Translate this page into:
Malaria incidence among paramilitary personnel in an endemic area of Tripura
Reprint requests: Dr Sunil Dhiman, Scientist ‘B’, Defence Research Laboratory, Tezpur, Assam 784 001, India e-mail: sunildhiman81@gmail.com
-
Received: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Paramilitary operations along the Indo-Bangladesh border are adversely affected by malaria induced morbidity and mortality. Villages surrounding the paramilitary installations often serve as disease reservoirs. Malaria incidence in Tripura State Rifles (TSR) units in Dhalai District of Tripura was studied and the role of the village population in disease transmission was also assessed.
Methods:
Mass blood surveys were carried out among TSR personnel and villagers during 2007 to 2009. Malaria diagnosis through blood smear examination and rapid detection kits was done, and percentage parasitaemia was determined. Activity of malaria vectors was monitored using CDC light traps.
Results:
Slide positivity rates (SPR) in the neighbouring villages (51.4%) was significantly higher than that in TSR (27.7%) (P<0.0001). Malaria incidence in villages did not show seasonal variability while it was lowest during post-monsoon season in TSR (P<0.325; OR = 0.74). Per cent Pf parasitaemia was high in TSR (0.29) as compared to villagers (0.20) (P<0.0001). Anopheles minimus and An. dirus were the major malaria vectors observed.
Interpretation & conclusions:
Paramilitary and public health authorities should adopt targeted measures to reduce the malaria incidence in the villages surrounding the paramilitary installations as the village populations play a major role in disease transmission.
Keywords
Malaria
paramilitary
parasitaemia
Plasmodium falciparum
Tripura
Malaria continues to cause high rates of morbidity and mortality in India, and remains as a major public health concern in the country. There is an increasing trend in the proportion of Plasmodium falciparum infection in India during the last few decades and the parasite has become resistant to conventional drugs1. The northeastern States of India are highly prone to malaria incidence and transmission, and the control of P. falciparum malaria poses a great challenge to development of this part of the country2. The State of Tripura in the northeastern region of India is surrounded by Bangladesh except in the north. The State is strategically important since it shares a long international border with frequent movement of defence forces guarding it. There is a high risk of acquiring the infection along the inter-state or international border areas and severe morbidity is being regularly reported from among the defence personnel posted in these areas3. Outbreaks of malaria may incapacitate large number of personnel so as to hinder military operations in sensitive areas. The armed forces and paramilitary personnel deployed in the region are particularly vulnerable to malaria due to outdoor patrolling activities and lack of immunity. The village populations surrounding the paramilitary installations serve as reservoirs for malaria parasites and hence have an important role to play in the epidemiology of malaria among the service personnel45.
Tripura State Rifles (TSR) is a paramilitary force deployed in the State with many outposts along the Indo-Bangladesh border. The present investigation was undertaken to determine the incidence of malaria in TSR units and outposts along the Indo-Bangladesh border in Dhalai district of Tripura. The disease incidence in the villages surrounding the paramilitary installations in these areas was also studied and comparisons were made.
Material & Methods
Study area : Dhalai district of Tripura, situated between 23°25’N to 24°14’N latitude and 91°44’ E and 92°10’ E longitude, shares a 169 km long international border with Bangladesh. It has an area of 2312.29 km2and a population of over 0.3 million. The mean temperature ranges from 5.3° to 36°C with an annual rainfall of 220 cm. The present study was carried out in Tripura State Rifles 8th Battalion Headquarters at Lalcherra and in the outposts at Kakchangamin and Kacharicherra in Dhalai district of Tripura during 2007-2009. The study was a part of project sanctioned by DRDO for Tripura State Riffles (TSR) on the request of Govt. of Tripura. The entire project was approved by the institutional ethical committee (IEC). The villages neighbouring these TSR units and outposts were also surveyed. Each study site was visited twice during pre-monsoon (March-June), monsoon (July-September) and post-monsoon (October-February) seasons. There were dense forest areas around Kakchangamin and Kacharicherra outposts. The neighbouring villages were surrounded by paddy fields, ponds and streams and were mainly inhabited by tribal people and migrant labourers.
