Translate this page into:
Maternal near miss events in India
For correspondence: Dr Ragini Kulkarni, Department of Operational Research, Indian Council of Medical Research-National Institute for Research in Reproductive Health, JM Street, Parel, Mumbai 400 012, Maharashtra, India e-mail: kulkarnir120@gmail.com
-
Received: ,
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Maternal morbidity is an indicator of the quality of a country’s maternal health services. Maternal near miss (MNM) can provide valuable information in this context and hence these cases need to be reviewed which can indirectly play a major role in reducing maternal mortality ratio in India. The objectives of the present review were to find the prevalence/incidence, criteria used for identification, review the causes of MNM cases and identify the contributory factors responsible for the occurrence of these cases based on three-delay model.
Methods:
Articles were identified from the PubMed, Google Scholar, Scopus and Cochrane Library using search terms such as ‘Maternal Near Miss’,‘maternal morbidity’, ‘India’ among others. All health facility-based observational studies conducted in India published between 2010 to 2019 irrespective of data collection period, and criteria used for identification of MNM cases were included for review. Data were extracted from included studies and summarized in terms of prevalence/incidence, ratio and percentage.
Results:
Out of 25 studies, majority were prospective observational conducted at government health facilities. The incidence of MNM varied widely from 3.9 to 379.5 per 1000 live births and 7.6-60.4 per 1000 deliveries. MNM: Maternal Death varied from 1.7:1 to 21.8:1; studies used different criteria to define MNM cases.
Interpretation & conclusions:
Hypertensive disorders and anaemia were the leading direct and indirect causes of MNM, respectively. There was a lack of uniformity in using the criteria for MNM across studies conducted in India over the last decade. Future studies on MNM in India should follow the uniform criteria mentioned in the MNM-Review guidelines released by the Government of India in 2014 for obtaining systematic data and proper summary estimates.
Keywords
Incidence
India
maternal near miss
prevalence
review
WHO criteria
Maternal mortality is a key indicator demonstrating the quality of maternal health services offered in the country. However, healthy gestation and maternal mortality are mild to severe conditions between which there is a spectrum of maternal morbidities1. In this regard, the World Health Organization (WHO) defines the criterion of severe maternal morbidity or Maternal Near Miss (MNM) as a woman who nearly died but survived a complication that occurred during pregnancy, childbirth or within six weeks after pregnancy1. MNM cases occur more often as compared to maternal deaths and have similar pathways that can directly give information about the strengths and weaknesses of the system that need to be overcome during the process of providing healthcare123. In addition, it provides stronger conclusions and rapid reports on issues related to obstetric care4. MNM is gaining more importance as maternal mortality ratio (MMR) for 2014-2016 in India is reduced to 130/100,000 live births (LB). Couple of States such as Kerala and Maharashtra have lowered MMR to as low as 46 and 61, respectively, and achieved the MDG goal for 2015 (100/1 lakh live births)5. Ministry of Health and Family Welfare, Government of India (GOI), released MNM guidelines in December 20146.
Considering the variations in the prevalence of MNM cases in India, there was a need to conduct a review to survey the prevalence/incidence of MNM cases, to study the criteria used for identification, to review the causes of MNM cases and to identify the various contributory factors such as personal/family, administrative and logistic problems responsible for the occurrence of MNM cases in India based on three-level delay model. The findings may help us to identify the modifiable factors if corrective actions were to be taken.
Material & Methods
Search strategy: Three search engines were explored including PubMed, Google Scholar, Cochrane Library. The review was restricted to studies from India, published in English from 2010 to 2019. Search terms used were ‘Maternal Near Miss’, ‘India’, ‘severe maternal morbidity’, ‘severe obstetric morbidity’, ‘Maternal Near miss audit India’, ‘Near Miss Cases’, ‘Near miss events India’, ‘Near miss obstetric events’, ‘Near Miss criteria’, ‘ Near miss tool for assessment’, ‘Near miss guidelines India’ and ‘Maternal comorbid conditions’ for review. In addition, the website of Ministry of Health and Family Welfare, Government of India (GOI), was also searched for policy documents on guidelines currently being used in India to assess severe maternal morbidity. Manual search in the bibliographic references of the articles selected was also conducted for additional relevant articles.
Inclusion criteria: All health facility-based observational studies conducted in India, published in English language from 2010 to 2019 irrespective of data collection period, and criteria used for identification of MNM cases were included for review.
Exclusion criteria: Articles published as editorials, commentaries, reports, letters to editor, studies involving MNM associated with a single disease condition/adverse event, abstracts without full paper and studies where criteria for identification of MNM cases were not clearly defined were excluded from the study.
