Translate this page into:
Ocular graft versus host disease in allogenic haematopoetic stem cell transplantation in a tertiary care centre in India
Reprint requests: Dr Murugesan Vanathi, Cornea & Ocular Surface, Cataract & Refractive Surgery Services, Dr Rajendra Prasad Centre for Ophthalmic Sciences, All India Institute of Medical Sciences, New Delhi 110 029, India e-mail: vanathi_g@yahoo.com
-
Received: ,
This is an open access article distributed under the terms of the Creative Commons Attribution NonCommercial ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
This study was aimed to report the occurrence of ocular graft versus host disease (oGVHD) in allogeneic haematopoietic stem cell transplantation (allo-HSCT) patients in a tertiary care hospital setting.
Methods:
A cross-sectional study of ocular surface of allo-HSCT patients was done. Slit lamp biomicroscopy, symptom score, tear meniscus height, fluorescein tear break-up time, Schirmer's test I, ocular surface staining, dry eye severity, ocular surface disease index score were done. Indications for allo-HSCT, human leukocyte antigen (HLA) matching, GVHD risk factor, systemic manifestation and treatment were also noted.
Results:
GVHD occurred in 44.4 per cent of 54 allo-HSCT patients (mean age 26.7 ± 12 yr) included in the study. GVHD risk factors identified included female gender, relapse, older age of donor, cytomagelo virus (CMV) reactivation, and multiparous female donors. oGVHD was noted in 31.5 per cent with mean time to occurrence being 17.8 ± 21.9 months after the allo-HSCT and was observed in 89.5 per cent of chronic GVHD cases. Acute GVHD (oral and dermatological) involvement showed a significant association with GVHD in our patients (P< 0.001, 0R 23.0, CI 6.4-82.1). Chronic GVHD was observed to be associated with the occurrence of oGVHD (dry eye) (P<0.001, OR = 24.0, CI 0.02 - 0.29). Of the 34 eyes with oGHVD, dry eye of level 3 severity was seen in 16, level 2 in six, level 1 in 12 eyes.
Interpretation & conclusions:
GVHD occurred in 44.4 per cent of the patients studied in the present study. Acute and chronic GVHD showed a strong association with oGVHD. Dry eye disease due to chronic oGVHD was observed in 17 (31.5%) of 54 allo-HSCT patient with chronic oGVHD occurring in 17 (89.4%) of chronic GVHD cases in allo-HSCT patients. Our study on oGVHD in post allo-HSCT patients in tertiary care centre points towards the fact that ocular morbidity due to dry eye disease as a result of oGVHD is a cause for concern in these patients.
Keywords
Bone marrow transplant
dry eye
haematopoetic stem cell transplantation
oGVHD
peripheral blood stem cell transplant
The success of allogenic haematopoetic stem cell transplants (allo-HSCT) [peripheral blood stem cells transplantaion (PBSCT), bone marrow transplantation (BMT) and cord blood cells transplantation (CBT)] for various haematologic and non-haematologic disorders has resulted in improved early post-transplant survival. However, graft versus host disease (GVHD) continues to remain a cause of concern in these patients1. GVHD occurs due to the donor's immune system recognizing the recipient tissues as antigenic and, thereby resulting in inflammation and fibrosis.
The reported occurrence of oGVHD (oGVHD) in allo-HSCT2345 is 40-60 per cent and is responsible for ocular surface disease of varying severity that can result in a negative impact on the quality of life3. The incidence of acute and chronic GVHD has been found to be increasing with the use of peripheral-blood progenitor cells as a source of donor stem cells4.
GVHD was earlier recognized in two forms: an early acute form of GVHD and a delayed chronic form5. This clear distinction between acute and chronic GVHD now seems to be ill defined1567. The National Institutes of Health (NIH) consensus conference working Group5 described the categories of GVHD as acute GVHD category (either classic acute GVHD occurring within 100 days of allo-HSCT or persistent), recurrent, or late acute GVHD (features of acute GVHD occurring beyond 100 days, which commonly present during immunosuppressives withdrawal period), chronic GVHD category includes classic chronic GVHD (without features or characteristics of acute GVHD) and an overlap syndrome, which is characterized by diagnostic or distinctive features of chronic GVHD and acute GVHD occurring concurrently. Treatment options include lubricating eye drops, immunomodulator and steroid drops, and punctal occlusion5. Newer management options including molecular level therapies are currently being explored.
