Translate this page into:
Outbreak prone communicable diseases of public health importance in the northern districts of West Bengal – Current status & the way forward
For correspondence: Dr Puran Kumar Sharma, Pasteur Institute, 2, Convent Lane, Kolkata 700 015, West Bengal, India e-mail: puran.sharma611@gmail.com
-
Received: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
India is perilously poised on the threshold of an explosion of infectious diseases, some of which have witnessed re-emergence while others await apposite opportunity to do so. The State of West Bengal is uniquely positioned with its innate geographical vulnerabilities that favour outbreaks of a host of infectious diseases. The northern districts of this State are well known endemic areas for many outbreak prone communicable diseases like malaria, Japanese encephalitis, scrub typhus, dengue and kala-azar. An outbreak of Nipah virus in the recent past is a pointer towards the emerging and re-emerging threat in these regions and warrants urgent prioritization for surveillance and monitoring of these diseases. Identification of risk factors, challenges in delivery of primary healthcare, implementation of intervention strategies along with strengthening of healthcare setup are also the need of the hour. Multisectoral initiatives with emphasis on understanding the complex and rapidly evolving human-animal-vector dynamics as envisaged under the ‘One Health’ concept are indubitably important pillars in the effective management of these emerging public health challenges.
Keywords
Dengue
emerging diseases
Japanese encephalitis
malaria
One Health
scrub typhus
surveillance
West Bengal
The rapid urbanization, deforestation and enhanced human forays into forested land for leisure/livelihood coupled with changing climatic patterns have all colluded to fatally influence the complex dynamics of vector-borne, zoonotic and other infectious diseases12. The fragile human-animal-vector interactions play a critical role in the spread of these infectious diseases into newer geographical expanses and also in the exponential rise in the number of outbreaks of these diseases12. The importance of ‘One Health’ concept cannot be more clearly deciphered and understood in the present context, with a large number of re-emerging vector-borne and zoonotic diseases, poised to radically impact human lives and challenge the already burdened public health system of India.
With its innate geographical vulnerabilities, the State of West Bengal is favourable for outbreaks of a large number of infectious diseases. The northern districts of West Bengal (Figure) mainly Alipurduar, Jalpaiguri, Cooch Behar and Darjeeling, are heavily forested, rich in wild life biodiversity and share international borders with countries like Bangladesh, Bhutan and Nepal and inter-State borders with Indian States like Bihar, Assam and Sikkim (which shares the international border with China and Bhutan) which are also well-known endemic areas for many outbreak prone communicable diseases34567891011. Jalpaiguri and Alipurduar districts of West Bengal are endemic for malaria with reports of outbreaks, deaths and drug resistant Plasmodium falciparum cases121314. The North Bengal districts are endemic for Japanese encephalitis (JE) too with reported outbreaks in 2011 and 20141516. Scrub typhus (ST) outbreak was reported for the first time in the State from Darjeeling district in 20041718. A dengue outbreak was also reported in Siliguri town of Darjeeling in the year 2005 and since then dengue has been endemic in the area19. In 2001 and 2007 Nipah virus (NiV) outbreaks took place at Siliguri in Darjeeling district and in Nadia district, respectively with similar outbreaks also reported from the neighbouring country, Bangladesh since 20012021. Kala-azar was restricted to two adjacent community development blocks in Darjeeling, which is in turn adjacent to Bihar State, Nepal and Bangladesh, all three of which are endemic for kala-azar22. These diseases pose an incessant public health challenge with recurrent surge in cases and threats of outbreaks.
