Translate this page into:
Methicillin resistance & inducible clindamycin resistance in Staphylococcus aureus
Reprint requests: Dr Mandira Banerjee, Department of Microbiology, Nilratan Sircar Medical College & Hospital, Kolkata 700 014, West Bengal, India e-mail: drsamarbanerjee@gmail.com
-
Received: ,
This is an open access article distributed under the terms of the Creative Commons Attribution NonCommercial ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Methicillin resistant Staphylococcus aureus (MRSA) isolates with inducible clindamycin resistance (iCR) are resistant to erythromycin and sensitive to clindamycin on routine testing and inducible clindamycin resistance can only be identified by D-test. This study was aimed to detect methicillin resistance and iCR among S. aureus isolates, effectiveness of some commonly used antibiotics and correlation between methicillin resistance and iCR.
Methods:
The present cross-sectional study included 46 S. aureus isolates subjected to Kirby-Bauer's disk diffusion method for antibiotic susceptibility testing (AST) to estimate MRSA and resistance to some commonly used antibiotics. D-test was employed to detect iCR.
Results:
Eleven of the 46 (23.9%) isolates tested were MRSA. Overall, 19 (41.3%) isolates showed of iCR. Vancomycin and linezolid were found to be 100 per cent effective. A positive Karl-Pearson's coefficient of correlation (0.89) between methicillin resistance and iCR was obtained.
Interpretation & conclusions:
Detection of iCR is important for the use of clindamycin in MRSA infections. Methicillin resistance and iCR appear to be clinically unrelated.
Keywords
D-test
inducible clindamycin-resistance
methicillin-resistance
MRSA
Infection with methicillin resistant Staphylococcus aureus (MRSA) has emerged as a major problem of public health importance. Methicillin resistance is usually conferred by altered penicillin binding protein (PBP-2a) that causes resistance to all ß-lactam antimicrobial agents1. Clindamycin is not recommended for any infection caused by an inducible resistant isolate. MRSA isolates with inducible clindamycin resistance (iCR) are resistant to erythromycin and sensitive to clindamycin on routine testing. D-test can help to determine whether clindamycin could be used as a therapeutic option2. Sedighi et al3 have recommended) to use D-test routinely in all microbiologic laboratories and not to apply clindamycin in patients with infections caused by inducible resistant S. aureus. They also suggested to avoid switch therapy from erythromycin to clindamycin3. We undertook this study to investigate the presence of methicillin resistance and inducible clindamycin resistance, to estimate any existing relation between these two variables and to test the effectiveness of commonly used antibiotics on MRSA.
Material & Methods
The present study was conducted during May-July 2013 at the Microbiology department of Nilratan Sircar Medical College and Hospital, Kolkata, West Bengal, India. A total of 46 non-duplicate S. aureus isolates selected consecutively (23 pus, 6 blood, 17 wound swab samples) were subjected to Kirby-Bauer's disk diffusion method4. D-test for detecting iCR was employed on all specimens.
The antibiotic susceptibility test (AST) was done using Mueller-Hinton agar plate and evaluated using Clinical and Laboratory Standards Institute (CLSI) guidelines5. The isolates were tested for cefoxitin (30 μg), clindamycin (2 μg), azithromycin (15 μg), erythromycin (15 μg), co-trimoxazole (1.25/23.75 μg), ciprofloxacin (5 μg), vanocomycin and linezolid (30 μg) each. For D-test standard procedure as depicted by Seifi et al6 was followed. Chi-square test of significance for antibiotic effect on MRSA and methicillin sensitive S. aureus (MSS) and Karl-Pearson's correlation coefficient (r) for correlating methicillin resistance in S. aureus and iCR were employed.
Results & Discussion
Of the 46 isolates tested, 11 (23.9%) were MRSA, and 35 (76.1%) were MSSA. Six of 17 (35.3%) isolates from wound swab specimens were MRSA while five of six (83.3%) isolates from blood samples were MSSA. Nineteen of 46 isolates (41.3%) showed iCR.
Wound swab and blood specimens exhibited the highest (10 of 17, 58.82%) and lowest (1 of 6, 16.67%) iCR, respectively. Six of eleven (54.54%) MRSA and 13 of 35 (37.14%) MSSA isolates showed iCR. Ten of 17 (58.8%) erythromycin-resistant and clindamycin-sensitive isolates showed positive D-test.
