Translate this page into:
Out-of-pocket payments & catastrophic healthcare expenditure for non-communicable diseases: Results of a State-wide STEPS survey in north India
For correspondence: Dr Pooja Kansra, Department of Economics, Lovely Professional University, Jalandhar 144 411, Punjab, India e-mail: pkansra@gmail.com
-
Received: ,
Accepted: ,
Abstract
Background & objectives
Non-communicable diseases have been designated as ‘public health priority’ globally, and they are accountable for debility, morbidity, and mortality. Thus, the present study aims to estimate the out-of-pocket payment, catastrophic healthcare expenditures and household wage loss.
Methods
Field research was conducted with an adapted survey questionnaire. Data from 576 individuals from various healthcare facilities in Punjab were collected using a convenience sampling approach. The out-of-pocket and catastrophic healthcare expenditures (CHE) were estimated using descriptive statistics and indices, viz., headcount overshoot and mean positive overshoot. Lastly, logistic regression models were applied to identify determinants of catastrophic health expenditure.
Results
The study findings showed that most respondents incurred a high out-of-pocket payment for inpatient care. Further, at any threshold level, the incidence of catastrophic health was highest among diabetic patients. The intensity of catastrophic healthcare expenditure with diabetes and hypertension exceeded the five per cent threshold bracket. Logistic regression results revealed that the odds of incurring catastrophic healthcare expenditure were highest among respondents diagnosed with diabetes, chronic obstructive pulmonary disease (COPD), and stroke.
Interpretation & conclusions
The study recommends that the government health insurance scheme ‘Ayushman Bharat-Mukh Mantri Sehat Bima Yojana (AB-MMSBY)’ must include outpatient and pre- and post-diagnostic costs incurred by respondents diagnosed with cardiovascular disease (CVD), COPD, and diabetes in Punjab. Therefore, respondents with diabetes mellitus (i.e., specifically type-1 patients) must be covered under health insurance benefits.
Keywords
Catastrophic healthcare expenditure
diabetes mellitus
healthcare utilisation
India
non-communicable diseases
out-of-pocket payments
Globally, non-communicable diseases (NCDs) are considered a ‘Public Health Priority’, being accountable for huge mortality and morbidity1,2. The burden of NCDs is expected to increase globally due to rapid environmental changes, rising global populace, demographic transitions, and lifestyle modifications3. People above 60 yr of age are the most affected by NCDs, and the number is projected to double by 20504,5. With the commencement of the millennium, the entire world has been witnessing an increasing trend of NCDs, especially in industrially developed and developing economies5,6. Most NCDs are chronic and require expensive treatment regimens and prolonged healthcare utilization7. Globally, the economic burden of NCDs is enormous, and diseases like diabetes and cardiovascular conditions have been projected to reduce global GDP by five per cent8.
India’s epidemiological transition is driven by the fact that lives lost due to communicable, maternal, neonatal, and nutritional diseases (CMNNDs) reduced from 53.6 per cent in 1990 to 27.5 per cent. In contrast, NCDs accounted for 61.8 per cent of deaths in 20169. Among NCDs, the leading cause of mortality in India in 2016 was cardiac disease, followed by chronic respiratory diseases and cancer. Developing economies like India are, therefore, witnessing an alarming epidemic of NCDs10 because of risk factors related to behavioural, biological, environmental, and physical11 issues. Similarly, the proportion of disability-adjusted life years (DALYs) caused by NCDs has increased remarkably across India, from 30.5 per cent in 1990 to 55.4 per cent in 20169. Examining the transition in DALYs in India, it becomes evident that most NCDs witnessed an upsurge from 1990. According to Verma et al12, ‘NCDs in India account for an economic burden in the range of 5 to 10 per cent of the GDP, significantly slowing down the economic growth. Since India is confronted with the ‘triple burden’ of disease in conjunction with infectious disease and injuries, the burden posed by NCDs remains the Achilles heel for the underfunded health system’. NCDs like diabetes, hypertension, heart disease, chronic obstructive pulmonary disease (COPD), and stroke were among the top five causes of DALYs in 201913. A breadth of literature on NCDs’ financial and socioeconomic impact and coping strategies is available at national, state, and district levels14-17. Still, literature in the context of Punjab is scant and mainly concentrates on prevalence, risk factors, and prevention strategies18-23. Thus, this study aims to estimate out-of-pocket payments, catastrophic healthcare expenditures, and household wage loss.
Materials & Methods
This cross-sectional study was conducted by the department of Economics, Lovely Professional University, Punjab, India.
Study design
A descriptive, cross-sectional research design was adopted for the present study conducted in the North Indian State of Punjab. Data from 576 individuals were collected using a convenience sampling approach through a survey questionnaire from healthcare facilities like public hospitals, private hospitals, etc., from March 6 to September 21, 2023. The out-of-pocket expenses were quantified for both outpatient and inpatient care, as shown in figure. The occurrence of outpatient care was assessed using a two-month recall at the time of the survey. In contrast, the occurrence of inpatient care was evaluated within a one-yr reference period at the time of the survey.