Study selection and data extraction: The study selection procedure is schematically shown in the Figure. Initially, 483 studies were identified including four articles from other sources. Screening was initially done based on titles using search terms (key words). Then, abstracts were reviewed and only the full-text articles were selected for inclusion in the study. All the articles were reviewed separately, and disagreement between researchers was resolved by discussion and establishing consensus. A total of 25 articles were included in the review for exploring various aspects related to MNM.
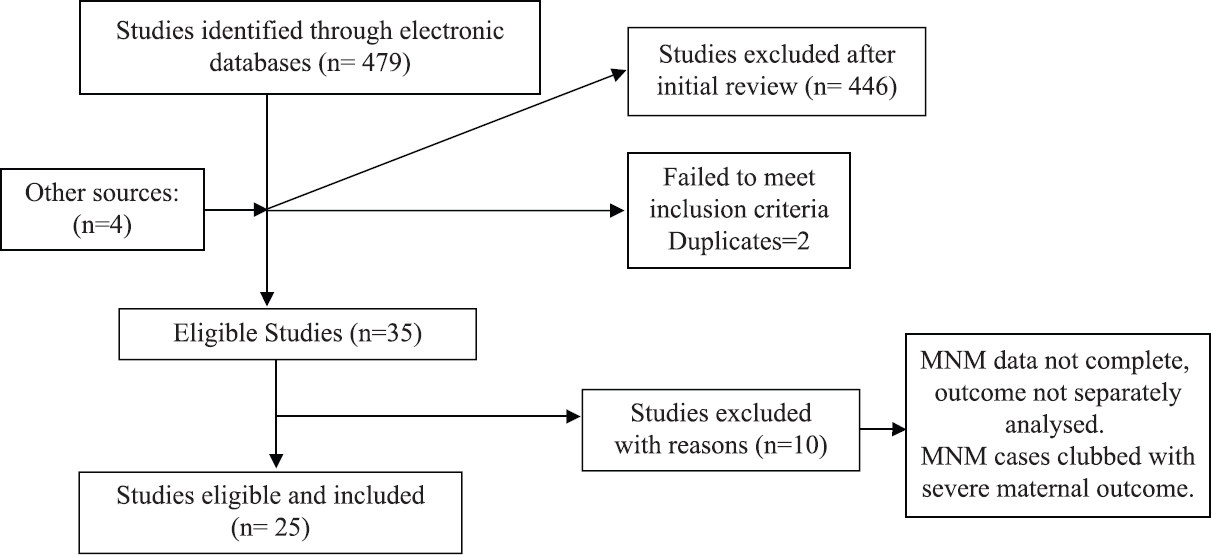
- Study selection (flowchart).
Data were extracted by two independent researchers using the inclusion and exclusion criteria including parameters such as setting, study type, duration, sample size, etc.178910. Prevalence, MNM: Maternal death ratio, mortality Index, sociodemographic factors, adverse events/disease conditions, and factors responsible for delay were also extracted from studies as presented in Tables I-IV. Studies mentioning delays based on three delay model in maternal near miss cases were included in the present review1116182223.
