Translate this page into:
Long-term follow up of clients from a community-based opioid substitution therapy programme in Manipur
+For correspondence: mkermode@unimelb.edu.au
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
Opioid substitution therapy (OST) involves replacing an illicit drug of dependence such as heroin, which is usually injected, with an orally administered, medically prescribed medicine such as methadone or buprenorphine in a supervised setting. The provision of OST to opiate dependant people is recognized in most Western countries as an effective component of the response to the dual public health problems of illicit drug use and HIV (approximately 10% of HIV infections worldwide are attributable to injecting drug use)1. Awareness of the need to mount a more effective response to prevent HIV transmission among injecting drug users (IDUs) is increasing2. Evidence that OST programmes substantially reduce engagement in HIV risk behaviours, overdoses and criminal activity, while at the same time improve the health of IDUs is strong3. However, it is estimated that only 8 per cent of IDUs globally are currently receiving OST, and the proportion is even lower in India45.
Despite evidence for OST effectiveness, and even though OST is endorsed by UNAIDS, UNODC and WHO,6 and methadone and buprenorphine are on the WHO Essential Medicines list,7 doubts about the wisdom of providing OST to IDUs remain widespread in India, where abstinence is often seen as the only legitimate treatment goal. Currently, there is a scarcity of evidence regarding outcomes of OST programmes in India or similar settings to either support or challenge these perceptions3.
The State of Manipur shares a long porous border with Myanmar, close to the Golden Triangle, and is characterized by a long-standing insurgent movement, substantial underdevelopment (29% live below the poverty line)8, and a major injecting drug use problem resulting in the highest HIV prevalence in the country (1.4% in 2009)9. Approximately 1-2 per cent of the population injects drugs10, and HIV prevalence among IDUs was reported to be 29 per cent in 200811. In addition to heroin, several pharmaceutical agents are injected, especially Spasmoproxyvon (a synthetic opioid analgesic containing dextropropoxyhene).
The HIV prevention response in Manipur is co-ordinated by the government through the National AIDS Control Organization (NACO) and the Manipur State AIDS Control Society (MACS). Alongside this, Avahan (Bill & Melinda Gates Foundation in India) has funded Project ORCHID to provide HIV prevention in selected districts of Manipur and the neighbouring s0 tate of Nagaland over a ten year period (2004-2013)12, delivered in the field by local non-government organizations (NGOs). Prior to initiation of this OST programme, OST was not available to IDUs in North East India, and even now OST coverage is limited.
In 2006, Project ORCHID was funded by DFID to resource selected local NGOs to deliver a community-based OST programme for opiate dependent IDUs in the States of Manipur and Nagaland. Sub-lingual buprenorphine is provided for registered IDUs seven days per week, and is administered by trained health care workers (mostly nurses) under the supervision of medical doctors, following a standardized protocol. The provision of OST through community-based NGOs rather than health system-based clinics differentiates this programme from most OST programmes in Western countries. The DFID funding for the OST programme expired at the end of 2007, and NACO has since assumed responsibility for its continuation. This study reports on field-based operational research undertaken in the State of Manipur to follow-up clients from this community-based OST programme 2-3.5 years after enrollment to determine their long-term outcomes.
During May 2006 to December 2007 detailed information regarding characteristics of the clients, engagement in risk behaviours, and outcomes of the programme were systematically collected as part of routine programme monitoring and evaluation. Data collection was conducted at intake, three months after entry into the programme, and at cessation of treatment regardless of the reason for cessation. Findings showed retention in OST in this resource-constrained setting was 63 per cent after six months, which was comparable to retention outcomes reported by a WHO collaborative study (approximately 70% overall, only 55% in Australia)13.
A random sample of 10 per cent of the 1853 clients enrolled in the Manipur OST programme between May 2006 and December 2007 was obtained 2-3.5 years later in December 2009 (n=185). The sampled clients were actively followed up through eight implementing NGOs to determine the long-term outcomes. Possible outcomes were classified as: abstinent (client is no longer enrolled in OST and has not returned to former pattern of injecting drug use); currently enrolled in the OST programme; relapsed (client is no longer enrolled in OST and has resumed injecting drug use); and expired. The outcomes were ascertained for each sampled client individually by examining NGO registers, individual client records, and talking with outreach workers and peer educators who work directly with IDU clients. As IDUs in North East India tend to remain living with their families, they are not highly mobile, and communities are relatively small and geographically isolated, so identifying current outcomes for individual clients was feasible.
The data presented here only captured the status of the sampled clients in December 2007 and December 2009, and it was not possible to show the extent to which they left and re-entered the programme in the intervening years. No follow up information was available on the December 2009 outcomes for 39 (21%) due to loss of contact between the client and the NGO workers.
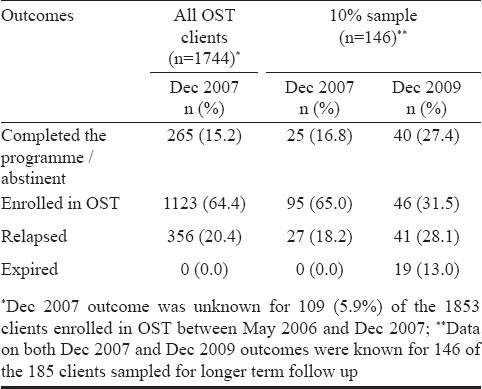
The Table presents the outcomes for the entire group of OST clients as of December 2007, and the sampled OST clients for December 2007 and December 2009. The proportion of sampled clients who were abstinent at the time of follow up was higher (27.4%) compared with the proportion who had completed the programme (the client had withdrawn from buprenorphine through a negotiated, gradual reduction in dose, and had not returned to his former pattern of injecting drug use at the time of being discharged from the OST programme) by December 2007 (16.8%). In total, 59 per cent of the sample had a positive outcome (abstinence or in OST treatment) when followed up in December 2009.