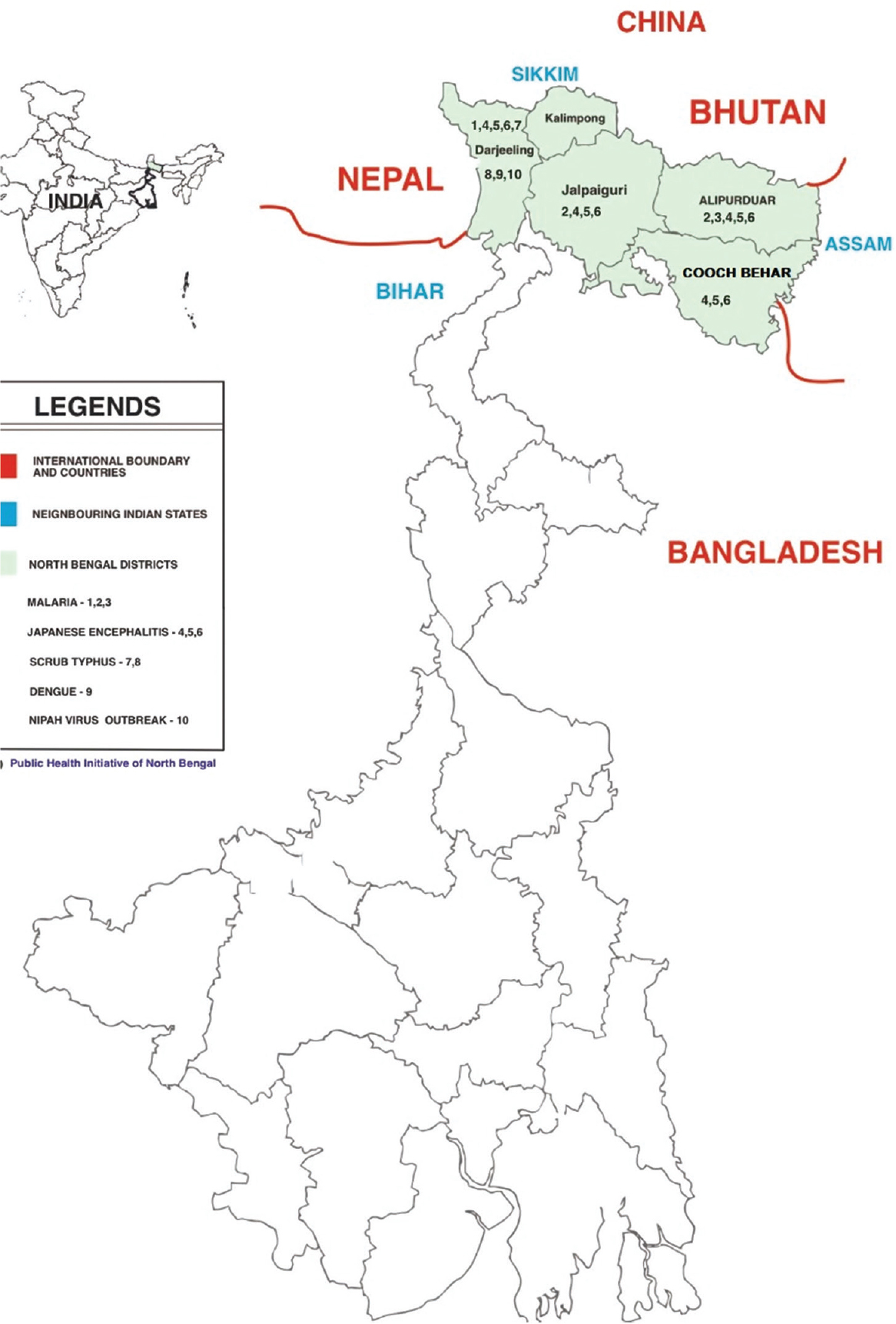
- Map of West Bengal State of India showing outbreak-prone northern districts. Source: Reproduced with permission (https://drive.google.com/file/d/1CcvTlnFnqFGjOyZGFaDqhJYqtHhDNq3V/view?usp=sharing).
Although malaria has been brought under control, it nonetheless is responsible for causing high morbidity and mortality in West Bengal. After the JE outbreaks in Jalpaiguri (including Alipurduar, which became a separate district in 2014) and Cooch Behar and Darjeeling in 2011 and in 2014, vaccination against JE was conducted in campaign mode for children and adults between 2012-2013 and 2015-2016 respectively and also introduced in the Routine Immunisation programme as per the Operational Guidelines under the National Programme for Prevention and Control of Japanese encephalitis/Acute Encephalitis Syndrome (2014)23. ST, a re-emerging disease in India, first reported from West Bengal in 2004 from Kurseong in Darjeeling district, has remained endemic since18. The area is now well recognized as a veritable hot spot of ST. Till date, the West Bengal State Health department has officially declared malaria (2018), JE (2017), dengue (2017) and kala-azar (2017) as notifiable diseases entailing their reporting by all government and private hospitals/laboratories, including non-governmental organization (NGO) run hospitals, as well as individual medical practitioners to strengthen capturing of surveillance data24.
The northern districts of West Bengal share porous international borders with Bhutan and Nepal and inter State borders (Figure);this coupled with the presence of a large number of army units in the region, ensures a steady perennial influx of large populations in the region. Additionally, Siliguri being the gateway to the North-Eastern States of India and a business hub also encourages enormous, movement/migration, thus setting the stage for outbreaks of many communicable diseases25. Thus, this review was undertaken to tabulate the status of outbreak prone communicable diseases in the region to highlight the issues at hand and emphasize the need for strategic planning of public health actions, which in turn would ease the burden of the emerging and re-emerging diseases.