| Study setting and State | Year of study/duration in months (m) | MNM cases | MD | MNM criteria | Number of live births/deliveries | Incidence/1000 delivery or/1000 LB | MNM: MD | Mortality index (%) | |
|---|---|---|---|---|---|---|---|---|---|
| Prospective studies | |||||||||
| Purandare et al11 | 6 TH MS, UP, TN |
July-November 12, 16 months |
264 | - | WHO1 MOHFW, India6 |
27,433# | 9.6a | - | - |
| Venkatesh et al12 | 1 TH Karnataka |
May 12-April 13, 12 months |
18 | 3 | WHO1 | 2340# | 7.6a | 6:1 | - |
| Bakshi et al13 | 2 PHCs, 1 CHC, 1TH Uttarakhand | June 12-June 13, 12 months |
51 | 10 | WHO1 | 688 | 74.1b | 5.1:1 | 16.3 |
| Sangeeta et al14 | 1 TH, Delhi | January 12-March 13, 14 months | 27 | 8 | WHO1 | 6767 | 3.9b | 3.3:1 | 22.8 |
| Sujata et al15 | 1 TH Odisha | January 14-December 15, 24 months | 114 | 5 | WHO1 | 3340 | 34.1b | 21.8:1 | 4.3 |
| Abha et al16 | 1 TH Chattisgarh | September 13-August 15, 24 months | 211 | 102 | WHO1 | 13,895 | 15.1b | 2:1 | 32.5 |
| Patankar et al17 | 1 TH Maharashtra |
July 14-June 15, 12 months |
98 | - | WHO1 | 4571# | 21.9a | - | - |
| Kulkarni et al18 | 2 THs Maharashtra |
April 12-March 14, 12 months |
887 | 94 | WHO1 | 14,508# | 60.4a | 9.4:1 | 9.6 |
| Parmar et al19 | 1 TH Gujarat | May-September 2012, 6 months |
46 | 18 | WHO1 Water stone et al8 Mantel et al9 |
1929 | WHO criteria-20.7b Mantel-19.7b |
2.6:1 | 28.1 |
| Behera and Behera20 | 1 TH, Odisha | October 15-September 17, 24 months | 201 | 116 | WHO1 | 17,024 | 11.8b | 1.7:1 | 36.5 |
| Kamal et al21 | 1 TH Jharkhand | October 14-October 16, 24 months | 480 | - | Five factor scoring system7 | 18,426 | 26.0b | - | - |
| Reena and Radha22 | 1 TH Kerala |
August 11-October 12, 15 months | 32 | 5 | WHO1 | 3451 | 9.3b | 6.4:1 | - |
| Kumar and Tewari 23 | 1 SRU West Bengal |
May 15-June 16, 12 months |
126 | - | Filippi et al10 | - | 379.5b | - | - |
| Chaudhuri et al27 | 1 TH West Bengal |
April 2013 and October 2014 | 177 | 23 | Modified Mantels Criteria | 4081 | 43b | 7.7:1 | 11.5 |
| Alluvala et al28 | 1 TH Hyderabad |
2015 | 67 | - | WHO1 | 7821# | 8.6 | - | - |
| Pandit R et al29 | 1 TH | July 2015-February 2016 | 116 | 58 | WHO1 | - | - | 2:1 | - |
| Retrospective studies | Prevalence/1000 LB | ||||||||
| Ps R et al30 | 1 TH Karnataka |
January 11-December 12, 24 months |
131 | 23 | WHO1 | 7330 | 17.9 | 5.6:1 | 14.9 |
| Kalra et al31 | 1 TH Rajasthan |
May 11-October 12, 18 months |
112 | 54 | Five factor scoring system7 | 26,734 | 4.2 | 2.1:1 | - |
| Pandey et al4 | 1 TH Uttar Pradesh |
May 11-April 12, 12 months |
633 | 247 | WHO1 | 5273 | 120 | 2.6:1 | 32.6 |
| Bansal et al32 | 1 TH Chhattisgarh | September 13-August 14, 12 months | 39 | - | WHO1 | 3276 | 11.9 | - | - |
| Rathod et al33 | 1 TH Maharashtra |
January 11-December 13, 24 months | 161 | - | WHO1 | 22,092 | 7.2 | - | - |
| Khan et al34 | 1 Corp.hos, Delhi | September 9-August 11, 24 months | 302 | 67 | WHO1 | 20,556 | 14.6 | 4.5:1 | - |
| Tallapureddy et al35 | 1 TH Telangana |
January 14-August-14, 8 months | 32 | 6 | WHO1 | 3784 | 8.4 | 5.34:1 | 15.7 |
| Naik et al24 | 1 TH Eastern India state |
Study period not given, 12 months | 116 | 69 | WHO1 | 8436 | 13.7 | 1.68:1 | 37.3 |
| Manjunatha et al25 | 1 TH Karnataka |
January 2016-December 2016, 12 months | 25 | 4 | WHO1 | 3347 | 7.5 | 6.25:1 | 13.7 |
#Number of deliveries, aIncidence per1000 deliveries, bIncidence per1000 live births. MS, Maharashtra State; UP, Uttar Pradesh; TN, Tamil Nadu; TH, Tertiary hospital; CHC, community health centre; PHCs, primary health centres; MD, maternal death; MNM, maternal near miss; WHO: World health organization; LB, live births; MoHFW, Ministry of Health and Family Welfare