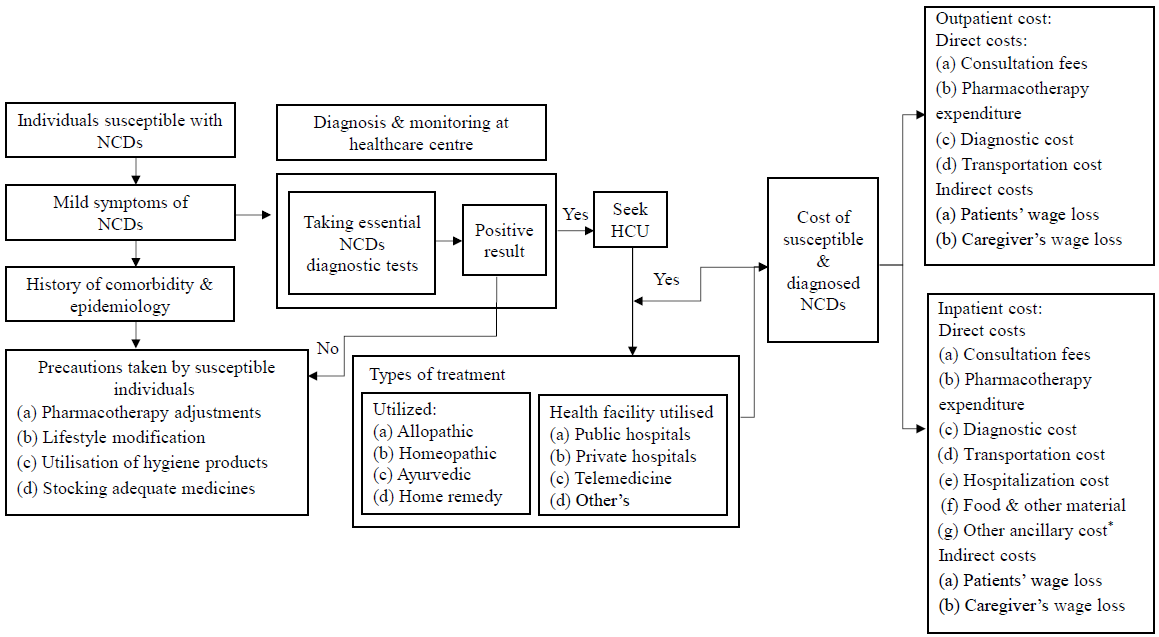
- Framework on the healthcare utilisation and economic enquiry of NCDs. HCU, healthcare utilisation; NCDs, non-communicable diseases. *Multiple responses are possible.
The rationale of the study
According to the Indian Council of Medical Research9, Punjab’s affluence and consuming habits make it the State with the highest rates of obesity and hypertension. The proportion of NCDs to the total disease burden is 52.1 per cent in Punjab. Moreover, Punjab witnessed a drastic shift in Disability-Adjusted life years (DALYs) from 1990 to 2016. NCDs such as ischaemic heart disease, chronic obstructive pulmonary disease (COPD), and diabetes are among the top three leading causes of fatality and debility in Punjab9, with a mean percentage change of 17.1, 4, and 3.9 per cent, respectively, in 2016.
Study variables
The method adopted by us identified direct and indirect costs and their total expenditure as essential components for assessing the economic burden of NCDs. Direct costs consist of expenses related to resource usage because they originate from diagnosis and treatment followed by healthcare procedures24. Direct costs are derived from medical and non-medical costs; their sum calculation produces the total direct cost. Direct medical expenses consist of payment for physician appointments, testing fees, drug prescriptions, and their required supplies. Hospitalisation costs, costs of patient transport to medical facilities, and expenditures on food items and materials make up direct non-medical expenses16,25.
The loss of worker productivity affects patients with illness and their household members who function as caregivers, resulting in indirect costs. Wage loss data was documented by combining outpatient and inpatient appointment attendance periods through interview responses from patients and their acquaintances17. The human capital approach26,27, served as the methodology followed throughout this investigation. Health expenses become catastrophic whenever individuals spend more on out-of-pocket medical costs than a predetermined share of their annual spending. This study investigated threshold levels of 5, 10, 20, and 30 per cent relating to the incidence and intensity of total household expenditures.
Developing research instrument
This study used a self-administered research instrument adapted from the ‘WHO STEP wise Surveillance’ manual. Before the primary survey, a four-stage procedure was followed to develop and adapt measures regarding scale development21; (i) designing the instrument, (ii) modifications in research items, (iii) psychometric trait testing, and (iv) reliability test. Demographic characteristics are presented in the first section, followed by section two, which discusses the type of NCD the respondents were diagnosed with. Lastly, section 3 focuses on both inpatient and outpatient costs associated with NCDs.
