Translate this page into:
Lichenoid skin lesions & mucosal erosions as a paraneoplastic syndrome
*For correspondence: ajkanwar1948@gmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
A 65 year old male, a known case of chronic lymphocytic leukemia, presented to the department of Dermatology, Venereology and Leprology, Postgraduate Institute of Medical Education and Research (PGIMER), Chandigarh, India in January 2012 with a three months history of painful oral and genital erosions, conjunctival congestion and hoarseness of voice. Simultaneously he developed multiple flaccid vesicles and crops of itchy, violaceous, mildly scaly papules and plaques over face, trunk and upper extremities (Fig. 1). Skin biopsy showed upper dermal lichenoid infiltrate and necrotic keratinocytes. Direct immunofluorescence (IF) of perilesional skin showed cell surface and basement membrane zone deposits of IgG (Fig. 2a). Intercellular IgG deposits were also demonstrated by indirect IF using normal human skin section (1:40; not in Fig. 2b) and rat bladder transitional epithelium (1:10) (Fig. 2b). On immunoblotting, patient's serum reacted with the 210 kDa envoplakin and 190 kDa periplakin. A diagnosis of paraneoplastic pemphigus (PNP) was made and the patient was treated with oral corticosteroids and intravenous rituximab but had poor response to therapy. The patient died of uncontrolled disease three months after the initial presentation.

- Violaceous, mildly scaly, discrete to confluent papules and plaque over the back.
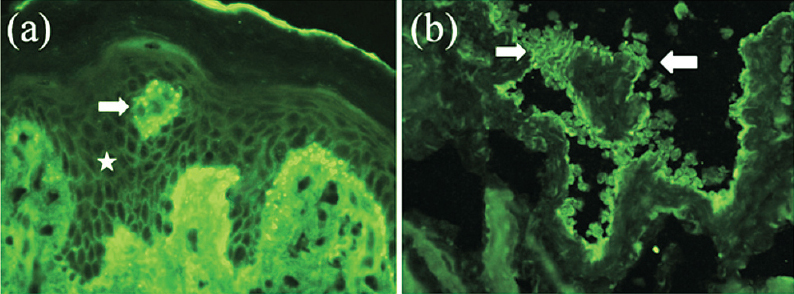
- (a). Direct immunofluorescence of perilesional skin section showing IgG deposits on cell surface (star) and basement membrane zone (arrow). The arrow (→) points to a obliquely cut dermal papillae. (b). Indirect immunofluorescence of rat bladder section, showing positive IgG reactivity with the transitional epithelium over 1:10 titre (both arrows) 400x.
PNP is a rare paraneoplastic dermatosis usually seen in association with haematological malignancies1. The cutaneous manifestations vary form a spectrum of at least five different clinical and immunopathological variants2. PNP differs clinically from classical pemphigus by presence of intractable stomatitis, inflammatory lesions in association with blisters and association with internal malignancy. In nearly one third of cases, PNP precedes the diagnosis of internal malignancy and acts as a cutaneous marker3. Conversely, a diagnosis of PNP should always be considered in patients with known haematological malignancies, who develop severe, intractable mucosal erosions or cutaneous blisters and lichenoid plaques.
References
- Neoplasms associated with paraneoplastic pemphigus: a review with emphasis on non-hematologic malignancy and oral mucosal manifestations. Oral Oncol. 2004;40:553-62.
- [Google Scholar]
- Classification, clinical manifestations, and immunopathological mechanisms of the epithelial variant of paraneoplastic autoimmune multiorgan syndrome: a reappraisal of paraneoplastic pemphigus. Arch Dermatol. 2001;137:193-206.
- [Google Scholar]
- Paraneoplastic pemphigus/paraneoplastic autoimmune multiorgan syndrome. Int J Dermatol. 2009;48:162-9.
- [Google Scholar]