Data Collection
Annual consolidated data on JE, scrub typhus and dengue for five North Bengal districts (Darjeeling, Kalimpong, Jalpaiguri, Alipurduar & Cooch Behar) and the State along with consolidated district data on malaria and kala-azar for the years 2018-20 were collected (personal communication). Data on malaria and dengue outbreaks from the five districts was also collected from published literature. Data on clinically suspected ST cases were collected from the treating physicians from two hospitals in Kurseong (personal communication) sub-division catering to areas of high risk for ST in Darjeeling district. Published literature online using medical journal search engines (PubMed and Google Scholar) on ST, malaria, dengue, JE, NiV and kala-azar disease burden for the year 2019 and reported outbreaks of these diseases in India, Bangladesh, Nepal and Bhutan since 2000 were searched. Entomological studies done in relation to these diseases, and abstracted information on reported outbreaks, hospital and community based serosurveillance data were also covered along with government documents related to disease control from the State health website.
Observations
Malaria: Malaria is endemic in India, Bangladesh, Nepal and Bhutan, with reported 3,38,494 [Plasmodium falciparum (Pf) cases 45.7% and 77 deaths)] 17,225 (Pf 85.6% and 9 deaths), 1,438 (Pf 0.6% and zero deaths) and 42 (Pf 9.5% and zero deaths) cases respectively in 20193. Bhutan and Nepal, which were among the 21 countries earmarked for elimination of malaria by 2020, reported one and 127 indigenous malaria cases respectively in 2019. West Bengal contributed to 7.5 per cent of the total malaria cases in the country and is one of the four high burden States for malaria in India where the High Burden High Impact (HBHI) approaches are to be implemented under NVBDCP (National Vector Borne Disease Control Programme)26. No spurt in the number of cases or outbreaks of malaria was reported from any district of the northern part of West Bengal during 2018-2020.
Dengue: Many outbreaks of dengue are reported from India, Bhutan, Bangladesh and Nepal since 20004561927. Dengue incidence in these four countries in 2019 was 1,36,422 (till November 2019), 1,01,000, 14,662 and 5935 respectively6272829.
A visible rise in dengue cases was reported across the State of West Bengal in 2019 (47,928), with Darjeeling district recording 1,244 cases in 2018 and 1,279 cases in 2019, with Cooch Behar and Alipurduar districts reporting 576 and 2,542 cases respectively in 2019 (unpublished data). There was an upsurge of cases in 2019 at Jaigaon town (Alipurduar) adjacent to Phuntsholing city (Bhutan), which experienced a huge outbreak in 20196. The West Bengal State Health department has, since 2017, enforced implementation of Integrated Vector Management strategies for prevention and control of dengue and strengthened Inter-sectoral coordination by actively roping in the urban local bodies (ULBs), department of Urban Development & Municipal Affairs, Panchayat & Rural Development, Animal Resource,School Education, Public Health Engineering, Women and Child Development and Social Welfare led by the District Magistrate at the district level24. Weekly house visits to check for vector breeding and fever surveillance followed by prompt treatment and vector control measures as applicable have been the key features for dengue prevention and control activities in the State24.
Other infectious diseases: India, Bangladesh, Nepal and Bhutan reported 2822, 97, 185 and 1 cases of kala-azar respectively in 201930. India and Bangladesh still have 90 and 16 endemic kala-azar blocks respectively while Nepal was able to achieve the elimination target in the 12 previously endemic blocks by 201331. Kala-azar is still endemic and confined in blocks of 54 districts of Bihar, Jharkhand, West Bengal and Uttar Pradesh, which contribute to a major chunk of the kala-azar load of the country32. However, no recent outbreaks of kala-azar have been reported from any of the two endemic blocks of Khoribari and Phansidewa in Darjeeling district, which are adjacent to the State of Bihar.