The Fig. presents the outcome status for the OST clients in December 2009 disaggregated by their outcome status in December 2007. These findings highlight the fact that OST clients tend to cycle between OST, relapse and abstinence over time. However, the overall trend in what is well-recognised as a chronic relapsing condition is positive for IDUs enrolled in OST. Approximately two-thirds (64.0%) of those who had ceased treatment due to relapse by December 2007 had either re-engaged in OST or were abstinent in December 2009. Conversely, 26.1 per cent of those who completed the programme by December 2007 were back in OST treatment in December 2009, and a further 26.1 per cent had relapsed. However, it is noteworthy that almost 40 per cent of those who had completed the programme by December 2007 were abstinent in 2009. These findings highlight that the benefits of participation in the OST programme are not only immediate13 but also long-term. The fact that 13 per cent of the sample had expired at the time of follow up highlights the heavy burden of mortality associated with drug use.
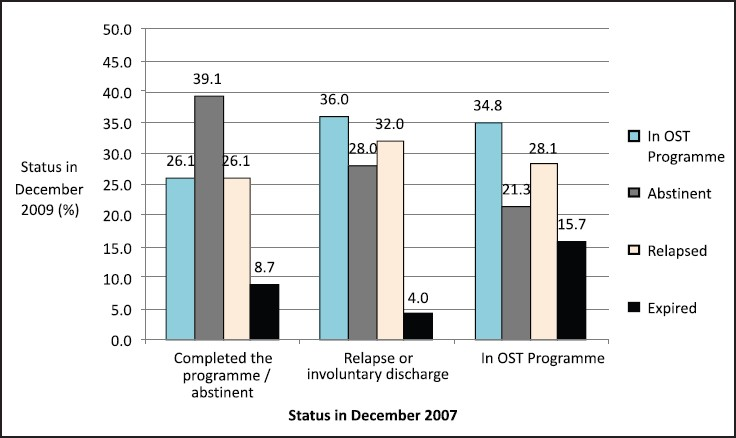
- Long-term outcomes in December 2009 by status in December 2007 (n=146).
These findings have relevance to other parts of India and Asia where injecting drug use is common, and are a first step towards filling the gap in knowledge regarding the effectiveness of community-based OST programmes delivered in resource-constrained settings. A longitudinal prospective cohort study to systematically follow a cohort of OST clients over time would provide more rigorous evidence regarding outcomes, impact of different dosing schedules, social and economic benefits, programme costs and cost-effectiveness, and the extent to which clients are cycling in and out of the programme. Additionally, it would be useful to follow clients who cease treatment to compare the benefits of staying in treatment over those of leaving, and to compare the effectiveness of community-based versus clinic-based OST delivery in similar resource constrained settings.
Acknowledgment
The participating NGOs who assisted with follow up of the OST clients and Drs B. Langkham, B. Aibannangkiew and B. Lyngdoh who read the manuscript and gave helpful feedback. This work was funded by the Bill & Melinda Gates Foundation, Washington DC.
References
- HIV prevention, treatment, and care services for people who inject drugs: a systematic review of global, regional, and national coverage. Lancet. 2010;375:1014-28.
- [Google Scholar]
- Key findings from the WHO collaborative study on substitution therapy for opioid dependence and HIV/AIDS. Addiction. 2008;103:1484-92.
- [Google Scholar]
- Prevention of HIV infection for people who inject drugs: why individual, structural, and combination approaches are needed. Lancet. 2010;376:285-301.
- [Google Scholar]
- A situation update on HIV epidemics among people who inject drugs and national responses in South-East Asia region. AIDS. 2009;23:1405-13.
- [Google Scholar]
- WHO, UNODC, UNAIDS. In: Technical guide for countries to set targets for universal access to HIV prevention, treatment and care for injecting drug users. Geneva: WHO; 2009.
- [Google Scholar]
- WHO. 16th WHO Model List of Essential Medicines. Available from: http://www.who.int/medicines/publications/essentialmedicines/en
- [Google Scholar]
- Ministry of Development of North Eastern Region and North Eastern Council. In: North Eastern Region vision 2020. New Delhi: Government of India; 2008.
- [Google Scholar]
- NACO (National AIDS Control Organization) 2010. HIV declining in India; New infections reduced by 50% from 2000-2009; Sustained focus on prevention required. Press release 1 Available from: http://www.nacoonline.org/
- [Google Scholar]
- Containing HIV/AIDS in India: The Unfinished Agenda. Lancet Infect Dis. 2007;6:508-21.
- [Google Scholar]
- WHO SEARO. In: Report on people who inject drugs in the South-East Asia region. New Delhi: WHO; 2010.
- [Google Scholar]
- Avahan. In: From hills to valleys - Avahan's HIV prevention programs among injecting drug users in Northeast India. New Delhi: Bill & Melinda Gates Foundation; 2009.
- [Google Scholar]
- Opioid substitution therapy in Manipur and Nagaland, north-east India: operational research in action. Harm Reduction J. 2010;7:29.
- [Google Scholar]