| Mean age±SD (years), (%) | Gravid status | Un-booked status* (%) | Referral status (%) | Gestational age >28 weeks (%) | ||
|---|---|---|---|---|---|---|
| Primi (%) | Multi (%) | |||||
| Prospective studies | ||||||
| Purandare et al11 | 20-29, 64.0 | - | - | - | 39.0 | - |
| Sujata et al15 | 25-35, 71.9 | 50.8 | 31.5 | 84.2 | 57.0 | 67.5 |
| Abha et al16 | 21-30, 70.6 | 38.8 | 61.1 | - | - | - |
| Patankar et al17 | 27.8±3.4 | 26.5 | 39.7 | 80.6 | 70.4 | 59.1 |
| Kulkarni et al18 | 25.8±4.6 | 41.0 | - | - | 77.0 | 59.5 |
| Behera and Behera20 | 20-30, 80.6 | 56.2 | 43.8 | 74.1 | 61.2 | - |
| Kamal et al21 | 18-35, 27.0 | 28.7 | - | 80.0 | 40.0 | - |
| Reena and Radha22 | 21-34, 87.5 | 37.5 | 62.5 | - | 84.0 | 68.9 |
| Kumar and Tewari23 | 20-29, 66.6 | 33.5 | 39.6 | 10.0 | - | 68.7 |
| Chaudhuri et al27 | 20-35, 80.5 | 87.0 | 13.0 | 32.4 | 80.2 | 80.2 |
| Retrospective studies | ||||||
| Ps R et al30 | 27.0±4.7 | 56.4 | 43.6 | - | 86.9 | 57.2 |
| Kalra et al31 | 24.0±3.11 | 48.2 | 27.9 | - | - | 53.5 |
| Pandey et al4 | 18-35, 88.2 | 34.4 | 65.6 | 94.3 | 53.1 | 71.9 |
| Bansal et al32 | 18-24, 41.0 | 5.9 | 64.1 | - | - | 56.4 |
| Rathod et al33 | 21.8 | 19.8 | 9.3 | 18.6 | - | 69.6 |
| Khan et al34 | 26.7±4.6 | 36.4 | - | 71.9 | - | - |
| Naik et al24 | 26.0 | - | - | - | - | - |
| Manjunatha et al25 | 21-25, 40.0 | 55.0 | 45.0 | 48.0 | 12.0 | 94.0 |
*Unregistered pregnancies. SD, standard deviation
| Hypertensive disorders (%) | Severe anaemia (%) | Haemorrhage (%) | Sepsis (infections) (%) | Ruptured uterus (%) | ICU admissions (%) | Other significant conditions (%) | |
|---|---|---|---|---|---|---|---|
| Prospective studies | |||||||
| Purandare et al11 | 26.5 | 8.6 | 46.9* | 4.4 | 16.0 | - | Hepatitis-6.3 |
| Venkatesh et al12 | 7.0 | - | 14.0* | 3.5 | 3.5 | - | Rupture ectopic Pregnancy-49.1 |
| Bakshi et al13 | 23.5 | - | 37.3 | 58.9* | 3.92 | - | - |
| Sangeeta et al14 | 12.7 | 7.4 | 40.7* | 7.4 | 31.5 | 21.5 | Med/surgical-18.5 |
| Sujata et al15 | 38.5* | - | 29.8 | 7.0 | 3.5 | 27.1 | LSCS-41.2 |
| Abha et al16 | 33.1 | 57.0* | 27.5 | 4.3 | 6.6 | - | Septic abortion-4.2 |
| Patankar et al17 | 51.0* | - | 43.9* | 3.1 | 3.1 | 64.3 | Medical-13.2 |
| Kulkarni et al18 | 61.2* | 55.1 | 8.8 | 25.0 | - | 35.2 | - |
| Parmar et al19 | - | - | - | 14.0 | - | 36.8 | - |
| Behera and Behera20 | 17.2 | 28.5* | 11.5 | 3.5 | 7.0 | - | Obstructed labour-37.9* |
| Kamal et al21 | 23.5 | - | 42.5* | 10.0 | 12.9 | - | |
| Reena and Radha22 | 40.6* | - | 21.8 | 12.5 | - | - | Scarred uterus-43.7 |
| Kumar and Tewari23 | 59.3* | 22.7 | 8.9 | 6.3 | - | - | Dystocia-2.7 |
| Chaudhuri et al27 | 55.9* | 16.3 | 1.6 | Acute renal failure-6.5 Jaundice-1.5 |
|||
| Pandit et al29 | 18.1 | 31.9 | Hepatic disease-9.4 Renal failure-6.8 |
||||
| Retrospective studies | |||||||
| PS et al30 | 23.6 | - | 44.2* | 16.3 | 62.6 | Medical-11.6 | |
| Kalra P et al31 | 17.8 | - | 56.0* | 5.35 | 8.9 | 75.0 | - |
| Pandey et al4 | 33.0 | 20.7 | 45.7* | 7.4 | 5.8 | 40.9 | Ruptured ectopic pregnancy-21.5 |
| Bansal et al (2016)32 | 12.8 | 15.4 | 43.5* | 5.12 | 15.4 | - | Malaria-5.1 Hepatitis-2.6 |
| Rathod et al33 | 11.8 | 24.8 | 26.7* | 11.2 | - | 26.7 | Hepatitis-16.8 |
| Khan et al34 | 20.5 | 4.3 | 63.4 * | 2.7 | - | 81.5 | - |
| Tallapureddy et al35 | 31.2 | 65.6* | 43.7 | - | - | - | Other causes-15.6 |
| Naik et al24 | 40.5* | - | 18.0 | 31.0 | 7.8 | 53.4 | Dystocia-10.0 |
| Manjunatha et al25 | 20.0 | - | 28.0 | 32.0* | - | 88.0 | Multiple blood transfusion-48.0 |
*Leading cause. ICU, intensive care unit; LSCS, lower segment caesarean section
| Studies delays | Factors | Purandare et al (2013)11 (%) | Abha et al16 (%) | Kulkarni et al18 (%) | Reena and Radha22 (%) | Kumar and Tewari23 (%) |