West Bengal witnessed outbreaks of NiV in 2001 (in Siliguri, Darjeeling district with 66 cases and case fatality ratio of 74%) and 2007 in Belechuapara village (in Nadia district with 5 cases and case fatality ratio of 100%) but none since then2021. NiV outbreaks were reported during the same years in Bangladesh too. Bangladesh, which shares international borders with many districts of West Bengal, has reported more than 16 outbreaks of NiV since its first report in 200121. There are reports of similarity in the strains of NiV involved in the outbreaks in West Bengal and Bangladesh, as well as, the geographical features of the two regions and the practice of consumption of date palm sap as a delicacy21. Similarities in clinical features of cases in both regions with evidence of human to human transmission too have been reported20. There are reports of presence of fruit eating bats (Pteropus giganticus) in both the regions with evidence of their being reservoirs of NiV and playing an important role in disease transmission with no role of pigs evidenced yet21. No reports of NiV were available from Nepal and Bhutan.
JE & acute encephalitis syndrome (AES): India, Bangladesh, Nepal and Bhutan reported 2496, 86, 71 and 0 cases of JE respectively in 201933343536. These countries are endemic and high risk for JE and have been reporting cases since many years7. Many outbreaks of JE have been reported from India and Nepal1137. JE vaccination has been incorporated in the routine immunisation programme in India only in select endemic States including West Bengal and in Nepal nationally7. Ten districts each of West Bengal including Darjeeling, Jalpaiguri (including the newly formed Alipurduar district) and Assam and 15 districts of Bihar are high priority districts for JE in India11. Outbreaks of JE have been reported in Bankura, Burdwan, Darjeeling and Jalpaiguri districts of West Bengal111516. The JE cases in the five districts and the State as a whole, however, show a declining trend from 2018 till 2020 (Table I).
| District/State | 2018 | 2019 | 2020 | |||
|---|---|---|---|---|---|---|
| # JE cases | # JE deaths | # JE cases | # JE deaths | # JE cases | # JE deaths | |
| Alipurduar | 10 | 3 | 6 | 2 | 3 | 1 |
| Jalpaiguri | 11 | 5 | 2 | 0 | 3 | 1 |
| Darjeeling | 7 | 2 | 2 | 0 | 3 | 1 |
| Cooch Behar | 20 | 9 | 4 | 2 | 1 | 0 |
| Kalimpong | 0 | 0 | 0 | 0 | 0 | 0 |
| Total | 48 | 19 | 14 | 4 | 10 | 3 |
| State | 140 | 35 | 82 | 12 | 41 | 4 |
Source: State Public Health wing of the Directorate of Health Services, Department of Health & Family Welfare, Government of West Bengal (personal communication)
Children and adults were vaccinated against JE in the years 2013-14 and 2015-2016 respectively. Routine JE vaccination for infants was also started from 2013-2014 in all the districts of North Bengal. Incidence of JE in Uttar Pradesh was also reported to have come down appreciably after the JE vaccination campaigns and introduction of JE vaccine under routine immunisation38; similar benefits are evident in this State as well.
Scrub typhus (ST): Numerous outbreaks of ST across India and two outbreaks each from Nepal and Bhutan were reported since 20009394041. Bangladesh is yet to report any outbreak of ST. Among India, Bangladesh, Nepal and Bhutan, only Bhutan has declared ST as a notifiable disease so far. Community and hospital based serosurveillance reports are available from these four countries providing evidence of endemicity of ST810424344. Similar reports are also available for Assam and Bihar4546.
West Bengal State Health Department commissioned 15 sentinel sites in March 2019 to screen all cases of AES and acute febrile illnesses (AFIs) using ST ELISA based IgM kits. Management protocols for ST were issued in September 20194748.
Studies from Gorakhpur (Uttar Pradesh) and Assam to determine non-JE aetiologies of AES found antibodies against Orientia tsutsugamushi in 62.7 per cent and 20.3 per cent of the cases respectively4345. The case fatality ratios (CFRs) in the studies from Assam and at North Bengal Medical College & Hospital, Siliguri, (NBMCH) in West Bengal, India showed high CFRs of 32.7 per cent and 49 per cent, respectively4549.
Another such study from the northern part of West Bengal, jointly conducted by the State Health department and National Institute of Mental Health & Neurosciences (NIMHANS) at NBMCH, Burdwan Medical College & Hospital (BMCH), Burdwan, and Bankura Sammeleni Medical College & Hospital (BSMCH), Bankura showed a seropositivity of 36 per cent50. Similar hospital based sero-surveillance studies for scrub typhus showed seropositivity against O. tsutsugamushi viz. Bangladesh (16.6%), Nepal (52.6%), Bhutan (22.6%), and in the Indian States of Assam (20.3%), Bihar (25%) and West Bengal (10.5%) (at NBMCH) among AFIs81044454649.