This study was undertaken to evaluate the occurrence of chronic oGVHD (dry eye disease) in Indian patients undergoing allo-HSCT in a tertiary care hospital setting.
Material & Methods
This cross-sectional study was undertaken on all consecutive haematological patients who had undergone allo-HSCT (for haematological malignant and non-malignant diseases) reporting to the post-transplant clinic of the haematological department of All India Institute of Medical Sciences (AIIMS), New Delhi, India, between November 2009 to November 2013. This was a one time study with criteria for recruitment into the study being all clinically stable patients above the age of five years, who had undergone allo-HSCT after a post-operative period greater than one month, with willingness to participate in the study. Patients with prior ocular surface morbidities (such as exposure keratitis, blink abnormalities) were not included in the study. Institutional Ethics Committee approval was obtained and written informed consent was taken from all patients.
Clinical data including demographic details, diagnosis, duration of disease, previous treatment, source of transplant, type of transplant, concurrent medications, donor characteristics [donor age and relation, human leukocyte antigen (HLA) matching, sex matching], GVHD risk factors [recipient /donor - age/sex, diagnosis, disease status, cytomegalo virus (CMV) status and conditioning regimens], immunosuppressant prophylaxis, antimicrobial therapy, occurrence of systemic acute / chronic GVHD (type), manifestations of chronic GVHD, were recorded at the time of recruitment. The diagnosis of systemic GVHD was made by the treating haematologist in accordance with the NIH consensus report5 and the cases were managed in conjunction with related specialist physician.
Ocular surface evaluation891011 was done one time at the point of recruitment and included visual acuity assessment, symptom score8, ocular surface disease index score (OSDI)9 slit lamp biomicroscopy, ocular surface evaluation tests (tear meniscus height (TMH), fluorescein tear break-up time (FTBUT), Schirmer's test I, Meibomian gland dysfunction, and ocular surface staining10. Symptoms grading8 was done as absent signs and symptoms - 0, mild irritation/discomfort - 1, moderate foreign body sensation with difficulty in opening eyes - 2, severe dry eye symptoms ± vascularisation and or keratinization - 3. The OSDI score was recorded using the 12-item questionnaire (based on 3 subscales of vision related function, ocular symptoms and environmental triggers) and graded as normal (0 - 12), mild (13 - 22), moderate (23-32), severe (33-100)9. The diagnosis of keratoconjunctivitis sicca was made based on FTBUT < 5 sec, Schirmer's I test < 5 mm in 5 min, ocular staining score ≥ 311. Dry eye severity classification and treatment protocols were in accordance to the Dry Eye Work Shop (DEWS) recommendations12. All data were recorded on a predesigned proforma.
Statistical analysis: Statistical analysis of data was done in Stata 11 software (Statacorp, USA) and unpaired t test was used. Odds ratio and GVHD risk factor analysis were done by logistic regression analysis with probability level for confidence interval being less than 5 per cent.
Results
Fifty four patients of allo-HSCT of mean age 26.7 ± 12 yr (range: 8 - 48 yr, 41 males 25.2 ± 10.8 yr, 13 females 30.9 ± 12.5 yr) were included in the study after a mean time of 11.1 ± 14.1 months (range: 1.1-78.7 months) after allo- HSCT, of whom 44.5 per cent (n = 24) were diagnosed to have GVHD. The parents of 12 paediatric patients did not consent to participate in the study. The most common indication for allo-HSCT was aplastic anaemia (n = 24, 44.5%) followed by chronic myeloid leukaemia (n=10, 18.5%), acute myeloid leukaemia (n=8, 14.8%), thallassaemia major (n = 3, 5.5%), acute lymphoblastic leukaemia (n = 4, 7.4%), myelodysplastic syndrome (n = 2, 3.7%), acute biphenotypic leukaemia (n = 1, 1.9%), and pure red cell aplasia (n = 2, 3.7%).