Statistical analysis
Descriptive analyses were performed in the present study to estimate the socio-demographic characteristics and out-of-pocket payments. Mean, median, and range were calculated for costs by the components of direct and indirect costs. Moreover, catastrophic healthcare expenditure (CHE) was measured to estimate the incidence and intensity of healthcare expenditures28. The headcount and overshoot method was employed to assess the incidence of NCDs29,30, and mean positive overshoot was used to assess the intensity of healthcare expenditures29. The headcount ratio and overshoot technique collectively offer significant insights into the cost of illness (COI) research, facilitating a thorough comprehension of both the prevalence and severity of the economic burden resulting from disease. The headcount ratio offers breadth by indicating who and how many individuals are affected, whereas the overshoot method provides depth by assessing the severity of their impact. Together, these methods create a comprehensive framework for understanding and addressing the economic burdens of illness. The mean positive overshoot technique enhances the study by quantifying the average economic distress of individuals over a cost threshold, thereby guiding targeted interventions, reducing disparities, and offering a more thorough assessment of illness-related financial burdens. Finally, a logistic regression model was used to assess the influence of several independent factors provided concurrently to predict membership in one of the two dependent variable categories31.
Where, E = Indicator equal to one, if Oi/Yi>z or else Zero; Pi = Out-of-Pocket expenditure of household; Yi = Household income; Z = Catastrophic threshold level; N = Sample size.
Where,
Results
Socio-demographic profile
Table I highlights the socio-demographic profile of the study respondents from Punjab. Of the 576 respondents, a sizable proportion diagnosed with NCDs was male. The majority of the NCDs were identified as lifestyle diseases, and most of the respondents were from urban regions. The analysis revealed that a sizable proportion of respondents diagnosed with any NCD were from the age groups of 41-60 yr and above 60 yr. Moreover, a history of NCDs in the family was reported by 54 per cent of the respondents. Among diverse types of NCDs, a large proportion of respondents were diagnosed with diabetes (31%), followed by hypertension (24%), CVD (19%), stroke (15%), and COPD (11%).
| Characteristics | (N=576), n (%) |
|---|---|
| Gender | |
| Male | 380 (66) |
| Female | 196 (34) |
| Residence | |
| Urban | 357 (62) |
| Rural | 218 (38) |
| Marital status | |
| Bachelor | 75 (13) |
| Married | 301 (87) |
| Age group (yr) | |
| Up to 20 | 17 (03) |
| 21-40 | 75 (13) |
| 41-60 | 288 (50) |
| 60 and above | 196 (34) |
| Work status | |
| Salaried | 63 (11) |
| Business | 219 (38) |
| Student | 23 (04) |
| Homemaker | 173 (30) |
| Retired | 52 (09) |
| Other | 46 (08) |
| Education level | |
| Illiterate | 35 (06) |
| Primary | 173 (28) |
| Secondary | 179 (33) |
| Graduate | 150 (26) |
| Post-graduate & above | 41 (07) |
| Stated monthly income | |
| Less than ₹15,000 | 86 (15) |
| ₹ 15,000 - ₹ 30,000 | 184 (32) |
| ₹ 30,000 - ₹ 45,000 | 138 (24) |
| ₹ 45,000 - ₹ 60,000 | 81 (14) |
| ₹ 60,000 and above | 86 (15) |
| Family type | |
| Nuclear | 271 (47) |
| Extended | 305 (53) |
| History of NCDs in family | |
| Yes | 351 (61) |
| No | 225 (39) |
| Type of non-communicable disease | |
| Hypertension | 138 (24) |
| Diabetes | 179 (31) |
| Cardiovascular disease (CVD) | 109 (19) |
| Chronic obstructive pulmonary disease (COPD) | 63 (11) |
| Stroke | 86 (15) |
Source: Calculation based on our survey data
Healthcare utilisation of non-communicable disease in Punjab
Table II elucidates the healthcare utilisation of NCDs in Punjab. It was found that a large proportion of respondents used allopathic treatment (76%), followed by home remedies (18%), ayurveda (5%), and homoeopathy (1%). The study results revealed that 48 per cent of respondents utilised private healthcare facilities, 26 per cent utilised public healthcare facilities, 19 per cent preferred chemists, and seven per cent utilised homoeopathy care. Lastly, of all the 576 respondents, a substantial proportion of 259 individuals own private insurance, followed by 34 per cent with governmental (AB-MMSBY) insurance, and 21 per cent do not know about the health insurance they possess. The mean distance covered to access healthcare facilities was 5.49 km.
| Healthcare utilisation | n (%) |
|---|---|
| Treatment taken | |
| Allopathic | 438 (76) |
| Ayurveda | 103 (18) |
| Home remedies | 29 (05) |
| Homoeopathy | 06 (01) |
| Type of health facility utilised | |
| Public hospitals | 150 (26) |
| Private hospitals | 276 (48) |
| Homeopathy clinic | 41 (07) |
| Chemists | 109 (19) |
| Type of insurance owned | |
| Government (AB-MMSBY) | 196 (34) |
| Private insurance | 259 (45) |
| No insurance | 121 (21) |
| Distance covered to visit health facility | |
| Mean (±Standard Deviation) distance in km | 05.49 (±3.5) km |
Source: Calculation based on our survey data
Annual outpatient and inpatient costs of NCDs by component of direct and indirect costs
The results of the annual outpatient and inpatient cost of NCDs by components have been shown in table III. Respondents with cardiovascular disease incurred the highest mean direct outpatient cost of ₹48,000 (3800 - 90,000) and mean indirect cost of ₹6000 (500 - 7500). It was found that respondents with stroke experienced the second-highest mean direct outpatient cost of ₹40,300 (4000 - 85,000). In contrast, respondents with COPD incurred the second-highest mean indirect cost (₹4909). The results revealed that patients with hypertension incurred the least direct and indirect outpatient costs. Expenditure on medicines constituted the most significant cost element among all NCDs, succeeded by expenses related to diagnostics, consultation fees, and transportation costs.