|---|---|---|---|---|---|---|
| Delay 1-D1 | Delay in seeking help/care | 60.6 | 44.1 | 6.3 | 38.0 | |
| Transport and other logistical problems | 30.3 | - | 20.8 | - | ||
| Delay 2-D2 (referral facility) | Lack of equipment and materials | 13.6 | 36.0 | Referral-68.2 | Access to care-25.0 | - |
| Lack of blood and blood products | 7.6 | Lab invest-16.6 | Both D1 and D2-12.5 | |||
| Delay 3-D3 (present facility) | Lack of equipment and materials, blood and blood products at the present facility | - | 19.9 | 2.7 | Adequate and appropriate t/t-18.7 | - |
| Both D2 and D3-3.1 |
Results
Twenty five studies were included for review representing all the major regions of India. A total of 16 were prospective studies (PS), while nine were retrospective studies (RS). Out of 25 studies in review, 10 PS and eight RS described the sociodemographic characteristics of study participants including age, gravid status, gestational period and registration as well as referral status.
Prospective studies: Sixteen studies conducted at 21 health facilities representing most regions of India were included in review,11121314151617181920212223272829. For the incidence of MNM, most studies mentioned LB as denominator while few mentioned deliveries. Majority of the studies (n=13) used WHO criteria1 to define MNM cases, whereas Parmar et al19 used both WHO, Mantel and Waterstone criteria. Kumar and Tewari23 used Filippi criteria, five scoring system was used by Kamal et al21 and Chaudhuri and Nath27 used modified Mantel’s criteria. The incidence of MNM cases showed a wide variation from 3.9 to 379.5 per 1000 LB, whereas it ranged between 7.6 and 60.4 per 1000 deliveries. The MNM: Maternal death ratio varied from 1.7:1 to 21.8:1 and the mortality index varied from 4.3 to 36.5 per cent111213141516171819202122 (Table I).
Age of the participants varied highly ranging from 18 to 35 yr. MNM cases were more common among multipara ranging from 31.5 to 62.5 per cent. The overall referral rate was more than 50 per cent in all the studies except two1121. Most studies indicated that more than 70 per cent cases admitted to the hospital were unbooked, i.e. first-time visitors. Most MNM cases (59.1-80.2 %) were admitted with gestational age more than 28 wk (Table II).
Out of 16 studies, clinical conditions were mentioned in 15 studies. Eight cases had hypertensive disorders as a cause of MNM (7.0-61.2 %), and haemorrhage was also a cause of MNM in eight studies (8.8-46.9%). In a study by Bakshi et al13, sepsis was also an important cause among 58.9 per cent MNM cases. Severe anaemia (7.4-57 %) was reported as one of the causes of MNM in some of the studies (Table III).
Out of 16 studies, organ dysfunction-based criteria were included in seven studies14151617182027. Among these, coagulation dysfunction was most common complication (2.6-60 %). In a study done by Patankar et al17, 28 cases (28.5 %) of MNM included combined coagulation and vascular dysfunction cases.
Regarding the three-delay models, most studies showed that the first-level delay (D1) (6.3-60.6 %) including delay in seeking help and other personal problems was responsible for MNM cases11162223. Transport and other logistic problems contributed to 20.8-30.3 per cent of MNM cases1118. Second-level delay (D2) at referral centres including lack of infrastructural issues, lack of equipment, medications, instruments, unavailability of blood and blood products in referral facilities ranged from 7.6 to 68.2 per cent contributing to MNM cases1118. Third-level delay (D3) at facilities including similar parameters ranged from 2.7 to 19.9 per cent1618. Thus, it was noted that the first and second-level delay was most common in the reviewed studies (Table IV).
