Translate this page into:
Out-of-pocket expenditure due to hepatitis A disease: A study from Kollam district, Kerala, India
*For correspondence: epidklm@gmail.com
-
Received: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Several outbreaks of hepatitis A have been reported from Kerala, India, in the last 10 years1234. An average of 8268 [standard deviation (SD) 1767] cases suspected to have hepatitis A per year has been reported to the State's official disease surveillance system45. Most of the affected individuals were young adults between 15 and 35 yr age group. Many public health experts have opined that the Government should start thinking of hepatitis A vaccination in Kerala67. Cost is considered as a major concern by many for recommending hepatitis A vaccine in the State. Knowing the out-of-pocket expenditure due to hepatitis A will help the policymakers to decide on the vaccination policy in the State. The present study was done in Kollam district of Kerala in 2015 to estimate the out-of-pocket expenditure experienced by households due to hepatitis A disease.
Kollam district with a population of around 2.6 million has reported maximum number of hepatitis A cases in the State45. The female literacy rate for the district is 92 per cent8. Integrated disease surveillance programme (IDSP) has been performing reasonably well in the district with the help of a good primary health care team and notifications from major private hospitals. Apart from IDSP weekly reporting, the State also depends on a daily telephone-based reporting system, which collects information regarding communicable diseases from all the government hospitals on a daily basis. The District Surveillance Unit (DSU) prepares a line list of affected people for major communicable diseases based on information from daily and weekly reports. The district reported 584 cases of hepatitis A during 2015. Line list of people affected with hepatitis A notified to the DSU during August-October 2015 (n=114) was obtained.
All 114 individuals with confirmed hepatitis A were contacted with the help of primary health care team. Exploratory interview, using a pretested and validated questionnaire, was conducted during November 2015-January 2016, with the selected participants at their houses. Details of cost during hospitalization, consultation fees to doctors including traditional healers, amount spent on drugs including traditional medicines, laboratory investigations, additional amount spent for food and travel due to illness by the patient and relatives, informal tips, payment to caregivers, wages lost due to sickness for the patient and wage loss to any relative were collected in detail. Bills and medical records available with the patients were verified. The study was approved by Ethics committee of Center for Public Health Protection, Kollam (6/2015 dated 15.06.15).
For assessing the indirect cost, only the actual income loss to patient and relatives was considered. The productivity loss due to forgone non-market activities including school, household works and intangible cost was not converted to monitory terms. Data were analyzed using SPSS version 12 (SPSS, Chicago, IL, USA). Data were presented as a total and as an average with a SD in local currency, i.e., Indian Rupees ( ) and US dollars (US$) applying the exchange rate (US$1=
) and US dollars (US$) applying the exchange rate (US$1= 68).
68).
A total of 95 of 114 patients were interviewed. Others could not be contacted (n=6) or were not available at the address provided (n=13) during the data collection period. Among them, 40 per cent (n=38) were less than 15 yr, 47.4 per cent (n=45) were between 16 and 30 yr and 10.5 per cent (n=10) were between 31 and 45 yr. Males constituted 60 per cent (n=57). Of them, 60 per cent (n=57) were students, 16.8 per cent (n=16) were unskilled/semi-skilled labourers, 6.3 per cent (n=6) were homemakers, 4.2 per cent (n=4) were professionals/semi-professionals, 3.2 per cent (n=3) were skilled labourers and 2.1 (n=2) per cent were doing petty business. Further, 78.9 per cent (n=75) of the household interviewed possessed a below poverty line card.
