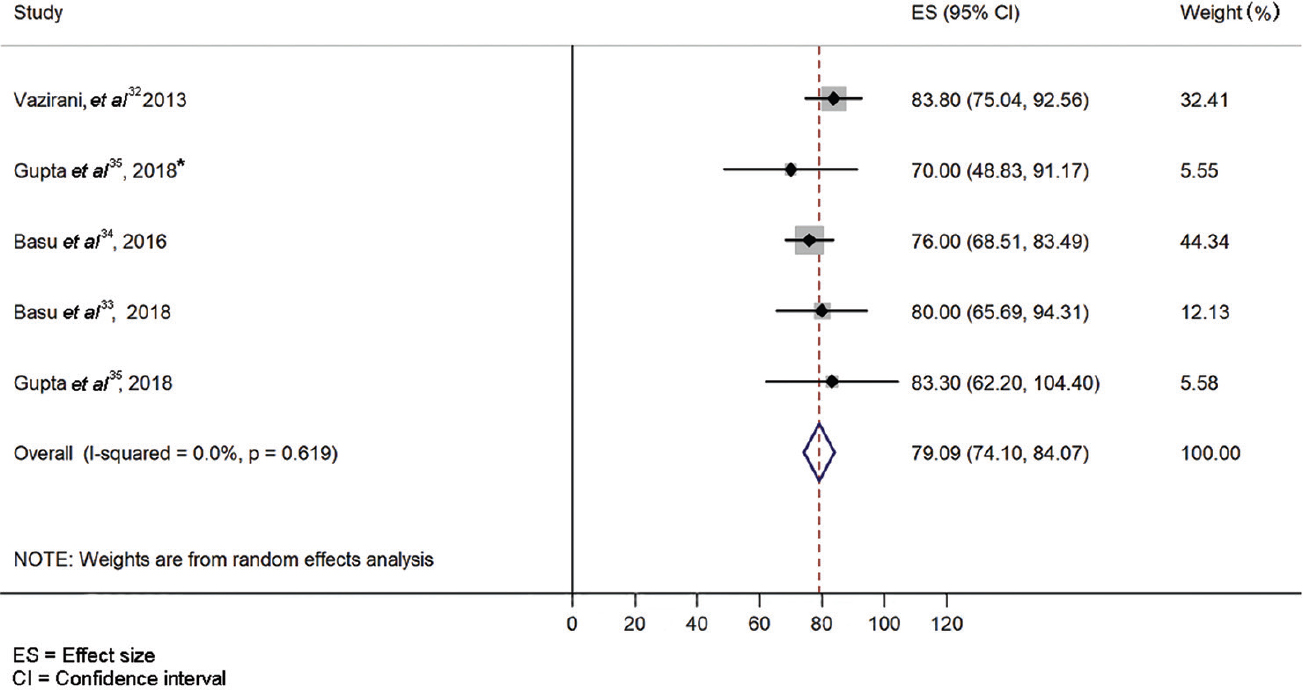
- Clinical outcome pooled estimate for simple limbal epithelial transplantation surgery.
Of the 17 studies, 10 were retrospective and nine were prospective. Among the analyzed studies, direct transplantation of the limbal lenticule either as an autologous tissue from the fellow eye (CLAU) or as an allograft from a cadaver/live donor (KLAL/CLAL) and combination of CLAU plus KLAL were done in one, three and one studies, respectively. The ex vivo expanded cultivated limbal epithelial transplantation (CLET) and SLET were done in six and four studies, respectively. One study each compared CLAL versus KLAL and CLET versus KLAL.
CLAU, CLAL and KLAL surgical outcomes: Direct limbal lenticule was transplanted in five studies1920212225, and one was a comparative study between CLAL and KLAL25. Transplantation of autologous lenticule tissue from the fellow eye (CLAU) was done in a study by Baradaran-Rafii et al19, an allograft from a live-related donor (CLAL) in study by Barreiro et al20 and Scocco et al21, an allograft from cadaver (KLAL) in a study by Baradaran-Rafii et al22 and combined CLAU plus KLAL intervention by Chan et al25.