The most common preparative regimen included fludarabine 30 mg/m2 for six days, cyclophosphamide 60 mg/kg/day for two days and anti-thymocyte globulin 30 mg/kg/day for four days. The total CD 34+ve stem cell dose infused was 5.96 × 106/kg. GVHD prophylaxis included methotrexate 10 mg/m2 on day +1 and 7 mg/m2 on days +3 and +6 and cyclosporine 1.5 mg/kg twice daily intravenously, with plasma cyclosporine levels maintained between 150-300 ng/ml, for one year for allo-transplants for non-malignant diseases.
The BuCy protocol was used for conditioning prior to transplant in patients with haematological malignancies. BuCy consists of busulphan 3.2 mg/kg/day for four days and cyclophosphamide 60 mg/kg/day for two days. GVHD prophylaxis comprises methotrexate 15 mg/m2 on day + 1 (D+1), methotrexate 10 mg/m2 on D+3, D+6, and D+ 11 with folinic acid rescue, and cyclosporine 1.5 mg/kg twice daily intravenously. Systemic cyclosporine dose was adjusted as per plasma cyclosporine levels maintained between 150-300 ng/ml. It was continued for one year in patients with non malignant haematological disorders. Systemic cyclosporine was given for three months followed by taper over the next three months in patients with haematological malignancies. Acute systemic GVHD was initially managed with steroids. If refractory to steroids, then anti-thymocyte globulin was used. In case of chronic systemic GVHD, the patient received steroids.
Of the 24 patients with GVHD, 22 (40.7%, 22/54) were found to have acute GVHD [skin involvement in 13 patients (59.1%, 13/22), gastrointestinal tract in 14 patients (63.6%, 14/22) and hepatic in 4 patients (18.2%, 4/22)]. Chronic GVHD occurred in 19 patients (35.1%, 19/54), of whom (89.4%, 17/19) had chronic GVHD following acute GVHD, while (11.6%, 2/19) had chronic GVHD occurring de novo. Systemic involvement in chronic GVHD was ocular in 18 patients (92.3%), oral in 10 patients (53.8%), skin and hepatic in three patients (15.5%) each, respectively. Of the 41 male patients, 13 had chronic systemic GVHD, of whom 12 had oGVHD. Of the 13 female patients, six had chronic systemic GVHD, of whom five had oGVHD.
Of the ocular surface of all eyes (n = 108) evaluated, oGVHD (dry eye disease) was observed in 31.4 per cent (34 eyes of 17 patients). The mean time between the allo- HSCT and oGVHD occurrence was 17.9 ± 21.6 months (range: 1.3 to 78.7 months).
Of all the 54 allo-HSCT patients who had been HLA matched, 23 (42.6%) did not have any risk factors for GVHD while 31 patients (57.4%) had risk factors for GVHD development (gender mismatch, older multiparous female donor, in the remaining six patients-older age, gender mismatch, CMV reactivation, relapse of disease, multiparous female donor).
Risk factors noted in oGVHD patients were gender mismatch in nine patients; relapse, gender mismatch, CMV activation in one; age mismatch, gender mismatch in two; age mismatch; age mismatch with CMV activation; and multiparity, age mismatch, gender mismatch in one each; and no risk factors were observed in two patients. Of the 54 patients analysed, GVHD risk factors were identified in 31 patients which were significantly associated with the occurrence of oGVHD [OR = 6.667, CI 2.014 - 22.06,5 P=0.001] but not with the systemic GVHD [OR=2.00, CI 0.804-4.972, P=0.134]. Acute GVHD (oral and dermatological) involvement was seen to have a strong association with oGVHD in our patients (0R = 23.0, CI 6.4 - 82.1, P<0.001). Chronic systemic GVHD was observed to be significantly associated with the occurrence of oGVHD (dry eye) (P<0.001, OR = 24.0, CI 0.02 - 0.2).