A community based study among febrile persons in Gorakhpur showed a seropositivity of 19.7 per cent against O. tsutsugamushi42 Reports on annual incidence of ST in the five North Bengal districts and the total incidence in the State were obtained from 2018 to 2020. Personal communications of the physicians at Mirik Rural and Kurseong sub-divisional hospitals in Darjeeling district on estimated incidence of clinical ST cases encountered and managed revealed more than 200 cases annually from 2018 to 2020. Data on ST obtained from the State Health Directorate for years 2018, 2019 and 2020 indicate a gradual increase in the number of ST cases in the district of North Bengal with more than six and four fold rise in total case load in the State in the years 2019 and 2020 respectively compared to the year 2018 (Table II). The estimated number of clinical ST cases encountered by the physicians at Mirik Rural and Kurseong sub-divisional hospital in Darjeeling district in the years 2018 to 2020 was more than 8 times than that reported by the district annually in those years.
| District | 2018 | 2019 | 2020 | |||
|---|---|---|---|---|---|---|
| # ST | # ST deaths | # ST | # ST deaths | # ST | # ST deaths | |
| Alipurduar | 15 | 2 | 13 | 0 | 17 | 0 |
| Cooch Behar | 5 | 1 | 28 | 1 | 17 | 1 |
| Darjeeling | 19 | 3 | 21 | 0 | 23 | 0 |
| Kalimpong | 0 | 0 | 1 | 0 | 3 | 0 |
| Jalpaiguri | 10 | 2 | 27 | 2 | 21 | 2 |
| Total | 49 | 8 | 90 | 3 | 81 | 3 |
| State | 579 | NA | 3148 | NA | 2002 | NA |
Source: State Public Health wing of the Directorate of Health Services, Department of Health & Family Welfare, Government of West Bengal (personal communication)
The presence of dedicated national programmes for prevention and control of malaria, JE, dengue and kala-azar as also the presence of orders of the West Bengal State Health department declaring them as notifiable diseases along with the presence of structured mechanisms for early detection, comprehensive data capture of cases and their timely management as per the laid down national protocols and State's initiatives have all led to better prevention and control of these enlisted diseases in the State24. However, there are certain concerns with regards to dengue and ST.
Though only two outbreaks of NiV have been encountered in West Bengal so far with 71 confirmed cases, the occurrence of numerous NiV outbreaks year after year in neighbouring Bangladesh, makes it imperative that surveillance for NiV infection be strengthened, sero-surveys be carried out in the bordering districts amongst the fruit eating bats and other potential vertebrate hosts in the region and spread awareness about the disease and safeguards while harvesting date palm saps.
The initiatives of the State have indubitably led to a decline in the number of JE cases in the North Bengal districts and the State as a whole. The decrease in JE is likely due to the JE vaccination campaigns and its introduction under routine immunisation, which has been seen in Uttar Pradesh (UP) as well38.
Scrub typhus has emerged as one of the major causes of morbidity and mortality in West Bengal49. Scrub typhus has re-emerged and is brazenly challenging the public health professionals with newer and varied clinical presentations, elusive epidemiology and its expansion and presence in areas not known for its endemicity51. The recent years has seen an increase in the number of cases of ST in the entire State including the North Bengal districts which possibly is due to enhanced awareness of ST as an important cause of AES and AFI among the medical practitioners52. The large number of reported outbreaks of AES and AFIs over the last decade, coupled with the increased access to testing facilities for ST in at least tertiary level hospitals has contributed substantially to an enhanced awareness amongst all stakeholders. Poor surveillance for ST with near absence of a system to send all clinical samples for testing are likely factors contributing to the morbidity and mortality caused by the disease especially in Kurseong sub-division of Darjeeling district. The woefully wanting situation has been additionally impacted by the ongoing COVID-19 pandemic, which has further crippled the situation. Delayed hospitalisation of ST cases with multiple organ dysfunctions due to diagnostic dilemmas or lack of clinical suspicion and high mortality of these cases have been widely reported4549.
There is only one epidemiological study reported from West Bengal which identified the local risk factors for ST and also recommended measures for prevention, including personal protection measures18. More such epidemiological, entomological, and sero-surveillance studies are required to identify the local risk factors, the predominant vertebrate hosts and vector mites and the endemicity of O. tsutsugamushi to help plan appropriate interventional strategies involving different non-health sectors including animal resource, agriculture, irrigation, forest, environment departments, etc. to control ST under the “One Health” concept. Enrolment of the Armed Forces for taking a lead in the effective management and establishment of a surveillance system in the affected area, at this crucial juncture, cannot be overemphasized. The Armed Forces Medical College (AFMC), Pune, India has been in the forefront of rickettsial research especially ST for the past 70 yrs with a live trombiculid mite colony to boast. Their expertise in training personnel for rickettsial survey, vector studies and identification, evaluation of various preventive modalities and outbreak investigations is well recognized. The enormous presence of Armed Forces in this border area exhorts their enhanced cooperation by sharing their expertise in formulation of area specific strategies, innovative preventive modalities and targeted recommendations for the effective containment of ST.