Baradaran-Rafii et al19 evaluated surgical outcomes of CLAU in 34 patients having unilateral LSCD. Chemical injury was attributed as a cause of LSCD in 73.5 per cent of patients. The authors reported anatomical success, visual success and failure in 88, 88 and 11.8 per cent of the patients, respectively. Complications such as conjunctival encroachment on to the graft, graft dislodging due to small size, thick graft, graft oedema, ocular surface exposure, progressive horizontal conjunctivalization and pyogenic granuloma were reported during the post-operative period19.
Similar studies done by Barreiro et al20 and Scocco et al21 looked at surgical outcomes of CLAL in 34 and 32 patients, respectively. Barreiro et al20 included patients with unilateral and bilateral LSCD, and Scocco et al21 enrolled patients with bilateral LSCD alone. The major cause of LSCD in these studies was chemical injury (100%)20 and Steven–Johnson syndrome (43.7%)21, respectively. These two studies reported anatomical success, visual success and failure in 47.4, 82.1 and 52.6 per cent and 84.6, 46.2 and 15.4 per cent of the patients, respectively2021. Along with the assessment of surgical outcomes of CLAL, Barreirio et al20 compared the outcomes of conjunctival limbal transplantation with and without the use of amniotic membrane (AM) transplantation and documented similar results with both the procedures. In another study, no immunosuppressants were given and the limbal graft rejection was reported in 17.9 per cent of the cases21, whereas in study by the Barreiro et al20, immunosuppression was given in HLA-incompatible cases.
Baradaran-Rafii et al22 used cadaveric limbal allografts (KLAL) for transplantation in 45 patients with bilateral LSCD. Similar to the previously cited study21, chemical injury was the most common cause of LSCD (80% cases) and authors noted anatomical success, visual success and failure in 73.4, 84.8 and 26.6 per cent of patients, respectively22. In addition, adverse events such as immunologic rejections, graft-related complications and chronic ocular surface exposure were reported post-KLAL surgery. Chan et al25 evaluated outcomes of combined procedure of CLAU and KLAL. They included 11 patients with unilateral LSCD (attributed mainly to chemical injury, i.e. 54.5% patients) and documented anatomical success, visual success and failure in 82, 73 and 18 per cent of patients, respectively. Titiyal et al23 compared living-related CLAL with KLAL in a prospective interventional study. The study included 20 patients with unilateral LSCD (attributed to ocular burns) divided randomly into the two groups. At six months of follow up, the eyes that underwent CLAL as compared to those which underwent KLAL did significantly better in terms of visual gain (80 vs. 50%), ocular surface stability (70 vs. 20%), regression of conjunctivalization and corneal neovascularization. No complications were noted in either of the groups at the end of six months23.
Ex vivo expanded CLET: CLET was performed in six studies, of which two analyzed outcomes in patients with unilateral LSCD and four studies analyzed patients with both unilateral and bilateral LSCD262728293031. Vazirani et al26 looked at surgical outcomes of CLET in 70 patients with unilateral LSCD (40% post-chemical injury) and reported anatomical success, visual success and failure in 75, 66.6 and 25 per cent, respectively. This study compared the outcomes of autologous CLET also, either using the healthy part of the affected eye or the fellow eye as a source of limbal stem cells. The authors concluded that outcomes were similar and irrespective of the location of donor area26.
Sangwan et al27 evaluated post-CLET data of 200 patients with unilateral LSCD (81% post-chemical injury) and documented anatomical success, visual success and failure in 71, 60.5 and 29 per cent of patients, respectively. However, Prabhasawat et al28 and Rama et al29 reported anatomical success, visual success and failure in 77.9, 73.7, 26.3 per cent of patients and 89.7, 41.1 and 10.3 per cent of patients, respectively, of the total 18 and 112 patients with both unilateral and bilateral LSCD, respectively. The main aetiology for LSCD in these two studies noted was chemical injury; in 40 and 97.3 per cent of patients, respectively.