Of the 108 eyes of 54 patients examined, 71.3 per cent (n = 77) had a Snellen's distance visual acuity of 6/6; 14.8 per cent (n=16) had 6/9; 6.5 per cent (n=7) had 6/12, 6.5 per cent (n=7) had 6/18; 0.9 per cent (n=1) had 6/24; and 0.9 per cent (n =1) had 6/60. The most common cause for decreased visual acuity was refractive error (n= 23), cataract (n=4), retinal haemorrhage (n=1), severe keratoconjunctivitis sicca (n=3) glaucoma (n=1), herpes zoster ophthalmicus (n=1), and cystoids macular oedema (n=1).
Out of 34 eyes with oGVHD, dry eye of level 3 severity was seen in 16, level 2 severity in six eyes, level 1 severity in 12 eyes, while none had level 4 severity. In eyes with oGVHD (n=34), the mean FTBUT was 11.8 ± 6.07 sec (range 0 - 26 sec), of which 82.3 per cent (n=28) had a FTBUT of >5 sec while 17.7 per cent (n=6) had ≤5 sec; mean conjunctival staining score with lissamine green was 1.8 ± 2.5 (range 0 - 10) and mean corneal staining score was 0.4 ± 1.7 (range 0-10); 75 per cent of eyes had a conjunctival score < 3 and 25 per cent ≥3; corneal staining score <3 was present in 93.5 per cent eyes whereas 6.5 per cent had score of ≥3; mean value of Schirmer 1 test in 5 min was 19.2 ± 11.8 mm (range 0-35 mm), of which 79.6 per cent (n=86) a value of >5 and 21.4 per cent (n=22) had ≤ 5; mean OSDI score was 13.7 ± 23.2 (range 0-87.5) being normal in 71.2 per cent (n=77), mild in 8.3 per cent (n=9), moderate in 13.8 per cent (n=15), and severe in 6.5 per cent (n=7).
Discussion
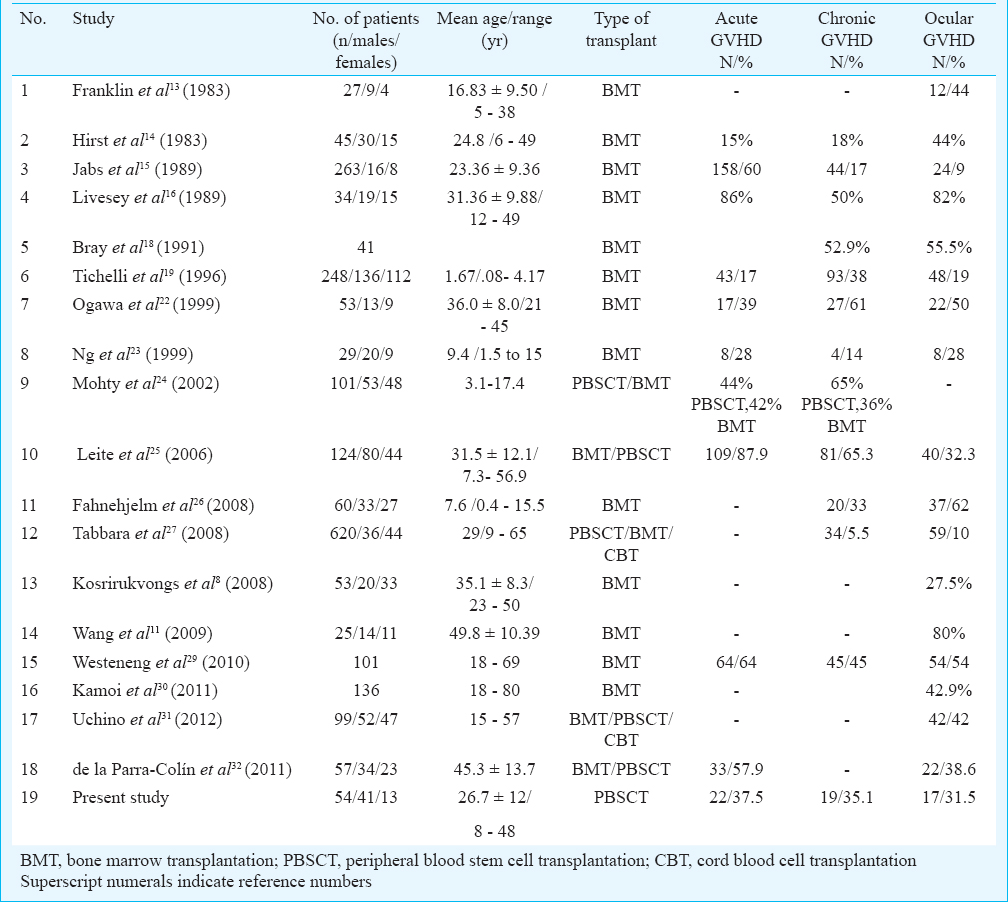
Literature on post-allogenic haematopoetic stem cell transplantation is replete with studies featuring from the early eighties, with most of them being related to bone marrow transplantation8111314151617181920212223242526272829303132 while the later ones24253132 report results following peripheral blood stem cell and cord blood transplantation. The prevalence of cGVHD in post BMT studies varied from 11.1 to 75 per cent8111314151617181920212223242526272829303132. Reported incidences of chronic GVHD in allogenic PBSCT patients ranges from 17 to 71 per cent24253132. oGVHD frequently accompanies chronic GVHD manifestations in other organs33. The reported prevalence of oGVHD ranges from 10 to 82 per cent (Table)13141516181922232425262729303132.