| Types of cost component | Type of non-communicable diseases | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Hypertension | Diabetes | CVD | COPD | Stroke | ||||||
| Outpatient cost of NCDs (n=576) | Mean | Median (Range) | Mean |
Median (Range) |
Mean |
Median (Range) |
Mean |
Median (Range) |
Mean |
Median (Range) |
| Consultation fee | 2400 |
2304 (3000-10) |
3600 |
3215 (4500-10) |
4500 |
4400 (7200-350) |
3600 |
3450 (6000-150) |
3500 |
3400 (7000-250) |
| Expenditure on medicines | 12000 |
12128 (17550-1050) |
24000 |
23000 (30000-1800) |
36000 |
33000 (45500-3600) |
27797 |
24000 (60000-2500) |
28,000 |
27500 (80000-4000) |
| Diagnostic expenditure | 3600 |
3520 (6000-800) |
6000 |
5850 (12500-1400) |
9600 |
9000 (25000-1800) |
8003 |
8015 (18500-2400) |
7500 |
7200 (15500-3600) |
| Transportation cost | 600 |
500 (1000-200) |
1200 |
800 (2000-200) |
1300 |
1200 (2000-150) |
1254 |
1150 (2000-250) |
1300 |
1100 (2500-500) |
| Total direct cost | ₹15840 |
14000 (30000-2000) |
₹30000 |
25500 (47550-2500) |
₹48000 |
45000 (90000-3800) |
₹35250 |
33750 (58500-3200) |
₹40,300 |
40000 (85000-4000) |
| Mean wage loss to the patient | 2400 |
2200 (3500-500) |
4200 |
4000 (7000-500) |
4800 |
4720 (12500-500) |
4250 |
4000 (7800-500) |
3750 |
3500 (10000-500) |
| Mean wage loss of the caregiver | 3000 |
2750 (4000-500) |
4800 |
4250 (6000-450) |
6000 |
5500 (7500-500) |
5110 |
4560 (9000-1000) |
2300 |
2200 (8000-1000) |
| Total indirect cost | ₹2400 |
4850 (7200-500) |
₹4200 |
3800 (6000-450) |
₹6000 |
5850 (7500-500) |
₹4909 |
4764 (8500-500) |
₹3500 |
3300 (5500-500) |
| Inpatient cost of NCDs in the past365 days (n=209) | ||||||||||
| Consultation fee | 1200 |
1100 (2500-10) |
1751 |
1700 (3500-10) |
2000 |
1700 (4500-150) |
2500 |
2280 (7000-250) |
3000 |
2500 (6000-400) |
| Expenditure on medicine | 4000 |
3600 (20000-800) |
5516 |
4408 (25000-800) |
6000 |
5510 (15500-1200) |
7200 |
6500 (14000-1000) |
5400 |
4850 (20000-1000) |
| Cost of hospitalisation | 3500 |
2800 (7500-250) |
5784 |
5500 (15000-500) |
2550 |
2100 (5500-250) |
7850 |
7000 (20000-800) |
3500 |
3200 (10500-500) |
| Diagnostic expenditure | 4000 |
3300 (10500-350) |
5478 |
4840 (10500-600) |
4500 |
4550 (10500-700) |
7000 |
6600 (15000-1000) |
5200 |
4945 (17500-800) |
| Transportation cost | 375 |
250 (1200-100) |
684 |
500 (1800-100) |
400 |
350 (1500-200) |
500 |
400 (1500-100) |
550 |
350 (1500-200) |
| Food & other material | 2000 |
1800 (5000-250) |
2632 |
2400 (4800-250) |
2500 |
2000 (4500-300) |
3000 |
2500 (5000-500) |
2500 |
2200 (4500-400) |
| Other ancillary cost* | 18000 |
14500 (35000-2000) |
27900 |
25000 (42000-2500) |
80000 |
66000 (150000-2500) |
43250 |
32000 (95000-3000) |
20000 |
15500 (55000-2000) |
| Total direct cost | ₹33075 |
28500 (38000-2000) |
₹35970 |
34500 (65000-2500) |
₹90000 |
72500 (150000-2500) |
₹50000 |
41000 (105000-3000) |
₹25,000 |
22000 (58500-2000) |
| Mean wage loss to the patient | 1200 |
1050 (3000-500) |
3000 |
2800 (6500-750) |
3172 |
2845 (12500-500) |
4150 |
3750 (10000-500) |
2700 |
2500 (9500-500) |
| Mean wage loss of the caregiver | 1500 |
1400 (4000-450) |
2500 |
2200 (4800-450) |
3837 |
3550 (6000-500) |
3200 |
3000 (5000-500) |
2100 |
2050 (6000-500) |
| Total indirect cost | ₹2700 |
2300 (6000-450) |
₹3000 |
2800 (6000-450) |
₹4277 |
4200 (12500-500) |
₹5000 |
4500 (10000-500) |
₹2600 |
2400 (9500-500) |
Source: Calculation based on our survey data
The analysis revealed that of the total 576 study respondents, only 209 utilised inpatient healthcare. The mean direct inpatient cost incurred by cardiovascular disease respondents was the highest at ₹90,000 (2500 - 1,50,000), followed by COPD, hypertension, stroke, and diabetes, as exhibited in table III. Under indirect inpatient cost, respondents with COPD incurred the highest mean cost of ₹5000 (500 - 10000), followed by cardiovascular disease, diabetes, stroke, and hypertension.