Shortt et al30 looked at surgical outcomes in 10 patients with both unilateral and bilateral LSCD and found anatomical success, visual success and failure in 60, 60 and 40 per cent of patients, respectively. Ramírez et al31 reported anatomical success, visual success and failure in 80, 50 and 20 per cent of patients, respectively, of a total of 19 patients with both unilateral and bilateral LSCD. In the study by Shortt et al30, chemical injury was the main cause of LSCD (40%), whereas in the study by Ramirez et al31, non-inflammatory conditions contributed maximally as a cause for LSCD (47.4%).
A prospective interventional study was conducted by Parihar et al24 which compared CLET with KLAL in 50 eyes of the 40 patients with bilateral LSCD. The most common indication for LSCD in their study was chemical and thermal burns (64%). They concluded that, at one year follow up, both the techniques were comparable. The complications reported included persistent epithelial defect, infective keratitis and primary graft rejection24.
Simple limbal epithelial transplant: There were four studies that evaluated the outcomes of SLET in cases of unilateral LSCD. Vazirani et al32 retrospectively evaluated and described the outcomes in 68 patients following SLET. The median follow up being 12 months, clinical success rate was 83.3 and in 65.7 per cent cases significant visual improvement was documented. Further supporting this study, a prospective interventional study by Basu et al33 suggested a success rate of 76 per cent and a failure rate of 18.4 per cent in post-SLET procedure. The median follow up was 18 months. Basu et al33 also supported the clinical success with histopathological evidence. The immunohistochemistry of the corneas post-SLET procedure was suggestive of corneal phenotype comparable to normal corneas. Basu et al34 evaluated the outcomes of SLET in failed CLET cases and showed successful outcomes in 80 per cent patients, observed over the period of 2.3 yr (mean follow up). Gupta et al35 published results of SLET in unilateral ocular surface burns in 30 patients. This study reported clinical success in 70 per cent patients. Visual acuity gain was seen in 71.4 per cent of cases. Conclusion of the study mentioned that autologous SLET was an effective limbal cell transplantation technique for the treatment of unilateral LSCD35. These studies revealed that following SLET, donor eye suffers minimal damage, the most common observation being a sub-conjunctival haemorrhage.
Cultivated oral mucosal epithelial transplantation: COMET promotes re-epithelialization and helps in reducing inflammation in patients with acute LSCD36373839. However, analysis of COMET studies was not performed as it is not purely an LSCT procedure. Sotozono et al36 reported the effectiveness and safety of COMET. This study concluded that substantial visual improvement was noted in patients with end-stage severe ocular surface disorders36. Hirayama et al37 compared the clinical results of COMET of substrate-free sheets with those of COMET with AM-based sheets and reported better outcomes with COMET of a substrate-free cell sheet in comparison to COMET with AM. Satake et al38 evaluated the long-term outcome of COMET for treatment of eyes with total LSCD and concluded that this surgery offered a viable and safe alternative in the reconstruction of a stable ocular surface with the additional advantage of a lower incidence of complications. Prabhasawat et al39 evaluated the outcomes of autologous COMET on human AM in 18 patients with bilateral severe LSCD. The authors concluded that COMET was instrumental in successful restoration of the ocular surface in majority of LSCD patients39.
Comparison of primary and secondary measures CLAL vs. CLET vs. KLAL vs. SLET: Overall, for the primary outcome (maintenance of a stable, epithelized, avascular cornea), there was no significant difference between any of the surgical procedures. However, the functional outcome in terms of gain in visual acuity post-operatively was better in KLAL group as compared to the CLET group (P=0.005) and SLET group as compared to CLET group (P<0.001). Hence, the anatomical success rates were almost identical between SLET, CLET, CLAL and KLAL procedures, while the functional success rates were better following KLAL and SLET procedures.