The extent of tissue involvement of the ocular surface tissues (lacrimal gland, lids, conjunctiva and cornea) and tear film determines the severity of the ocular surface disease morbidity. No significant difference has been seen in the cumulative incidence of chronic GVHD in post PBSCT or BMT recipients. However, chronic GVHD after PBSCT seems to be more prolonged and less responsive to treatment than chronic GVHD after BMT34. Variable prevalences of systemic GVHD after allogenic PBSCT and conventional BMT have been reported, with a higher risk of developing GVHD after allogenic PBSCT15. In our study GVHD risk factors were associated with the occurrence of oGVHD similar to the observation of Westeneng et al29. oGVHD occurrence was seen in 89.5 per cent of chronic GVHD cases in allogenic hematopoetic stem cell transplantation patients.
Our study is perhaps the first study in Indian patients from a tertiary care centre in north India, who have undergone allo-HSCT and establishes baseline data, which can help while planning more clinical and research studies in future.
Acknowledgment
Authors acknowledge the contributions of Ms Kalivani (Department of Biostatistics), further Prof. A. Panda (Dr R.P. Centre for Ophthalmic Sciences), Dr Lalit Kumar, Department of Oncology, All India Institute of Medical Sciences, New Delhi, for their contribution in this study.
Conflicts of Interest: None.
References
- Prevalence and risk factors associated with development of ocular GVHD defined by NIH consensus criteria. Bone Marrow Transplant. 2012;47:1470-3.
- [Google Scholar]
- Current insights into ocular graft-versus-host disease. Curr Opin Ophthalmol. 2010;21:485-94.
- [Google Scholar]
- Acute and chronic graft-versus-host disease after allogeneic peripheral- blood stem-cell and bone marrow transplantation: a meta-analysis. J Clin Oncol. 2001;19:3685-91.
- [Google Scholar]
- National Institutes of Health consensus development project on criteria for clinical trials in chronic graft - versus - host disease: I. Diagnosis and staging working group report. Biol Blood Marrow Transplant. 2005;11:945-56.
- [Google Scholar]
- Prognostic relevance of ‘early-onset’ graft-versus-host disease following non-myeloablative haematopoietic cell transplantation. Br J Haematol. 2005;129:381-91.
- [Google Scholar]
- Dry eye as a major complication associated with chronic graft-versus-host disease after hematopoietic stem cell transplantation. Cornea. 2003;22(7 Suppl):S19-27.
- [Google Scholar]
- Sjögren-like syndrome after bone marrow transplantation. J Med Assoc Thai. 2008;91:1739-47.
- [Google Scholar]
- Reliability and validity of the Ocular Surface Disease Index. Arch Ophthalmol. 2000;118:615-21.