Mass blood survey: Thick and thin smears were prepared on slides by collecting finger-prick blood samples from personnel in the TSR units and from persons in the neighbouring villages. The blood samples were collected only from cases having fever or with fever history in past 14 days. Malaria diagnosis using Optimal-IT Malaria Test Kit (TCS Biosciences Ltd., Buckinham, United Kingdom) was done and the positive subjects were treated in accordance with National Vector Borne Disease Control Programme guidelines6 under the supervision of a local medical practitioner. Microscopic examination of blood smears for malaria parasite was done after staining with Giemsa stain. The positive slides, mixed with 10 per cent negative slides, were again examined by a senior technician for confirmation. Epidemiological indices such as slide positivity rate (SPR), slide falciparum rate (SFR), slide vivax rate (SVR) and Plasmodium falciparum per cent (Pf %) were calculated. The parasites were counted against 200 white blood cells (WBC) and the counts were presented as parasitaes per microlitre of blood assuming 8000 WBC per microlitre. The percentage parasitaemia was calculated as; % parasitaemia = (parasite per microlitre of blood/ 4,000,000) × 100, where 4,000,000 red blood cells (RBC) were assumed per microliter of blood7.
Monitoring of vector activity: Centers for Disease Control and Prevention (CDC) light traps were setup in the TSR units as well as in the neighbouring villages to monitor malaria vector activity during 1800-0600 h. The adult mosquitoes collected were identified using standard keys89.
Statistical analysis: The rates of malaria incidence among TSR personnel in the study areas were compared with that in the surrounding villages using Chi-square test. The disease incidences during pre-monsoon, monsoon and post-monsoon seasons were also compared and odds ratios were determined. ANOVA was used for comparing the per cent parasitaemia among the three TSR units and also for analysing the season-wise differences in parasitaemia among the village population. The per cent parasitaemia in TSR and villagers were compared using ‘Student's ‘t’ test.
Results
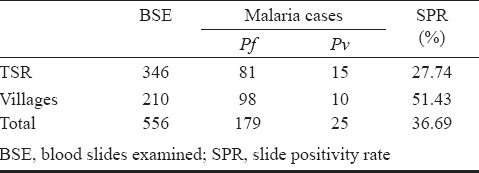
Of the 346 blood slides were collected from TSR units in the district, 81 tested positive for P. falciparum while 15 were positive for P. vivax (Table I). The SPR was 27.7 per cent while SFR was 23.4 per cent. Of the 210 blood samples collected from surrounding villages, 98 P. falciparum and 10 P. vivax positive cases were detected (SPR = 51.4%; SFR = 46.7%).
In the Kakchangamin outpost of TSR, a total of 27 malaria cases were detected (SPR = 36%; SFR = 28%) while 43 (SPR = 23.7%; SFR = 19.9%) and 26 (SPR = 28.9%; SFR = 26.7%) cases were detected in Lalcherra and Kacharicherra, respectively (Table II). There was no significant difference in the incidence of malaria among the three units of TSR. In the villages surrounding the TSR units, 47 cases were reported from Kakchangamin (SPR=39.8%; SFR=32.2%) whereas 9 (SPR=SFR=39.1%) and 52 (SPR=75.4; SFR=73.9%) cases were reported from Lalcherra and Kacharicherra, respectively. The cases of malaria were significantly higher in Kacharicherra in comparison with the other villages (P<0.0001).
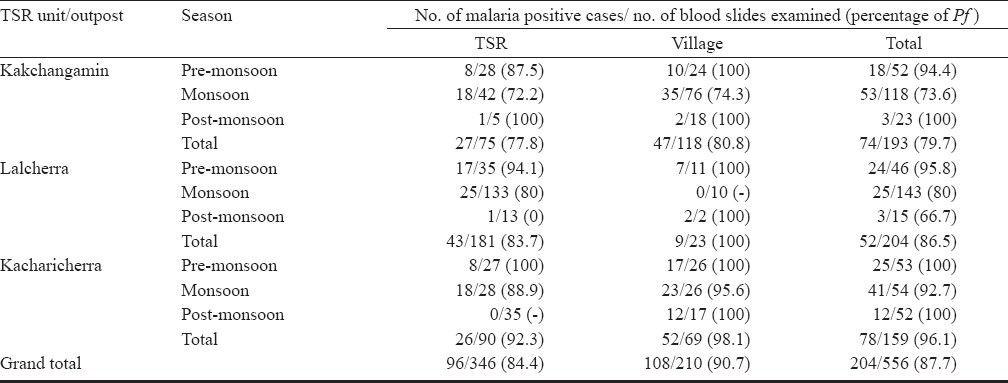
Season-wise analysis of malaria incidence in TSR indicated that SPR was significantly low during post-monsoon season (3.77%) whereas there was no significant difference in SPR between monsoon (30.05%) and pre-monsoon (36.67%). SPR in the villages were 55.74, 51.79 and 43.24 per cent during pre-monsoon, monsoon and post-monsoon seasons respectively, which did not differ significantly. Comparison of SPR between TSR and villages revealed that the villagers had a higher SPR (P<0.001).