Retrospective studies: Nine studies included in the review were conducted at eight tertiary hospitals and one corporation hospital42425303132333435. The prevalence of MNM cases varied from 4.2 to 120 per 1000 LB. The MNM ratio varied from 1.68:1 to 6.25:1 and the mortality index ranged between 13.7 and 37.32425 (Table I).
Age of the women ranged from 18 to 35 yr and primigravida women were higher in proportion ranging from 5.9 to 56.4 per cent3032. Overall referral rate was more than 50 per cent except in a study done by Manjunatha et al25. The number of unbooked cases showed a wide variation ranging from 18.6 to 94.3 per cent433 (Table II).
Haemorrhage was one of the causes for MNM events (18-63.4 %)2434 whereas hypertensive disorders ranged between 11.8 and 40.5 per cent. In a study done by Tallapureddy et al35, severe anaemia (65.6 %) was a leading indirect cause for MNM cases. Adverse events requiring intensive care unit (ICU) admission was also an important finding in MNM cases (26.7-88.0 %)3334 (Table III). Only three studies have elaborated about organ dysfunction criteria for identifying MNM cases where coagulation dysfunction was a most common complication (34.4-53.4 %)333435.
Discussion
In the present review, an attempt was made to review all the studies on MNM conducted in India over the past decade, which provide the prevalence/incidence, criteria used for identification of MNM cases, causes of MNM and factors contributing for the occurrence of these cases based on three-delay model.
Twenty three studies were conducted in urban settings411121415161718192021222425272829303132333435, while only two1323 were conducted in rural settings. This may be due to the fact that most cases in rural scenario were referred to urban tertiary care centres for further management. It was observed that most studies done were in urban areas at tertiary health facilities, which may not reflect the prevalence/incidence is such institutions. Most cases were referred from the referral units situated in rural areas, this indicates that the first referral units need to be strengthened so that they can cater to basic obstetric emergencies such as haemorrhage, hypertensive disorders, sepsis and shock. Thus, improvement in the infrastructure and facilities at secondary level centres may pave a way for identification of MNM cases and conduction of MNM studies at these centres.
The wide variation in incidence/prevalence, mortality index and MNM: Maternal death ratio411121314151617181920212223272829303132333435 may be dependent on various reasons. Firstly, due to methodological issues like study design, study setting and duration of data collection. Thus, from the data generated, no single estimate of MNM incidence ratio could be done. Hence, instead of single estimation, annual estimation may be beneficial in improving the provision of maternal health care. Second, the criteria used for identification of MNM cases varied in few studies published before 2011. Mantel’s criteria9 adopts the occurrence of maternal organic dysfunction and focus on serious diseases, however, these depend on the existence of a minimal level of care, including laboratory tests and material for critical patient monitoring. Waterstone’s criteria8 are based on clinical criteria and are simple to use; however, it has too low a threshold to label the case as near miss. Early pregnancy complications such as ectopic pregnancies and abortions are not included in these criteria. Geller’s criteria7 on the other hand propose a multiple approach and are mainly based on obstetric hospitalizations in ICUs. Therefore, these present the serious disadvantage of utility in services with more intensive care availability.
The WHO published MNM criteria based on markers of clinical, management and organ dysfunction in 201126 for systematic data collection on MNM and development of summary estimates. However, as per these criteria, case is defined as MNM if any of the three criteria are fulfilled. In the present study, out of 25 studies, 13 PS and eight RS used the WHO criteria to identify MNM cases whereas four studies19212331 used other criteria including five scoring system7, Waterstone et al8, Mantel et al9 and Filippi et al10, indicating a lack of uniformity in the criteria used for diagnosis of MNM cases.
The Ministry of Health and Family Welfare, Government of India, released MNM guidelines in December 20146. These guidelines are applicable in the Indian scenario and are based on a pilot study conducted in six medical colleges across India. The guidelines mention that for identification of an MNM case, minimum three criteria from each category – clinical findings (either symptoms or signs), investigations and interventions must be met; or if any single criteria that signifies cardiorespiratory collapse is present, then the case is identified as MNM. The clinical findings, investigations and interventions have been put under three broad categories – pregnancy specific obstetric and medical disorders, pre-existing disorders aggravated during pregnancy and accidental/incidental disorders of pregnancy. These categories have been further segregated under adverse events such as haemorrhage, sepsis and hypertension6. Furthermore it was found that although the data collection period in three studies was after 2014, the researchers have not used the criteria as per the MNM-R guidelines (2014) of GOI. For future studies, there is a need to follow the MNM guidelines in Indian scenario for systematic data collection on MNM cases and for obtaining proper summary estimates.
