Translate this page into:
Know the less known: Diffuse leptomeningeal glioneuronal tumour
*For correspondence: drarpitasahu@gmail.com
-
Received: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
A three year old girl†, presented to the department of Neuro-Oncology, Tata Memorial Hospital, Mumbai, India, in September 2019, with drowsiness, drooling of saliva and lower limb weakness, underwent non-contrast enhanced computed tomography (NECT) of brain showing diffuse hypodensity of the white matter involving cerebellum, bilateral basal ganglia and white matter (Fig. 1A). Magnetic resonance imaging (MRI) brain showed multiple tiny T2-hyperintense lesions in the vermis, both cerebellar hemispheres (Fig. 1B), deep grey nuclei with mild hydrocephalus, and a small T2-hyperintense lesion (Fig. 1C and D) in the cervical spine. Diffuse leptomeningeal enhancement along tentorium and Sylvain fissure (Fig. 1E) was observed, in the frontal lobe (Fig. 1F) with tiny nodular enhancing lesions along the cerebellar folia (Fig. 1E). Pial enhancement was seen along the upper cervical spine (Fig. 1F). The patient underwent craniotomy and biopsy. Haematoxylin and eosin-stained slides showed normal cortical brain parenchyma with tumour in the leptomeningeal location adherent to pial surface (Fig. 2A-C). Tumour showed moderate cellularity composed of elongated cells (Fig. 2D). On immunohistochemistry, MIB-1 labelling index was approximately 2-3 per cent (Fig. 3). Diagnosis was diffuse leptomeningeal glioneuronal tumour (DLGNT), not otherwise specified.

- (A) Non-contrast enhanced computed tomography (NECT) brain-irregular hypodensity in cerebellum (white). (B) Magnetic resonance imaging showing axial T2-weighted-multiple tiny T2-hyperintense lesions in the cerebellar hemisphere (red). (C and D) Sagittal and coronal T2-weighted-small T2 hyperintense intramedullary lesion within cervical cord in yellow and blue. (E) Axial T1C - tiny nodular enhancing lesions along cerebellar folia and diffuse leptomeningeal enhancement along tentorium cerebelli (purple) and along Sylvian fissure (black). (F) Sagittal T1C - leptomeningeal in the frontal lobe (yellow) and diffuse pial enhancement in the cervical cord (green), non-enhancing cervical cord lesion (orange).
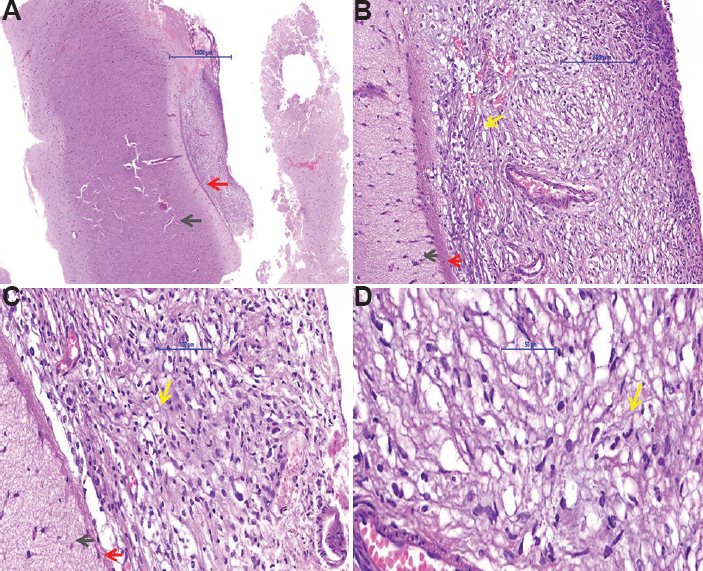
- Piamater with cortex biopsy specimen slide (A, H and E, ×2; B, H and E, ×10 and C, H and E, ×20) showing cortical normal brain parenchyma shown with black arrow, pial gliosis shown with red arrow, blood vessels shown with grey arrow and elongated tumour cells shown with yellow arrow. (D) Tumour area with low-to-moderate cellularity composed of elongated cells shown with yellow arrow and a few clear cells. Mitosis was not seen (H and E, ×40).
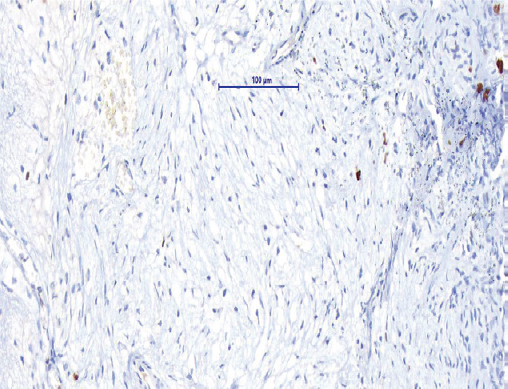
- MIB 1 immunohistochemistry staining showing MIB-1 labelling index approximately 2-3 per cent.
The patient underwent ventriculoperitoneal shunt relieving intracranial hypertension and palliative chemotherapy with carboplatin and vincristine. After completion of 12 wk of chemotherapy, in December 2019, follow up MRI revealed stable disease. The patient developed spasticity of the left lower limb, and was continued with six more months of chemotherapy on low-grade glioma protocol with physiotherapy.This diffuse leptomeningeal type of presentation of brain tumour is uncommon and can mimic infective meningitis.
Acknowledgment:
Authors acknowledge Dr Epari Sridhar, Professor, Department of Pathology, Tata Memorial Hospital, Mumbai, for providing the histopathology slides.
Conflicts of Interest: None.