Incidence and intensity of catastrophic healthcare expenditure (CHE) across various NCDs
The incidence and intensity of CHE across various NCDs in Punjab have been presented in table IV. At any threshold level, CHE incidence (headcount) was the highest among diabetic patients. The respondents with COPD experienced a minor incidence of CHE at 20 and 30 per cent threshold levels. The intensity (overshoot) of CHE with diabetes and hypertension was above eight per cent at the threshold level of five per cent, whereas respondents diagnosed with stroke experienced the least intensity (overshoot) of CHE at any given threshold level (i.e., from 5 to 30%). The analysis revealed that respondents diagnosed with hypertension suffered the second highest ‘overshoot’ and highest ‘mean positive overshoot’ intensity at five per cent and 10 per cent threshold levels, respectively. Similarly, respondents diagnosed with stroke experience the second-highest intensity (mean positive overshoot) of 11.43 per cent at a threshold level of five per cent.
| Types of NCDs | Measures of catastrophic health expenditure | Threshold levels for CHE (%) | |||
|---|---|---|---|---|---|
| 5% | 10% | 20% | 30% | ||
| Hypertension | Headcount | 65.74 | 45.24 | 17.27 | 11.69 |
| Overshoot | 08.32 | 06.37 | 03.55 | 1.09 | |
| Mean positive overshoot | 12.65 | 14.08 | 15.59 | 09.32 | |
| Diabetes mellitus | Headcount | 85.37 | 65.71 | 22.76 | 12.71 |
| Overshoot | 08.96 | 05.25 | 01.8 | 00.75 | |
| Mean positive overshoot | 10.49 | 08.01 | 10.4 | 11.2 | |
| Cardiovascular disease | Headcount | 80.56 | 50.97 | 14.03 | 5 |
| Overshoot | 07.77 | 04.32 | 01.38 | 00.53 | |
| Mean positive overshoot | 09.65 | 08.48 | 9.87 | 10.58 | |
| Chronic obstructive pulmonary disease | Headcount | 74.17 | 38.82 | 9.54 | 02.63 |
| Overshoot | 5.97 | 3.04 | 0.81 | 00.22 | |
| Mean positive overshoot | 8.05 | 07.83 | 08.52 | 08.38 | |
| Stroke | Headcount | 45.57 | 37.19 | 18.1 | 08.76 |
| Overshoot | 5.21 | 3.13 | 1.12 | 0.12 | |
| Mean positive overshoot | 11.43 | 08.41 | 6.18 | 1.36 | |
Source: Calculation based on our survey data
Determinants of catastrophic healthcare expenditure of NCDs in Punjab
The critical determinants of CHEs of NCDs were identified with logistic regression, as shown in table V. Based on the ‘Omnibus Test of Model’, the value of 0.000 exhibits the models as statistically significant. Hosmer and Lemeshow’s goodness of fit test shows that the model is an excellent fit for the data as the P value is more significant than 0.05. At a 30 per cent threshold level, respondents diagnosed with NCDs observed a statistically significant association with CHE and major socio-demographic variables such as gender, age, income, work status, education, and complications. As shown in table V, the probability of CHE was higher among male respondents diagnosed with hypertension, diabetes, and cardiovascular disease.