The overall MNM: Mortality ratio showed wide variation (1.7:1-21.8:1 for PS and 1.68:1-6.25:1 for RS) using the WHO criteria. It is one of the most sensitive indicators for social inequalities, which shows high inter-State variation within the country.
Third, demographic profile of women with near miss events indicated that the common age group was 20-30 yr. Most studies showed that majority of women had crossed viability period (more than 28 wk) ranging from 24.1 to 72 per cent. This shows that maternal complications develop mostly during the third trimester denoting it as the most vulnerable period for a woman surviving near miss event.
The causes of MNM cases varied across studies. Out of 25 studies, nine (five prospective and four retrospective) studies showed massive blood transfusion (>five units) as one of the criteria of MNM case identification41114151720222531. As commonly observed in India, majority of the women were anaemic across studies161835 and severe anaemia was overall responsible for the highest number of MNM cases. Other common causes were hypertensive disorders and haemorrhage which can be managed well during antenatal period. Thus, it is important that mothers should be well informed regarding impending warning signs of pregnancy and educated for undergoing regular ANC check-up through involvement of health workers. Regarding the three-delay model, it was noted that the first and second-level delay was most common in the reviewed studies. This may help policymakers to identify the modifiable factors for corrective actions to be taken.
As far as the three-delay model for MNM cases is concerned, only five of the 13 PS provided any information on the contributory factors. These five studies made only a passing mention of the proportion of cases with level of delays.
As there was a lack of uniformity in using the criteria for MNM across studies conducted in India over the last decade, it was difficult to estimate true prevalence/incidence of MNM which was limitation. A meta-analysis of the data from the published studies were not possible due to a wide variation in selection criteria, definitions, methodological issues and study duration. The present review may hence be influenced by selection as well as recall bias in individual studies other than incomplete information from case record forms in these studies.
Overall, there was a wide variation in the prevalence/incidence of MNM cases across studies. To estimate the true prevalence/incidence of MNM cases, a uniform criteria for the identification of MNM cases as per MNM-R guidelines released by MOHFW, GOI, should be adopted. Furthermore, the denominator used for calculating the prevalence/incidence of MNM should be uniform considering LB being used for calculating MMR. More emphasis should be given on three-delay model to identify modifiable factors and taking corrective measures for reducing MNM cases.
Financial support & sponsorship: None.
Conflicts of Interest: None.
References
- Regional Office for Europe. Conducting a Maternal Near-Miss Case Review Cycle at the Hospital Level“Manual with Practical Tools. 2016. Available from:http://www.euro.who.int/__data/assets/pdf_file/0003/324390/NMCR-manual-en.pdf?ua=1
- [Google Scholar]
- A population-based surveillance study on severe acute maternal morbidity (near-miss) and adverse perinatal outcomes in Campinas, Brazil:The Vigimoma Project. BMC Pregnancy Childbirth. 2011;11:9.
- [Google Scholar]
- Evaluation of obstetric near miss and maternal deaths in a tertiary care hospital in North India:Shifting focus from mortality to morbidity. J Obstet Gynecol India. 2014;64:394-9.
- [Google Scholar]
- National Institution for Transforming India, Government of India. Niti Aayog. Available from:http://niti.gov.in/content/maternal-mortality-ratio-mmr-100000-live-births
- [Google Scholar]
- Maternal Health Division, Ministry of Health &Family Welfare. Government of India. Maternal near miss review operational guidelines. Available from:http://www.nrhmorissa.gov.in/writereaddata/Upload/Documents/Maternal_Near_Miss_Operational_Guidelines.pdf
- [Google Scholar]
- A scoring system identified near-miss maternal morbidity during pregnancy. J Clin Epidemiol. 2004;57:716-20.
- [Google Scholar]
- Incidence and predictor of severe obstetric morbidity:Case-control study. BMJ. 2001;322:1089-93.
- [Google Scholar]
- Severe acute maternal morbidity:A pilot study of a definition for a near-miss. BJOG. 1998;105:985-90.
- [Google Scholar]
- Maternity wards or emergency obstetric rooms?Incidence of near - miss events in African hospitals. Acta Obstet Gynecol Scand. 2005;84:11-6.