Discussion
The present review highlights that although a variety of surgical modalities for the management of LSCD exists, yet there is a lack of standard protocol for deciding a particular intervention over the other. Hence, this analysis was aimed to emphasize on the deficiency in the previous studies designs, including the use of heterogeneous study parameters, and to critically evaluate them. Further studies are needed to compare these surgical modalities in terms of their availability, efficacy, cost factor, technical difficulties and long-term results.
In the previous studies, surgical interventions were done at dissimilar stages of LSCD. Since the severity and stage of ocular surface disease were not comparable at the time of intervention, outcomes might be variable and non-comparable. This also suggests that the stage of LSCD at the time of intervention may be an important deciding factor for choosing any intervention. In the studies included, exact extent (in terms of clock hours) of LSCD was not mentioned, though division into partial and total LSCD was documented in a few studies. Pre-operative extent of LSCD is an important confounding factor for the surgical outcomes, which has not been taken into consideration in majority of the studies.
The percentage contribution of underlying aetiology to LSCD also varied between different studies, which could be another confounding factor while assessing surgical outcomes. Of the total 17 studies, ocular burn (chemical/thermal) was the main cause of LSCD in most of the studies. The response of ocular surface in terms of post-operative inflammation and rate of epithelization may vary depending upon the underlying cause for ocular LSCD.
Another important confounding factor was the wide variation in the number of previous surgical interventions before LSCT. In all 17 studies analyzed, the number of previous surgeries done in acute stage of the ocular insult varied considerably, which may be responsible for variable surgical outcomes even with the same surgical procedure. The success rates tend to drop with increasing number of surgical procedures. In the present review, no randomized controlled trial was found. All the studies were either prospective or retrospective with large variations in sample size, resulting in heterogeneity.
Among CLAU, CLAL, and KLAL studies, surgical outcomes of CLAU reported by Baradaran-Rafii et al22 was better than CLAL and KLAL. However, demographic details of all these studies were not comparable. Additional benefit mentioned for CLAU in this study was the non-requirement of systemic immunosuppression. Immunological rejection contributes significantly to post-operative complications following CLAL and KLAL, more so with KLAL. Thus, systemic immunosuppression becomes important which has its own adverse effects. It is known to decrease the systemic immunity and pre-dispose to infections and requires constant monitoring of the systemic status. Attributing to these reasons, this procedure is not popular despite acceptable surgical outcomes.
In CLET studies, documented surgical outcomes were nearly comparable between the studies and better than that of direct limbal lenticule transplant surgeries. Cultivation of limbal stem cells allows retrieving a smaller sample of limbal tissue from the donor eye as compared to the tissue size required for a direct transplant. The CLET procedure requires association with extensive and specialized clinical laboratory for cultivation of limbal stem cells retrieved from the donor eye. This, in turn, raises issues regarding the cost-effectiveness of CLET and occurrence of LSCD in the donor eye due to the procedure.
SLET has recently emerged as an effective modality for LSCD reported to have a favourable outcome in most studies43. The findings of this systematic review suggest that SLET and KLAL have significantly better functional success rates compared with CLET. The advantage of this procedure is that it requires harvesting of a smaller section of limbal tissue from donor eye and that there is no need for clinical laboratory and systemic immunosuppression. SLET has slowly gained popularity due to its advantage of being a single staged hassle-free treatment in unilateral LSCD. Limitation being bilateral cases, where other modalities such as CLAL or KLAL may be useful.
Although substantial evidence is lacking to support any one particular surgical technique, but studies are available which, despite their heterogeneity, allow assessment of results of different procedures for LSCT in terms of anatomical and functional outcome. This information along with clinical experience of the surgeon can help decide the appropriate intervention based on individual indications.