- [Google Scholar]
- Report of the National Eye Institute/Industry workshop on Clinical Trials in Dry Eyes. CLAO J. 1995;21:221-32.
- [Google Scholar]
- Baseline profiles of ocular surface and tear dynamics after allogeneic hematopoietic stem cell transplantation in patients with or without chronic GVHD-related dry eye. Bone Marrow Transplant. 2010;45:1077-83.
- [Google Scholar]
- The definition and classification of dry eye disease: report of the Definition and Classification Subcommittee of the International Dry Eye Work Shop (2007) Ocul Surf. 2007;5:77-92.
- [Google Scholar]
- The eye in bone marrow transplantation. I. Clinical study. Arch Ophthalmol. 1983;101:580-4.
- [Google Scholar]
- The eye in bone marrow transplantation. III. Conjunctival graft-vs-host disease. Arch Ophthalmol. 1989;107:1343-8.
- [Google Scholar]
- Dry eye syndrome in long-term follow-up of bone marrow transplanted patients. Bone Marrow Transplant. 1989;4:675-8.
- [Google Scholar]
- Ocular complications of bone marrow transplantation. Br J Ophthalmol. 1991;75:611-4.
- [Google Scholar]
- Late-onset keratoconjunctivitis sicca syndrome after bone marrow transplantation: incidence and risk factors. European Group or Blood and Marrow Transplantation (EBMT) Working Party on Late Effects. Bone Marrow Transplant. 1996;17:1105-11.
- [Google Scholar]
- A retrospective study of ocular side effects in children undergoing bone marrow transplantation. Eur J Ophthalmol. 1996;6:436-9.
- [Google Scholar]
- Ophthalmological aspects in allogeneic bone marrow transplantation: Sjögren-like syndrome in graft-versus-host disease. Eur J Ophthalmol. 1997;7:13-8.
- [Google Scholar]
- Dry eye after hematopoietic stem cell transplantation. Br J Ophthalmol. 1999;83:1125-30.
- [Google Scholar]
- Ocular complications of pediatric bone marrow transplantation. Ophthalmology. 1999;106:160-4.
- [Google Scholar]
- Chronic graft-versus-host disease after allogeneic blood stem cell transplantation: long-term results of a randomized study. Blood. 2002;100:3128-34.
- [Google Scholar]
- Risk factors and characteristics of ocular complications, and efficacy of autologous serum tears after haematopoietic progenitor cell transplantation. Bone Marrow Transplant. 2006;38:223-7.
- [Google Scholar]
- Dry-eye syndrome after allogeneic stem-cell transplantation in children. Acta Ophthalmol. 2008;86:253-8.
- [Google Scholar]
- Acquisition of vernal and atopic keratoconjunctivitis after bone marrow transplantation. Am J Ophthalmol. 2008;146:462-5.
- [Google Scholar]
- Frequency of ocular manifestations of chronic graft versus host disease. J Ayub Med Coll Abbottabad. 2010;22:80-3.
- [Google Scholar]
- Ocular graft-versus-host disease after allogeneic stem cell transplantation. Cornea. 2010;29:758-63.
- [Google Scholar]
- Donor-recipient gender difference affects severity of dry eye after hematopoietic stem cell transplantation. Eye (Lond). 2011;25:860-5.
- [Google Scholar]
- Comparison of stem cell sources in the severity of dry eye after allogeneic haematopoietic stem cell transplantation. Br J Ophthalmol. 2012;96:34-7.
- [Google Scholar]
- Dry eye disease in chronic graft-versus-host disease: results from a Spanish retrospective cohort study. Transplant Proc. 2011;43:1934-8.
- [Google Scholar]
- Diagnosis and treatment of ocular chronic graft-versus-host disease: report from the German-Austrian-Swiss Consensus Conference on Clinical Practice in chronic GVHD. Cornea. 2012;31:299-310.
- [Google Scholar]
- Comparison of chronic graft-versus-host disease after transplantation of peripheral blood stem cells versus bone marrow in allogeneic recipients: long-term follow-up of a randomized trial. Blood. 2002;100:415-9.
- [Google Scholar]