- [Google Scholar]
- Maternal near-miss reviews:Lessons from a pilot programme in India. BJOG. 2014;121(Suppl 4):105-11.
- [Google Scholar]
- Implementation of WHO near-miss approach for maternal health at a tertiary care hospital:An audit. J Obstet Gynecol India. 2016;66:259-62.
- [Google Scholar]
- Indicators of maternal “near-miss“morbidity at different levels of health care in North India:A pilot study. Bangladesh J Med Sci. 2015;14:254.
- [Google Scholar]
- Evaluation of severe maternal outcomes to assess quality of maternal health care at a tertiary center. J Obstet Gynecol India. 2015;65:23-7.
- [Google Scholar]
- Evaluation of obstetric near miss and maternal deaths in a tertiary care teaching hospital. Int J Recent Sci Res. 2016;7:9001-5.
- [Google Scholar]
- Maternal near miss:A valuable contribution in maternal care. J Obstet Gynecol India. 2016;66:217-22.
- [Google Scholar]
- Severe acute maternal morbidity (near miss) in a tertiary care center in Maharashtra:A prospective study. Int J Sci Stud. 2016;4:134-40.
- [Google Scholar]
- Prospective observational study of near-miss obstetric events at two tertiary hospitals in Mumbai, Maharashtra, India. Int J Gynecol Obstet. 2016;132:170-3.
- [Google Scholar]
- Incidence of maternal “near-miss“events in a tertiary care hospital of central Gujarat, India. J Obstet Gynecol India. 2016;66:315-20.
- [Google Scholar]
- Study on maternal mortality and miss case. J Evid Based Med Healthc. 2017;4:5720-4.
- [Google Scholar]
- A study of maternal near miss cases at tertiary medical college of Jharkhand India. Int J Reprod Contracept Obstet Gynecol. 2017;6:2375-80.
- [Google Scholar]
- Factors associated with maternal near miss:A study from Kerala. Indian J Public Health. 2018;62:58-60.
- [Google Scholar]
- “Near-miss obstetric events“and its clinico-social correlates in a secondary referral unit of Burdwan district in West Bengal. Indian J Public Health. 2018;62:235-8.
- [Google Scholar]
- Comparison of near miss obstetric events and maternal deaths in a tertiary care teaching hospital from Eastern India. Int J Reprod Contracept Obstet. 2018;7:3619-24.
- [Google Scholar]
- A study of maternal near miss at a district teaching hospital:A retrospective observational study. Int J Reprod Contracept Obstet Gynecol. 2018;7:1421-6.
- [Google Scholar]
- Evaluating the quality of care for severe pregnancy complications the WHO near-miss approach for maternal health. Published, 2011 Available from:https://www.who.int/reproductivehealth/publications/monitoring/9789241502221/en/
- [Google Scholar]
- Life-threatening complications in pregnancy in a teaching hospital in Kolkata, India. J Obstet Gynecol India. 2019;69:115-22.
- [Google Scholar]
- One-year follow-up of women with severe acute maternal morbidity (SAMM):A cohort study. J Obstet Gynecol India. 2019;69:211-7.
- [Google Scholar]
- Applicability of WHO Maternal Severity Score (MSS) and Maternal Severity Index (MSI) model to predict the maternal outcome in near miss obstetric patients:A prospective observational study. Arch Gynecol Obstet. 2019;300:49-57.
- [Google Scholar]
- “Near miss“obstetric events and maternal deaths in a tertiary care hospital:An audit. J Pregnancy. 2013;2013:393758.
- [Google Scholar]
- Obstetric near miss morbidity and maternal mortality in a Tertiary Care Centre in Western Rajasthan. Indian J Public Health. 2014;58:199-201.
- [Google Scholar]
- Study of near miss cases in obstetrics and maternal mortality in Bastar, Chhattisgarh, India. Int J Reprod Contracept Obstet Gynecol. 2016;5:620-3.
- [Google Scholar]
- Analysis of near-miss and maternal mortality at tertiary referral centre of rural India. J Obstet Gynecol India. 2016;66:295-300.
- [Google Scholar]
- Prognostic factors of maternal near miss events and maternal deaths in a tertiary healthcare facility in India. Int J Gynecol Obstet. 2017;138:171-6.
- [Google Scholar]
- “Near-Miss“Obstetric events and maternal mortality in a Tertiary Care Hospital. Indian J Public Health. 2017;61:305-8.
- [Google Scholar]