Future studies may be done taking into account these factors and then comparing the various procedures after standardizing factors, such as baseline inflammatory status of ocular surface, cause of LSCD, stage of LSCD and clock hours of involvement. Systematic data collection can help in better understanding of the outcomes based on stage of disease. Further, it can help formulate standardized intervention methodology for different stages of LSCD to ensure uniformity in outcomes.
Limitations of the review: Regulatory issues in different settings, varied age groups of recruited patients, different regions, difference in type, stage, severity of LSCD, duration between injury and surgery, different culture methods and difference in primary and subsequent intervention were confounding factors. Variable study designs of included studies and lack of any randomized controlled trial contributed to the lack of any concrete inference on this subject. Further studies with standardized methods and homogenous study design and patient population will help in filling the existing lacunae in the literature.
Conclusion
There is some evidence to suggest that although the anatomical success rates were almost identical between SLET, CLET, CLAL and KLAL procedures, yet the functional success rates were better following KLAL and SLET procedures as compared to CLET. Clinical judgement and experience of the surgeon is the underlying parameter for choosing a suitable intervention by considering patient factors and availability of resources.
Financial support & sponsorship: None.
Conflicts of Interest: None.
References
- Corneal re-epithelialization from the conjunctiva. Invest Ophthalmol Vis Sci. 1981;21:135-42.
- [Google Scholar]
- The corneoscleral limbus in human corneal epithelial wound healing. Am J Ophthalmol. 1990;110:646-56.
- [Google Scholar]
- Clinical patterns of corneal epithelial wound healing. Am J Ophthalmol. 1987;104:481-9.
- [Google Scholar]
- The conjunctiva in corneal epithelial wound healing. Br J Ophthalmol. 1998;82:1407-11.
- [Google Scholar]
- Reconstruction of the corneal epithelium by limbal allograft transplantation for severe ocular surface disorders. Ophthalmology. 1995;102:1486-96.
- [Google Scholar]
- Limbal autograft reconstruction after conjunctival squamous cell carcinoma. Am J Ophthalmol. 1990;110:412-5.
- [Google Scholar]
- Limbal cell autograft transplantation for severe ocular surface disorders. Graefes Arch Clin Exp Ophthalmol. 1998;236:582-7.
- [Google Scholar]
- Epithelial transplantation for the management of severe ocular surface disease. Trans Am Ophthalmol Soc. 1996;94:677-743.
- [Google Scholar]
- Surgical management of ocular surface disorders using conjunctival and stem cell allografts. Br J Ophthalmol. 1995;79:977-82.
- [Google Scholar]
- Limbal autograft transplantations for chronic ocular surface failures. Jpn J Clin Ophthalmol. 1993;47:607-10.
- [Google Scholar]
- Limbal autotransplantation in the acute and chronic phases of severe chemical injuries. Eye (Lond). 1996;10(Pt 3):349-54.
- [Google Scholar]
- Limbal autograft transplantation for ocular surface disorders. Ophthalmology. 1989;96:709-22.
- [Google Scholar]
- Surgical reconstruction of the ocular surface in advanced ocular cicatricial pemphigoid and Stevens-Johnson syndrome. Am J Ophthalmol. 1996;122:38-52.
- [Google Scholar]
- Combined penetrating keratoplasty and limbal allograft transplantation for severe corneal burns. Ophthalmic Surg Lasers. 1997;28:765-8.
- [Google Scholar]
- Limbal stem cell deficiency:Concept, aetiology, clinical presentation, diagnosis and management. Indian J Ophthalmol. 2000;48:83-92.
- [Google Scholar]
- Postoperative complications of conjunctival limbal autograft surgery. Cornea. 2012;31:893-9.
- [Google Scholar]
- Comparative study of conjunctival limbal transplantation not associated with the use of amniotic membrane transplantation for treatment of total limbal deficiency secondary to chemical injury. Cornea. 2014;33:716-20.