The per cent P. falciparum parasitaemia in TSR units at Kakchangamin, Lalcherra and Kacharicherra (0.42 ± 0.03, 0.21 ± 0.02 and 0.28 ± 0.01 respectively) was significantly different among each other (P<0.001). Parasitaemia in TSR during monsoon (0.31 ± 0.02) and pre-monsoon (0.26 ± 0.02) seasons did not differ significantly. Per cent parasitaemia during monsoon, post-monsoon and pre-monsoon seasons in the villages were 0.26 ± 0.02, 0.12 ± 0.02, 0.16 ± 0.01 respectively, which were significantly different (P<0.001). Comparison of Pf per cent parasitaemia between TSR (0.29 ± 0.01) and villages (0.20 ± 0.01) indicated that the paramilitary personnel were having higher parasitaemia than the villagers (P<0.001).
Light trap collections of adult mosquitoes indicated that An. minimus and An. dirus were the major malaria vectors present with per trap night densities (mean ± SEM) of 8.2 ± 1.1 and 1.3 ± 0.2 respectively. An. philippinensis/nivipes, An. barbirostris, An. crawfordi and An. vagus were also observed in trap collections.
Discussion
The areas adjacent to the Indo-Bangladesh border are at high risk of malaria outbreak due to inadequate health infrastructure and lack of vector control operations10. Armed forces and paramilitary personnel deployed in these areas often have low levels of immunity, which make them vulnerable to diseases like malaria11. Studies on malaria incidence conducted in Tripura revealed a high rate of malaria incidence among General Reserve Engineering Force (GREF) engaged in road construction than the army personnel. This was attributed to better adherence to malaria control measures in army than in GREF12. The present study, carried out among the Tripura State Rifles personnel and the people inhabiting the neighbouring villages revealed the severity of malaria incidence in the areas adjoining the security-sensitive international border.
It was observed that adoption of control measures like indoor residual spray with DDT and use of bed nets was better in the TSR battalion headquarters at Lalcherra. Consequently the incidence of malaria in the headquarter was low in comparison with that in the outposts. The Kakchangamin outpost which was a relatively new installation recorded the highest incidence of malaria. Most of the personnel in this unit were either new recruits or were moved in from other parts of the State. The local population residing around the unit consisted mainly of tribal communities and migrant labourers. The tribal people in Tripura are semi-immune and asymptomatic carriers of malaria, thereby forming reservoirs for the newly inducted personnel12. Migrant labourers play an important role in the spread of malaria and hence the epidemiology of migration malaria in such areas needs to be studied further13. The migrant population in general remains out of reach of the health services and are often hesitant to comply with the malaria control strategies14. Shifting cultivation, which is considered to be one of the main contributory factors towards the incidence of malaria in northeastern India, was widely practiced in the area15. The TSR outpost at Kacharicherra was located in an area surrounded by deep forests. There was high incidence of malaria in the neighbouring villages, which were inhabited by tribal people who depend heavily on forest produce for their livelihood.
Comparison of malaria incidence between the TSR units and the village populations indicated that SPR in the village population was almost double as that of the service personnel. The tribal people and migrant labourers are at a high risk of acquiring and transmitting malaria as they frequently spent nights in the open and are more exposed to the malaria vectors13. The service personnel on the other hand, use personal protective measures which considerably reduce man - mosquito contact. Studies on malaria incidence carried out in an Air Force Station in Central India, revealed that SPR in neighbouring villages was significantly higher than that of the service personnel. It was also reported that adoption of targeted control measures could bring down the incidence of malaria among the Air Force personnel, while the disease continued to cause havoc among the local population416.
The percentage contribution of Pf to the total positive cases (%Pf) in the study sites, ranged from 77.8 to 92.3. In general, the TSR personnel, many of whom were recruited from non endemic areas of the country, were found to have more parasitaemia than the villagers due to their low levels of immunity. Malaria often leads to severe clinical complications in highly mobile and non-immune personnel as revealed by the studies on Central Reserve Police Force (CRPF) battalions in northeastern India3.