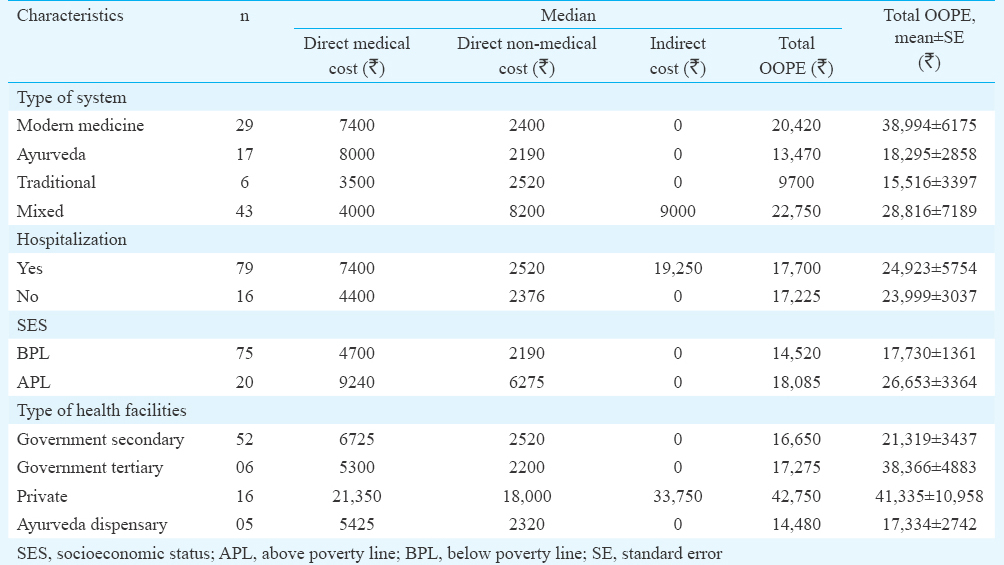
Of the 95 patients, 79 (83.2 %) had hospital admission, and 77.1 per cent (61/79) had admissions in government hospitals. The mean number of days admitted in hospital was 7.60 (standard error 0.92), median being four days. Of them (n=95), 30.6 per cent (n=29) consulted only modern medicine doctors, 18.9 per cent (n=18) consulted Ayurveda system, 6.3 per cent (n=6) visited traditional healers while 44.2 per cent (n=42) visited practitioners from more than one system. The median work days lost due to illness was 60 (range 21-180 days). The details of amount spent for each purpose and the total out-of-pocket expenditure (OOPE) are given in Table I. The mean direct medical cost, direct non-medical cost and indirect costs were  8446.2 (95% confidence interval (CI)
8446.2 (95% confidence interval (CI)  6726.1-10,166.3],
6726.1-10,166.3],  4438.1 (95% CI
4438.1 (95% CI  3502.1-5374.2) and
3502.1-5374.2) and  11890.5 (
11890.5 ( 6762.2-17,018.4), respectively. Total OOPE for the households due to one of its members affected with hepatitis A disease in Kollam district was
6762.2-17,018.4), respectively. Total OOPE for the households due to one of its members affected with hepatitis A disease in Kollam district was  24,774.8 (95% CI
24,774.8 (95% CI  19426.3- 30,123.2) (364 US$) with a median expenditure of
19426.3- 30,123.2) (364 US$) with a median expenditure of  17,700 (260 US$).
17,700 (260 US$).
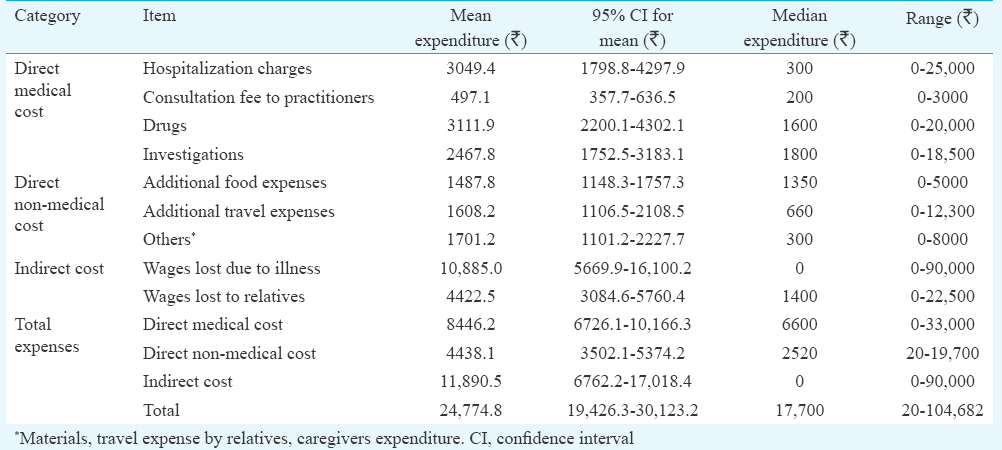
The details of OOPE by various categories are given in Table II. The OOPE due to hepatitis A disease was higher among those who sought care in modern medicine, especially from private sector.