It is pertinent to highlight that a majority of the clinically suspected ST cases in the hospitals at Mirik and Kurseong did not have any laboratory confirmation to confidently assume that the recorded ST cases were true ST cases. However, as the hospitals at Mirik and Kurseong have been encountering cases of ST regularly since 2004, and the healthcare providers are well versed in detecting these cases with or without the pathognomonic eschar in the backdrop of negative tests for malaria, typhoid and dengue and the fact that all the suspected cases promptly responded to the empirical treatment with doxycycline/azithromycin as per the Government of India and State guidelines, left no room for doubt regarding the diagnosis of ST.
On the basis of extensive review of published literature, documents and records on ST and related topics, the following recommendations are put forth:
-
(i)
awareness to be increased on ST being an important cause for AES and AFI in the region and capacity building of the healthcare providers on early detection and management of ST; (ii) use of empirical treatment of clinically suspected ST cases with doxycycline/azithromycin, as applicable, to prevent delayed treatment and complications prior to laboratory confirmation; (iii) promotion of personal protective measures including avoiding woods/forests/shrubs, wearing protective clothing and gumboots to work, use of mite repellents and insecticide treated clothes during work, avoiding sitting on grass or shrubs, bathing after work and changing clothes, rearing cattle away from home, avoiding close contact with peri-domestic animals and strict avoidance of open-air defecation1842; (iv) Institution of rodent control measures and proper disposal of dead rodents17; (v) The State Health department may consider the following:
-
a)
providing facilities for Weil-Felix test (which is not cost intensive) for confirmation of ST in the primary and secondary tier hospitals in the high risk areas, which have no ELISA facility for IgM testing. This would help early confirmation of ST cases and early referral of complicated cases
-
b)
issuing of order declaring ST as a notifiable disease so that there is a comprehensive capture of data on ST to help understand the true burden of the disease and plan appropriate public health action
-
c)
strengthening disease surveillance (case based reporting, reporting of all cases – lab confirmed as well as clinically suspected cases and efforts to get all suspected cases tested for confirmation) in the region given its strategic location, the heavy population movement and it being a tourist destination, business hub and gateway to the North Eastern States of the country
-
d)
Undertaking epidemiological, entomological, and sero-surveillance studies in different parts of the State to identify the local risk factors, the predominant vertebrate hosts and vector mites and the endemicity of O. tsutsugamushi to help plan appropriate interventional strategies involving different non-health sectors to prevent and control ST42.
-
Conclusion
The northern districts of West Bengal are known endemic areas for many outbreak prone communicable diseases like malaria, JE, ST, dengue, and kala-azar. Amongst these, malaria, JE and kala-azar are well in control, whereas dengue and ST are showing an upward trend. The risk of NiV infection too remains and so heightened surveillance for it is required. Multi-sectoral initiatives with emphasis on understanding the complex and rapidly evolving human-animal-vector dynamics as envisaged under the ‘One Health’ concept are indubitably important pillars in the effective management of these emerging public health challenges and necessitate prioritization.
Acknowledgment:
The authors express their thanks to Dr Dipankar Maji, Joint Director of Health Services (Public Health Wing), Department of Health and Family Welfare, Government of West Bengal, for providing data on the different diseases, and the Public Health Initiative of North Bengal for permitting the use of the map of West Bengal showing the North Bengal districts prepared by them.
Financial support & sponsorship: None.
Conflicts of Interest: None.
References
- Outbreak of vector-borne and zoonotic diseases are associated with changes in forest cover and oil palm expansion at global scale. 2021. Front Vet Sci. Available from: https://www.who.int/influenza/resources/documents/tripartite_concept_note_hanoi/en/
- [Google Scholar]
- Emerging Zoonotic diseases originating in mammals: a systematic review of effects of anthropogenic land-use change. Mamm Rev. 2020;50:336-52.
- [Google Scholar]
- World Malaria Report 2020: 20 years of global progress and challenges. Geneva: WHO; 2020.