| Sociodemographic variables | Catastrophic healthcare expenditure at 30 per cent threshold level | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Hypertension | Diabetes | CVD | COPD | Stroke | ||||||
| Odd ratios | P value | Odd ratios | P value | Odd ratios | P value | Odd ratios | P value | Odd ratios | P-value | |
| Gender (females) | ||||||||||
| Male | 2.574 | 0.046* | 1.197 | 0.572 | 2.551 | 0.015* | 0.333 | 0.063 | 0.058 | 0.055 |
| Age (below 20 yr) | ||||||||||
| 21-40 | 3.379 | 0.120 | 1.344 | 0.826 | 0.489 | 0.453 | 0.732 | 0.693 | 1.274 | 0.515 |
| 41-60 | 2.771 | 0.034* | 1.647 | 0.125 | 0.716 | 0.009* | 1.292 | 0.684 | 1.421 | 0.539 |
| 60 and above | 0.989 | 0.960 | 1.49 | 0.036* | 0.643 | 0.114 | 1.695 | 0.422 | 1.467 | 0.016* |
| Education (illiterate) | ||||||||||
| Primary | 2.212 | 0.875 | 0.150 | 0.108 | 0.614 | 0.703 | 2.662 | 0.510 | 0.291 | 0.269 |
| Secondary | 0.635 | 0.690 | 0.185 | 0.135 | 0.657 | 0.023* | 0.579 | 0.394 | 0.298 | 0.274 |
| Graduation | 0.981 | 0.987 | 0.160 | 0.103 | 0.751 | 0.807 | 0.598 | 0.432 | 0.360 | 0.359 |
| Post-graduation | 0.907 | 0.031* | 0.187 | 0.135 | 0.586 | 0.648 | 0.375 | 0.359 | 0.686 | 0.773 |
| Others | 1.075 | 0.569 | 0.227 | 0.202 | 0.310 | 0.384 | 0.272 | 0.406 | 0.434 | 0.999 |
| Work status (salaried) | ||||||||||
| Business | 1.759 | 0.274 | 1.966 | 0.107 | 0.967 | 0.957 | 0.903 | 0.848 | 0.473 | 0.001* |
| Student | 1.379 | 0.409 | 1.047 | 0.894 | 0.857 | 0.765 | 1.803 | 0.366 | 0.552 | 0.56 |
| Homemaker | 0.714 | 0.999 | 13.441 | 0.022* | 15.413 | 0.002* | 0.362 | 0.108 | 0.055 | 0.023* |
| Retired | 0.958 | 0.943 | 1.096 | 0.834 | 0.47 | 0.205 | 0.951 | 0.944 | 0.561 | 0.426 |
| Others | 3.561 | 0.02* | 1.699 | 0.221 | 0.986 | 0.983 | 1.151 | 0.866 | 0.277 | 0.165 |
| Income (less than ₹15,000) | ||||||||||
| ₹15,000 - ₹30,000 | 2.448 | 0.045* | 3.939 | 0* | 9.164 | 0* | 1.391 | 0.027* | 1.183 | 0.041* |
| ₹30,000 - ₹45,000 | 1.998 | 0.055 | 2.463 | 0.001* | 4.824 | 0.004* | 0.335 | 0.020* | 0.618 | 0.376 |
| ₹45,000 - ₹60,000 | 1.079 | 0.829 | 1.876 | 0.027* | 3.513 | 0.021* | 0.192 | 0.003* | 0.614 | 0.388 |
| ₹60,000 & above | 0.922 | 0.827 | 1.235 | 0.485 | 1.458 | 0.545 | 0.077 | 0.000* | 0.845 | 0.776 |
| History of NCDs (No) | ||||||||||
| Yes | 0.935 | 0.748 | 0.874 | 0.426 | 0.856 | 0.536 | 0.810 | 0.048* | 0.738 | 0.271 |
| Complications (No) | ||||||||||
| Yes | 0.461 | 0.000* | 2.417 | 0.000* | 0.495 | 0.008* | 1.518 | 0.173 | 2.525 | 0.001* |
| Household size (Nuclear) | ||||||||||
| 4-6 members | 0.711 | 0.44 | 1.399 | 0.349 | 1.82 | 0.223 | 0.590 | 0.209 | 0.516 | 0.228 |
| 6members and above | 0.999 | 0.997 | 0.949 | 0.815 | 0.973 | 0.937 | 0.808 | 0.712 | 0.494 | 0.276 |
| Model summary | ||||||||||
| Omnibus test of model | Sig. = 0.000 | Sig. = 0.000 | Sig. = 0.000 | Sig. = 0.000 | Sig. = 0.000 | |||||
| Hosmer & Lemeshow test |
Chi-square = 4.137; Sig.= 0.845 |
Chi-square = 6.246; Sig.= 0.620 |
Chi-square = 11.125; Sig.= 0.195 |
Chi-square = 7.192; Sig.=0.516 | Chi-Square = 12.15; Sig.=0.145 | |||||
| Nagelkerke (R2) | 0.162 | 0.168 | 0.209 | 0.216 | 0.194 | |||||
Source: Calculation based on our survey data
On the contrary, the odds of incurring CHE were lower among male respondents diagnosed with COPD and stroke. The odds of incurring CHE were two times higher among the respondents diagnosed with hypertension and COPD and having a primary level of education in Punjab. It was found that the odds of incurring CHE were thirteen times higher among diabetic homemakers as compared to other respondents diagnosed with hypertension, stroke, CVD, and COPD. The analysis revealed that respondents with low-income levels were likelier to experience CHE at any given type of NCD than respondents with high income. The logistic regression results revealed that the probability of incurring CHE was higher among respondents diagnosed with diabetes, COPD, and stroke as the major NCD complications. Lastly, the odds of incurring CHE were high among diabetic and CVD respondents with a household size of 4-6 members.