In our study 34 per cent of total OOPE was found to be contributed by direct medical expenses while nearly 47 per cent was due to indirect expenditures. Majority of the patients were students and hence not working. The period of absence in schools and year lost due to missing examinations were not converted to monitory terms in the current study. Capturing the health system costs due to hepatitis A which includes service and material costs at government hospitals and cost of public health interventions to deal with hepatitis A cases will give the true picture of the economic loss due to hepatitis A disease. It should also be noted that the indirect costs of health care also contribute to the financial burden incurred by households. There could be some recall bias as data were collected after receiving treatment. However, to minimize the bias, we conducted all interviews between three and four months after initial diagnosis. Sample size was small limiting the ability to look at sub-groups and interactions. The official disease surveillance system has its own weaknesses that it may miss many hepatitis A cases.
The HAV antibody seroprevalence rates reported from Kerala was <10 per cent in children below five years when compared to 60-80 per cent from many other parts of the country91011. Among the Indian States, Kerala has the highest average out-of-pocket healthcare spending share and there is very little variation in this share across consumption expenditure quintiles12. We could not find any recent studies on OOPE due to hepatitis A from India; however, the OOPE in the current study seemed very high when compared with the same estimated by other studies for other communicable diseases such as tuberculosis under DOTS from Chennai and acute illness including hospitalizations from Puduchery1314. The OOPE for those who sought treatment from private sector was high in this study, and this result was consistent with other study reports from India15.
To conclude, the average household OOPE due to one of its members affected with hepatitis A disease in Kollam district was around  25,000. Directions for future research include assessing the real burden of hepatitis A and detailed economic analysis of universalizing HAV vaccination in the State.
25,000. Directions for future research include assessing the real burden of hepatitis A and detailed economic analysis of universalizing HAV vaccination in the State.
Acknowledgment
Authors acknowledge the District Surveillance Unit, Integrated Disease Surveillance Project, Kollam, and primary health care team of Kerala State Health Services, Kollam, for permissions and help.
Conflicts of Interest: None.
References
- Viral hepatitis surveillance - India, 2011-2013. MMWR Morb Mortal Wkly Rep. 2015;64:758-62.
- [Google Scholar]
- Molecular characterization of hepatitis A virus from a large outbreak from Kerala, India. Indian J Med Res. 2006;123:760-9.
- [Google Scholar]
- Investigating a community-wide outbreak of hepatitis A in India. J Glob Infect Dis. 2014;6:59-64.
- [Google Scholar]
- Directorate of Health Services. Data on Communicable Diseases. Thiruvananthapuram, Kerala: DHS. 2016. Available from: http://www.dhs.kerala.gov.in/index.php/publichealth
- [Google Scholar]
- Directorate of Health Services. Information Regarding Hepatitis A Data. Right to Information Act No.: PH4 1698/2016 DHS 13.1.16. Thiruvananthapuram, Kerala: DHS; 2016.
- [Google Scholar]
- Return of the water devil: Kerala need to be cautious about Hepatitis A outbreaks. Kerala Med J. 2015;4:14-6.
- [Google Scholar]
- Hepatitis Outbreaks Warrant New Strategies. The Hindu. 2014. Available from: http://www.thehindu.com/todays-paper/tp-national/tp-kerala/hepatitis-outbreaks-warrant-newstrategies/article5958446.ece
- [Google Scholar]
- Census 2011, Government of India. Kollam District: Census 2011 data. Available from: http://www.census2011.co.in/census/district/283-kollam.html
- [Google Scholar]
- Seroepidemiology of hepatitis A infection in India: Changing pattern. Indian J Gastroenterol. 2001;20:132-5.
- [Google Scholar]
- Seroprevalence of hepatitis A in children - Implications for hepatitis A vaccine. Trop Gastroenterol. 1998;19:120-1.
- [Google Scholar]
- Catastrophic payments and impoverishment due to out-of-pocket health spending. Econ Polit Wkly. 2011;46:63-70.
- [Google Scholar]
- Out of pocket expenditure among the households of a rural area in Puducherry, South India. J Nat Sci Biol Med. 2014;5:135-8.
- [Google Scholar]
- Expenditure pattern for TB treatment among patients registered in an urban government DOTS program in Chennai city, South India. Tuberc Res Treat. 2012;2012:747924.
- [Google Scholar]
- Economic and disease burden of dengue illness in India. Am J Trop Med Hyg. 2014;91:1235-42.
- [Google Scholar]