- The dengue epidemic in Bangladesh: Risk factors and actionable items. Lancet. 2019;394:2149-50.
- [Google Scholar]
- Epidemiological analysis of 2019 dengue epidemic in Bhutan. Int J Environ Res Public Health. 2021;18:354.
- [Google Scholar]
- Recent and historical trends in the epidemiology of Japanese encephalitis and its implementation for risk assessment in travelers. J Travel Med. 2018;25(Suppl 1):3-9.
- [Google Scholar]
- Rickettsial illnesses as important causes of febrile illness in Chittagong, Bangladesh. Emerg Infect Dis. 2018;24:638-49.
- [Google Scholar]
- Scrub typhus in Bhutan: A synthesis of data from 2009 to 2014. WHO South East Asia J Public Health. 2016;5:117-22.
- [Google Scholar]
- Scrub typhus: A serious public health issue in Nepal. Clin Epidemiol Glob Health. 2020;8:815-7.
- [Google Scholar]
- Japanese Encephalitis – Transmission Dynamics and Prevention and Control Strategy and Outbreak Investigations. Available from: https://www.who.int/docs/default-source/wrindia/japanese-encephalitis/japaneseencephalitis-transmission-control-investigation-prsentedby-dr-roop-webinar-ahcf-2020.pdf?sfvrsn=bb590015_2
- A malaria outbreak in Naxalbari, Darjeeling district, West Bengal, India, 2005: Weakness in disease control, important risk factors. Malar J. 2009;8:288.
- [Google Scholar]
- Incidence, management, and reporting of severe and fatal Plasmodium falciparum malaria in secondary and tertiary facilities of Alipurduar, India in 2009. J Vector Borne Dis. 2012;49:157-63.
- [Google Scholar]
- The shift from public to private health care providers and malaria deaths in Jalpaiguri district, West Bengal, India, 2006. Int Health. 2009;1:148-53.
- [Google Scholar]
- Entomological investigations into an epidemic of Japanese encephalitis (JE) in northern districts of West Bengal, India (2011-2012) Indian J Med Res. 2014;139:754-61.
- [Google Scholar]
- An outbreak of JE/AES in North Bengal districts of West Bengal during 2014. J Commun Dis. 2014;46:51-8.
- [Google Scholar]
- Emergence of Schoengastiella ligula as the vector of scrub typhus outbreak in Darjeeling: Has Leptotrombidium deliense been replaced? Indian J Public Health. 2011;55:92-9.
- [Google Scholar]
- Scrub typhus in Darjeeling, India: Opportunities for simple, practical prevention measures. Trans R Soc Trop Med Hyg. 2009;103:1153-8.
- [Google Scholar]
- Sero diagnosis of dengue activity in an unknown febrile outbreak at the Siliguri town, District Darjeeling, West Bengal. Asian Pac J Trop Med. 2010;3:364-6.
- [Google Scholar]
- Nipah virus-associated encephalitis outbreak, Siliguri, India. Emerg Infect Dis. 2006;12:235-40.
- [Google Scholar]
- Epidemiology of post-Kala-Azar dermal leishmaniasis. Indian J Dermatol. 2021;66:12-23.
- [Google Scholar]
- National Vector Borne Disease Control Programme. Operational guidelines: National Programme for Prevention and Control of Japanese Encephalitis/ Acute Encephalitis Syndrome. Available from: https://nvbdcp.gov.in/Doc/JEAES-Prevention-Control(NPPCJA).pdf
- 2018. Health & Family Welfare Department, Government of West Bengal. State Vector Borne Disease Control and Seasonal Influenza Plan. Available from: https://www.wbhealth. gov.in/uploaded_files/ticker/State_Vector_Borne_2018.pdf
- 2004. Globalisation and infectious diseases: A review of the linkages. World Health Organisation. Available from: https://apps.who.int/iris/handle/10665/68726
- High burden to high impact (HBHI) approaches – Country perspective for adoption and adaptation in India. India J Commun Dis. 2020;52:5-16.
- [Google Scholar]
- Dynamics of dengue outbreaks in Gangetic West Bengal: A trend and time series analysis. J Family Med Prim Care. 2020;9:56228.
- [Google Scholar]
- Dengue and Severe Dengue. Available from: https://www.who.int/news-room/fact-sheets/detail/dengue-and-severedengue
- Establishment & recent surge in spatio-temporal spread of dengue in Nepal. Emerg Microbes Infect. 2020;9:676-9.