Discussion
The prevalence of NCDs stands as the foremost contributor to mortality, disability, and overall health deterioration. Without the implementation of immediate and widespread interventions across the nation, this burden is poised to escalate significantly. NCDs account for 63 per cent of India’s total disease burden, leading to a rise in overall mortality32. The socio-demographic profile in the study has highlighted that the incidence of NCDs was higher among urban respondents aged 41 to 60 yr. Moreover, the results of the present study are analogous to the evidence from prior literature demonstrating that households with low levels of income experienced a higher intensity of CHE compared to affluent counterparts33-35. India’s out-of-pocket payments are profusely higher than in other developing economies, owing to the paucity of health insurance coverage and lack of social security schemes36. Many out-of-pocket expenditures on NCDs in India are associated with direct costs such as medical expenditures and diagnostic procedures.
The results of the present study elucidate that there exists increasing health and financial insecurity in Punjab because of out-of-pocket healthcare expenditures, like the available literature12,37. The logistic regression results are analogous to available literature,38-41 revealing socioeconomic variables, such as region, gender, age, work status, income, and complications as significantly associated with CHE. Hence, providing financial protection to households with low socioeconomic status in Punjab is imperative. Therefore, the present study highlights the need for robust government policies to create awareness about the social consequences of NCDs in Punjab. This study’s strengths include enhancing the sparse literature on CHE, particularly in Punjab, and establishing a basis for focused health interventions. The logistic regression analysis provides a rigorous framework for identifying socioeconomic determinants of CHE, revealing critical patterns across gender, income, and household demographics. However, the study encounters various limitations, such as the cross-sectional approach constraining the establishment of the causation between study variables and limiting the understanding of the temporal evolution of health expenditures. Moreover, the findings of the study lack generalisability to other states and the entire State of Punjab because of distinctive demography and socioeconomic characteristics. Lastly, future studies may mitigate these constraints using longitudinal data and methodologies to achieve a comprehensive view.
Additionally, promoting a healthy diet and physical activity among the youths of Punjab, who are highly disposed to NCDs and are the national front-runners in risk factors like obesity, dyslipidaemia, and hypertension. The study further proposed that the government health insurance scheme ‘Ayushman Bharat-Mukh Mantri Sehat Bima Yojana’ must include outpatient and pre-and post-diagnostic charges incurred by respondents diagnosed with CVD, COPD, and diabetes in Punjab. Lastly, the healthcare system in Punjab requires a substantial transition away from its traditional emphasis on infectious diseases and maternity and child health to address primary and secondary prevention, along with diagnosis and treatment and bring affordable medications for diabetes mellitus and other NCDs within reach.
Overall, the study highlights the substantial economic cost that NCDs impose on households in Punjab. Out-of-pocket expenses have resulted in CHE, exhibiting a robust link between socioeconomic characteristics and the occurrence of CHE. Study reveals that households with lower income and specific demographics, such as larger household sizes or persons with lower educational attainment, are especially susceptible. Respondents with CVD incurred the highest direct (₹48,000) and indirect outpatient costs (₹6000). It was found that respondents with stroke experienced the second-highest direct outpatient cost (₹40,300), whereas respondents with COPS incurred the second-highest mean indirect cost (₹4909). The study recommends governmental strategies to bolster financial protection, avert impoverishment from NCD-related healthcare expenses, and promote early identification and treatment coverage to alleviate financial distress.
Financial support & sponsorship
None.
Conflicts of Interest
None.
Use of Artificial Intelligence (AI)-Assisted Technology for manuscript preparation
The authors confirm that there was no use of AI-assisted technology for assisting in the writing of the manuscript and no images were manipulated using AI.
References
- Burden of non-communicable diseases and its associated economic costs in India. Soc Sci Humanit Open. 2022;5:100256.
- [CrossRef] [Google Scholar]
- The economic burden of non-communicable diseases on households and their coping mechanisms: Evidence from rural Vietnam. World Dev. 2022;151:105758.
- [CrossRef] [Google Scholar]
- The rising burden of non-communicable diseases in the Americas and the impact of population ageing: a secondary analysis of available data. Lancet Reg Health Am. 2023;21:100483.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The global impact of non-communicable diseases on healthcare spending and national income: A systematic review. Eur J Epidemiol. 2015;30:251-77.
- [CrossRef] [PubMed] [Google Scholar]
- Preventing noncommunicable diseases (NCDs) by reducing environmental risk factors. Available from: https://www.who.int/publications/i/item/WHO-FWC-EPE-17.01, accessed on October 24, 2023.
- Burden of non-communicable disease: Global overview. Diabetes Metab Syndr. 2010;4:41-7.
- [CrossRef] [Google Scholar]
- Action to address the household economic burden of non-communicable diseases. Lancet. 2018;391:2047-58.
- [CrossRef] [PubMed] [Google Scholar]
- Noncommunicable diseases risk factor surveillance: Experience and challenge from India. Indian J Community Med. 2011;36:S50-6.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- India: health of the nation’s states-The India state-level disease burden initiative. Available from: https://www.healthdata.org/sites/default/files/files/policy_report/2017/India_Health_of_the_Nation%27s_States_Report_2017.pdf, accessed on July10, 2023.