- [Google Scholar]
- HLA-matched living-related conjunctival limbal allograft for bilateral ocular surface disorders:Long-term results. Arq Bras Oftalmol. 2008;71:781-7.
- [Google Scholar]
- Live related versus cadaveric limbal allograft in limbal stem cell deficiency. Ocul Immunol Inflamm. 2015;23:232-9.
- [Google Scholar]
- Allogenic cultivated limbal stem cell transplantation versus cadaveric keratolimbal allograft in ocular surface disorder:1-year outcome. Int Ophthalmol. 2017;37:1323-31.
- [Google Scholar]
- The modified Cincinnati procedure:Combined conjunctival limbal autografts and keratolimbal allografts for severe unilateral ocular surface failure. Cornea. 2012;31:1264-72.
- [Google Scholar]
- Unilateral partial limbal stem cell deficiency:Contralateral versus ipsilateral autologous cultivated limbal epithelial transplantation. Am J Ophthalmol. 2014;157:584-90.e1.
- [Google Scholar]
- Clinical outcomes of xeno-free autologous cultivated limbal epithelial transplantation:A 10-year study. Br J Ophthalmol. 2011;95:1525-9.
- [Google Scholar]
- Efficacy of cultivated corneal epithelial stem cells for ocular surface reconstruction. Clin Ophthalmol. 2012;6:1483-92.
- [Google Scholar]
- Limbal stem-cell therapy and long-term corneal regeneration. N Engl J Med. 2010;363:147-55.
- [Google Scholar]
- Ex vivo expansion and transplantation of limbal epithelial stem cells. Ophthalmology. 2008;115:1989-97.
- [Google Scholar]
- Stem cell therapy for corneal epithelium regeneration following good manufacturing and clinical procedures. Biomed Res Int. 2015;2015:408495.
- [Google Scholar]
- Successful simple limbal epithelial transplantation (SLET) in lime injury-induced limbal stem cell deficiency with ocular surface granuloma. BMJ Case Rep. 2013;2013:bcr2013009405.
- [Google Scholar]
- Simple limbal epithelial transplantation:Long-term clinical outcomes in 125 cases of unilateral chronic ocular surface burns. Ophthalmology. 2016;123:1000-10.
- [Google Scholar]
- Simple limbal epithelial transplantation (SLET) in failed cultivated limbal epithelial transplantation (CLET) for unilateral chronic ocular burns. Br J Ophthalmol. 2018;102:1640-5.
- [Google Scholar]
- Results of simple limbal epithelial transplantation in unilateral ocular surface burn. Indian J Ophthalmol. 2018;66:45-52.
- [Google Scholar]
- Visual improvement after cultivated oral mucosal epithelial transplantation. Ophthalmology. 2013;120:193-200.
- [Google Scholar]
- Transplantation of cultivated oral mucosal epithelium prepared in fibrin-coated culture dishes. Invest Ophthalmol Vis Sci. 2012;53:1602-9.
- [Google Scholar]
- Long-term outcome of cultivated oral mucosal epithelial sheet transplantation in treatment of total limbal stem cell deficiency. Ophthalmology. 2011;118:1524-30.
- [Google Scholar]
- Long-term result of autologous cultivated oral mucosal epithelial transplantation for severe ocular surface disease. Cell Tissue Bank. 2016;17:491-503.
- [Google Scholar]
- Cultivated limbal and oral mucosal epithelial transplantation. Semin Ophthalmol. 2012;27:80-93.
- [Google Scholar]
- The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions:Explanation and elaboration. PLoS Med. 2009;6:e1000100.
- [Google Scholar]
- A systematic literature review of surgical interventions for limbal stem cell deficiency in humans. Am J Ophthalmol. 2008;146:251-9.
- [Google Scholar]
- Autologous limbal stem cell transplantation:A systematic review of clinical outcomes with different surgical techniques. Br J Ophthalmol. 2020;104:247-53.
- [Google Scholar]