- [Google Scholar]
- Number of Cases of Visceral Leishmaniasis Reported Data by Country. Available from: https://apps.who.int/gho/data/node.main.NTDLEISHVNUM?lang=en
- Towards elimination of visceral leishmaniasis in the India sub-continent-translating research to practice to public health. PLoS Negl Trop Dis. 2017;11:e0005889.
- [Google Scholar]
- Independent Assessment of Kala-Azar Elimination Programme India. New Delhi: WHO, Regional Office for South-East Asia; 2020.
- WHO Vaccine-Preventable Diseases: Monitoring System. 2020 Global Summary. Available from: https://apps.who.int/immunization_monitoring/globalsummary/countries?countrycriteria% 5Bcountry%5D%5B%5D=IND
- WHO Vaccine-Preventable Diseases: Monitoring System. 2020 Global Summary. Available from: https://apps.who.int/immunization_monitoring/globalsummary/countries?countrycriteria%5Bcountry%5D%5B%5D=BGD
- WHO Vaccine-Preventable Diseases: Monitoring System. 2020 Global Summary. Available from: https://apps.who.int/immunization_monitoring/globalsummary/countries?countrycriteria%5Bcountry%5D%5B%5D=BGD
- WHO Vaccine-Preventable Diseases: Monitoring System. 2020 Global Summary. Available from: https://apps.who.int/immunization_monitoring/globalsummary/countries?countrycriteria%5 Bcountry%5D%5B%5D=NPL
- Analysis of Japanese encephalitis outbreak in western Nepal in 1997. Epidemiol Infect. 2001;126:81-8.
- [Google Scholar]
- Decline in Japanese encephalitis, Kushinagar district, Uttar Pradesh, India. Emerg Infect Dis. 2014;20:1406-7.
- [Google Scholar]
- Rickettsial disease outbreaks in India: A review. Ann Trop Med Public Health. 2014;7:249-54.
- [Google Scholar]
- Scrub typhus and emerging public health threat in Eastern Nepal: An analysis from a tertiary centre during two years outbreak. Int J Contemp Pediatr. 2018;5:1715-8.
- [Google Scholar]
- An outbreak investigation in Nepal: Confirmation of local transmission. BMC Infect Dis. 2021;21:193.
- [Google Scholar]
- Seroprevalence & seroincidence of Orientia tsutsugamushi infection in Gorakhpur, Uttar Pradesh, India: A community-based serosurvey during lean (April-May) & epidemic (October-November) periods for acute encephalitis syndrome. Indian J Med Res. 2020;151:350-60.
- [Google Scholar]
- Acute encephalitis syndrome in Gorakhpur, Uttar Pradesh, India – Role of scrub typhus. J Infect. 2016;73:623-6.
- [Google Scholar]
- Seroprevalence of rickettsial infections and Q fever in Bhutan. PLoS Negl Trop Dis. 2017;11:e0066107.
- [Google Scholar]
- Scrub typhus leading to acute encephalitis syndrome, Assam, India. Emerg Infect Dis. 2017;23:148-9.
- [Google Scholar]
- Emergence of Orientia tsutsugamushi as an important cause of acute encephalitis syndrome in India. PLOS Negl Trop Dis. 2018;12:e0006346.
- [Google Scholar]
- 2019. Directorate of Health Services (Public Health Branch), Government of West Bengal. Guideline for testing for scrub typhus. Available from: https://www.wbhealth.gov.in/uploaded_files/IDSP/Scrub_Typhus_Guideline_for_testing_in_Acute_Fever_(2019).pdf
- 2019. Directorate of Health Services (Public Health Branch), Government of West Bengal. Protocol for management of scrub typhus. Available from: https://www.wbhealth.gov.in/uploaded_files/IDSP/Protocol_for_empirical_antibiotic_testing_Scrub_Typhus_(03.12_.2019).pdf
- Scrub typhus: A hospital-based study in the northern districts of West Bengal, India. Int J Res Med Sci. 2019;2:2403-7.
- [Google Scholar]
- 2017. Directorate of Health Services (Public Health Branch), Government of West Bengal. Addressing scrub typhus through case management of AES in West Bengal. Available from: https://www.wbhealth.gov.in/uploaded_files/IDSP/Addressing_Scrub_Typhus_through_case_management_of_AES_14.12_.2017_.pdf
- Clinical Manifestations and Complications of Scrub Typhus Cases: A Hospital-based Observational Study from Rural Part of West Bengal. Int J Med Public Health. 2020;10:180-3.
- [Google Scholar]