- The economic cost of rising non-communicable diseases in India: A systematic literature review of methods and estimates. Appl Health Econ Health Policy. 2023;21:719-30.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Noncommunicable diseases in India: Challenges and the way forward. J Postgrad Med. 2019;65:5-6.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Assessing the household economic burden of non-communicable diseases in India: Evidence from repeated cross-sectional surveys. BMC Public Health. 2021;21:881.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Kumar V. 30% in Punjab have non-communicable diseases: Health department. The Times of India. 2019 Nov 25. Available from: https://timesofindia.indiatimes.com/city/chandigarh/30-in-punjab-have-non-communicable-diseases-health-dept/articleshow/72215015.cms, accessed on May 25,2022.
- Burden of non-communicable diseases and its associated economic costs in India. Soc Sci Humanit Open. 2022;5:100256.
- [CrossRef] [Google Scholar]
- Socioeconomic impact of hospitalisation expenditure for treatment of noncommunicable diseases in India: A repeated cross-sectional analysis of national sample survey data, 2004 to 2018. Value Health Reg Issues. 2021;24:199-213.
- [CrossRef] [PubMed] [Google Scholar]
- Cost of care for non-communicable diseases: Which types of healthcare providers are the most economical in India’s Chhattisgarh State? Pharmaco Economics Open. 2024;8:599-60.
- [Google Scholar]
- Out-of-pocket expenditure on non-communicable diseases during covid-19 A cross-sectional study from a semi-urban area of Kannur, Kerala. Clin Epidemiol Glob Health. 2023;19:101210.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Profile of risk factors for non-communicable diseases in Punjab, Northern India: Results of a state-wide STEPS survey. PLoS One. 2016;11:e0157705.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Burden and risk factors of dyslipidemia-results from a STEPS survey in Punjab India. Diabetes Metab Syndr. 2017;11:S21-7.
- [CrossRef] [PubMed] [Google Scholar]
- Structural equation modelling to identify the risk factors of diabetes in the adult population of north India. Trop Med Health. 2018;46:23.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Economic menace of diabetes in India: A systematic review. Int J Diabetes Dev Ctries. 2020;40:464-75.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Diabetes risk factors and prevention strategies: Awareness and perception of diabetics in Punjab. Econ Polit Wkly. 2021;56:60-4.
- [Google Scholar]
- Validation of diabetes-related awareness instrument (DRAI) to measure diabetics awareness towards risk factors and prevention strategies. IJQRM. 2022;39:1808-23.
- [CrossRef] [Google Scholar]
- Cost of diabetes and its complications: Results from a STEPS survey in Punjab, India. Glob Health Res Policy. 2023;8:11.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Cost of illness of non-communicable diseases in private and public health facilities in Nigeria: a qualitative and quantitative approach. Pan Afr Med J. 2023;44:6.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The value of human life revisited. Am J Public Health. 1982;72:536-8.
- [CrossRef] [PubMed] [Google Scholar]
- The economic costs of illness: A replication and update. Health Care Financ Rev. 1985;7:61-80.
- [PubMed] [PubMed Central] [Google Scholar]
- Out-of-pocket healthcare payments on chronic conditions impoverish urban poor in Bangalore, India. BMC Public Health. 2012;12:990.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Catastrophic payments and impoverishment due to out-of-pocket health spending. Econ Polit Wkly 2011:63-70.
- [Google Scholar]
- Catastrophic out-of-pocket payment for healthcare and implications for household coping strategies: evidence from West Bengal, India. Econ Bull. 2014;34:1303-16.
- [Google Scholar]
- Field A. Discovering statistics using IBM SPSS statistics. 4th ed. SAGE; 2013
- Burden of noncommunicable diseases in India: Setting priority for action. Int J Med Sci Public Health. 2013;2:7.
- [Google Scholar]
- Health-related financial catastrophe, inequality and chronic illness in Bangladesh. PLoS One. 2013;8:e56873.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Non communicable diseases. Available from: https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases, accessed on March 8, 2023.
- Inequalities in household catastrophic health expenditure and impoverishment associated with noncommunicable diseases in Chi Linh, Haiduong, Vietnam. Asia Pac J Public Health. 2017;29:35S-44.
- [CrossRef] [PubMed] [Google Scholar]
- Burden of healthcare utilisation and out-of-pocket costs among individuals with NCDs in an Indian setting. J Community Health. 2013;38:320-7.
- [PubMed] [Google Scholar]
- Measuring incidence of catastrophic out-of-pocket health expenditure: With application to India. Int J Health Care Finance Econ. 2012;12:63-85.
- [CrossRef] [PubMed] [Google Scholar]
- Refining estimates of catastrophic healthcare expenditure: An application in the Indian context. Int J Health Care Finance Econ. 2013;13:157-72.
- [CrossRef] [PubMed] [Google Scholar]
- Assessing the magnitude, distribution and determinants of catastrophic health expenditure in urban Lucknow, north India. Clin Epidemiology Glob Health. 2015;3:10-6.
- [CrossRef] [Google Scholar]
- Out-of-pocket expenditure and catastrophic health expenditure for hospitalisation due to injuries in public sector hospitals in north India. PLoS One. 2019;14:e0224721.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]