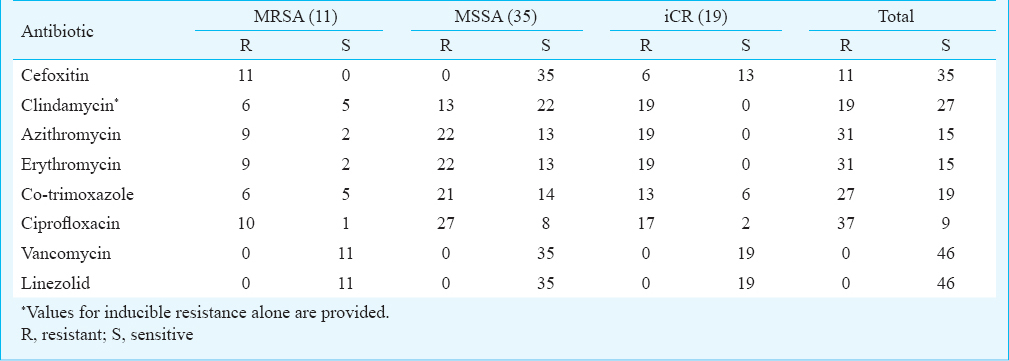
All isolates were sensitive to vancomycin and linezolid. Co-trimoxazole followed vancomycin and linezolid in effectiveness among the antibiotics tested against MRSA (45.5%), and a similar percentage of MSSA (40%) was sensitive to co-trimoxazole (Table). Nine of the 11 MRSA (81.82%) isolates, 22 of the 35 MSSA (62.86) isolates and all 19 iCR isolates were resistant to azithromycin. A study in the UK underlines the futility of using macrolides in MRSA infections7. Six of the MRSA (54.54%) and 21 of the MSSA (60%) isolates were resistant to co-trimoxazole. The correlation coefficient between MRSA and iCR in S. aureus was 0.89.
The findings on MRSA in our study was similar to that reported by Mehdinejad et al8. In a study by Prabhu et al9, 20 per cent MRSA and six per cent MSSA showed iCR contributing to an overall ten per cent prevalence of iCR. In the present study, about 40 per cent isolates showed iCR.
The relationship between MRSA and iCR appears to be clinically insignificant despite a high positive correlation coefficient.
MRSA is a growing public health problem globally. In our hospital 23.9 per cent of the tested isolates were MRSA. Higher prevalence of antibiotic resistance was noted among MRSA when tested for azithromycin and ciprofloxacin as compared to cotrimoxazole. Vancomycin and linezolid were found to be effective in all MRSA infected cases. A significant correlation could not be found between methicillin resistance and iCR.
Acknowledgment
The first author (SG) acknowledges the Indian Council of Medical Research, New Delhi, for providing Short Term Studentship.
Conflicts of Interest: None.
References
- Penicillin-binding protein 2a of methicillin-resistant Staphylococcus aureus. IUBMB Life. 2014;66:572-7.
- [Google Scholar]
- Prevalence of inducible clindamycin resistance in Staphylococcus aureus isolated from clinical samples. Med J Armed Forces India. 2014;70:43-7.
- [Google Scholar]
- D-test method for detection of inducible clindamycin resistance in Staphylococcus aureus. Iran J Pediatr. 2009;19:293-7.
- [Google Scholar]
- Antibiotic susceptibility testing by a standardized single disk method. Am J Clin Pathol. 1966;36:493-6.
- [Google Scholar]
- Clinical and Laboratory Standards Institute (CLSI). Performance standards for antimicrobial susceptibility testing; eighteenth informational supplement. CLSI document M100-18. Wayne PA, USA: CLSI; 2008.
- [Google Scholar]
- Inducible clindamycin resistance in Staphylococcus aureus isolates recovered from Mashhad, Iran. Iran J Microbiol. 2012;4:82-6.
- [Google Scholar]
- Guidelines for the prophylaxis and treatment of methicillin-resistant Staphylococcus aureus (MRSA) infections in the UK. J Antimicrob Chemother. 2009;63:849-61.
- [Google Scholar]
- Study of methicillin resistance in Staphylococcus aureus and species of coagulase negative staphylococci isolated from various clinical speciments. Pak J Med Sci. 2008;24:719-24.
- [Google Scholar]
- Inducible clindamycin resistance in Staphylococcus aureus isolated from clinical samples. J Lab Physicians. 2011;3:25-7.
- [Google Scholar]