Malaria incidence in TSR was low in post-monsoon season, whereas the rates of incidence in the villages were uniform throughout the year. It has been already established that malaria transmission in the northeastern region continues uninterrupted, aided by the vectors, An. minimus, An. fluviatilis and An. dirus2. The per cent P. falciparum parasitaemia in village populations was high during the monsoon season, whereas there was no seasonal variation in parasitaemia among the TSR personnel. An. dirus and An. minimus observed in light trap collections from the area are principal vectors of malaria in the northeastern India and the control of these vectors is essential for reducing malaria incidence in the region1718.
Malaria control operations in paramilitary forces like TSR are often directed at reducing the disease incidence among the troops. The present study draws attention to the fact that the villages surrounding the TSR units have a high incidence of malaria and hence play a major role in malaria transmission among the TSR personnel. Therefore, these villages should also be subjected to the same set of malaria control measures as followed in the paramilitary installations. Malaria surveillance and chemotherapy of the adjoining village population should be carried out in a regular manner. The State health authorities should initiate targeted efforts to reduce malaria incidence in these villages by active surveillance of all fever cases. Use of personal protective measures against vector borne diseases needs to be popularised among the troops. Rapid detection kits should be used to monitor the personnel moving in or out of the endemic areas and chemoprophylaxis should be adopted at the recommended doses.
The authors thank Tripura State Rifles for the cooperation rendered and Department of Health, Government of Tripura for the facilities provided during the conduct of the study. The authors also thank Dr Manash J. Nath, Defence Research Laboratory, Tezpur for GIS mapping of the study areas.
References
- Predictors of knowledge about malaria in India. J Vector Borne Dis. 2007;44:189-97.
- [Google Scholar]
- Transmission of malaria and its control in the northeastern region of India. J Assoc Physicians India. 2003;51:1073-6.
- [Google Scholar]
- Malaria related morbidity in central reserve police force personnel located in the north-eastern states of India. J Hum Ecol. 2004;15:255-9.
- [Google Scholar]
- Epidemiological and entomological correlation of malaria transmission in an air force station. Med J Armed Forces India. 2001;57:191-3.
- [Google Scholar]
- Malaria on the move: ecological considerations for the armed forces. Med J Armed Forces India. 2007;63:112-4.
- [Google Scholar]
- National Vector Borne Disease Control Programme (NVBDCP) In: Health bulletin for ASHA on prevention and control of vector borne diseases: malaria, Bulletin 4. Delhi: NVBDCP; 2007.
- [Google Scholar]
- WHO. In: Assessment of therapeutic efficacy of antimalarial drugs for uncomplicated falciparum malaria in areas with intense transmission. Geneva, Switzerland: World Health Organisation; 1996. WHO/MAL/96.1077
- [Google Scholar]
- Regionwise pictorial keys to the female Indian anopheles. Bull Natl Soc India Mal Mosq Borne Dis. 1961;9:85-138.
- [Google Scholar]
- Pictorial identification key for Indian anophelines. Delhi: Malaria Research Centre (ICMR); 2005.
- [Google Scholar]
- Physiographic and entomologic risk factors of malaria in Assam, India. Am J Trop Med Hyg. 2004;71:451-6.
- [Google Scholar]
- Epidemiological investigation of forest malaria among GREF and army personnel. Med J Armed Forces India. 2006;62:30-2.
- [Google Scholar]
- Migration malaria associated with forest economy in Central India. Curr Sci. 2004;87:1696-9.
- [Google Scholar]
- Malaria problem and its control in north eastern states of India. J Commun Dis. 1995;27:262-6.
- [Google Scholar]
- Tribal malaria and its effects on Air Force station Amla and surrounding areas: an ecological study. In: Proc Natl Symp Tribal Health. Jabalpur, India: Regional Medical Research Centre for Tribals; 2006.
- [Google Scholar]
- Insecta: Diptera: Culicidae. State Fauna Series 7: Fauna of Tripura. . 2000;III:201-28.
- [Google Scholar]
- Studies on anopheline fauna and malaria incidence in Dhansiripar PHC of Dimapur, Nagaland. J Vect Borne Dis. 2004;41:67-71.
- [Google Scholar]






