Translate this page into:
Is cure of HIV infection in sight?
* For correspondence: rparanjape@nariindia.org
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
The very recent case of HIV cure in a baby flagged on March 3, 2013 is an important benchmark in HIV research. Doctors at the Johns Hopkins Children's Center, USA, announced this as a case of ‘functional cure’, meaning that the virus did not rebound even after discontinuation of the antiretroviral treatment (ART)1. The baby, born in Mississippi, was detected to be HIV infected by HIV DNA and RNA testing on 2nd day of life. She was put on ART soon after the diagnosis at about 30 h after birth and continued until 18 months of age. HIV plasma viral load tests for the child were positive on several occasions before reaching an undetectable level at 29 days. HIV remained undetectable at 26 months despite ART being stopped at 18 months. Although some ultrasensitive tests could detect low copies of the virus in her cells, standard clinical assays like plasma viral load, peripheral blood mononuclear cells (PBMC) DNA, and HIV-specific antibodies failed to detect traces of the virus confirming a state of ‘functional cure’. This is quite unusual as it is expected that the virus would rebound after the ART is discontinued. This is because the antiretroviral drugs which are available currently control replicating HIV but do not have any effect on latent form of HIV integrated in host genome, hence, cannot cure HIV infection.
HIV reservoir and HAART
The latent form of HIV is mainly harboured in resting cells constituting HIV reservoir2. These cellular reservoirs contain integrated HIV in proviral form and are located throughout the body, including the brain, lymphoid tissue, bone marrow, and the gastrointestinal tract. These cells do not express HIV antigens on their surfaces and hence cannot be recognized by body's immune defences. Being not sensitive to anti-HIV drugs, these persist even in the presence of highly active antiretroviral therapy (HAART). HIV from these reservoirs resumes its replication once the drug pressure is removed. Hence, the drugs have to be taken life-long with regular dosages and any breach in adherence to the treatment regimen can lead to viral rebound as well as development of drug resistant mutations making those drugs ineffective against HIV. Apart from the risk of development of drug resistance, the patients may also have to suffer from some of the side effects of these drugs.
Strategies towards HIV cure
Since antiretrovirals need to be administered lifelong and are fraught with associated toxicity and emergence of resistance, there are efforts worldwide for cure from HIV whereby not only the replicating but also the latent form of HIV is eliminated from the body. This kind of a cure where every single infected cell including viral reservoir is removed is known as a ‘sterilising cure’3. Since the sterilizing cure is difficult to achieve, a novel concept of ‘functional cure’ has been put forth which essentially means controlling HIV replication effectively by keeping the virus dormant even without the use of long-term drugs. This is an important concept especially in the view of the limitations of life-long antiretroviral therapy for HIV infection.
Strategies attempted so far for HIV cure consist of purging of HIV reservoir in presence of anti-HIV drugs, bone marrow transplantation and gene therapy4. The aim of purging the HIV reservoir is to activate resting infected CD4 cells (CD4 lymphocytes harbouring latent HIV virus) which are expected to undergo apoptosis15. The cells also express HIV antigens on their surfaces and hence are destroyed by the immune system. The new HIV particles produced are also expected to be tackled by the ongoing antiretroviral treatment (Fig. 1). Initial attempts to “flush out” the virus by activation of latently infected resting CD4+ T cells with the administration of interleukin (IL)-2 and/or anti-CD3 monoclonal antibodies were ultimately unsuccessful, probably because of its inability to reach all of the latent viral reservoirs and the toxicity of the regimen678. A more promising approach for complete viral clearance now being attempted is by using small molecules with pharmacological properties that allow them to access the viral reservoirs and to specifically reactivate the latent proviruses without causing cellular activation9. The concept of small molecule activation of latent HIV-1 has been tested in many in vitro studies using mainly the histone deacetylase (HDAC) inhibitors and protein kinase C (PKC) activators101112. Unfortunately, clinical studies of valproic acid, which is a histone deacetylase (HDAC) inhibitor, have not shown a consistent decrease in the latent reservoir1314. As against valproic acid which is weak in inducing HIV activation, newer HDAC inhibitors like vorinostat, belinostat and givinostat have been found to be more effective at targeting specific HDACs for HIV-1 expression15 and are thought to be promising agents for HIV eradication. Scientists at the National AIDS Research Institute (NARI), Pune, India, also tried to activate latent reservoirs with HIV antigens16. These infected cells after activation produce IL-10, an immunosuppressive cytokine, which might be helping in persistence of these cells after activation indicating possible role of IL-10 blockade when such an activation is attempted (Fig. 2). Several studies are ongoing with the anti-latency agents demonstrating their efficacy in HIV activation, but their success in eliminating the reservoir as well as reaching deep lymphoid tissues, which harbour major HIV reservoir, needs to be determined. Newer delivery systems using nanoparticles or liposomes would also be helpful in targeting these drugs to deeper HIV reservoirs17.
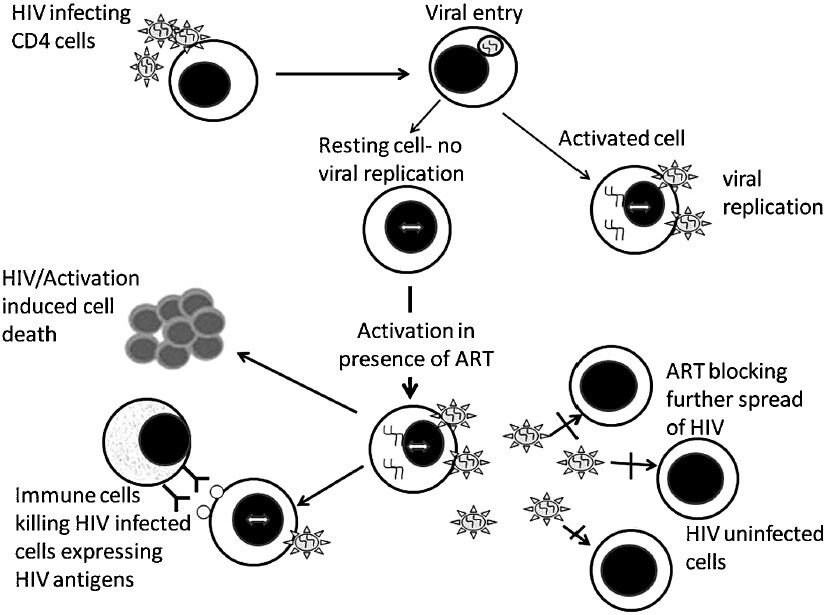
- Activation of latent HIV as a strategy for HIV cure: Anti-latency agents used for activating latent HIV proviruses present in CD4+ T cells cause cell death induced by HIV as well as by cellular activation and immune cell mediated lysis. These agents are to be used in combination with HAART to prevent further HIV spread to uninfected CD4+ T cells.
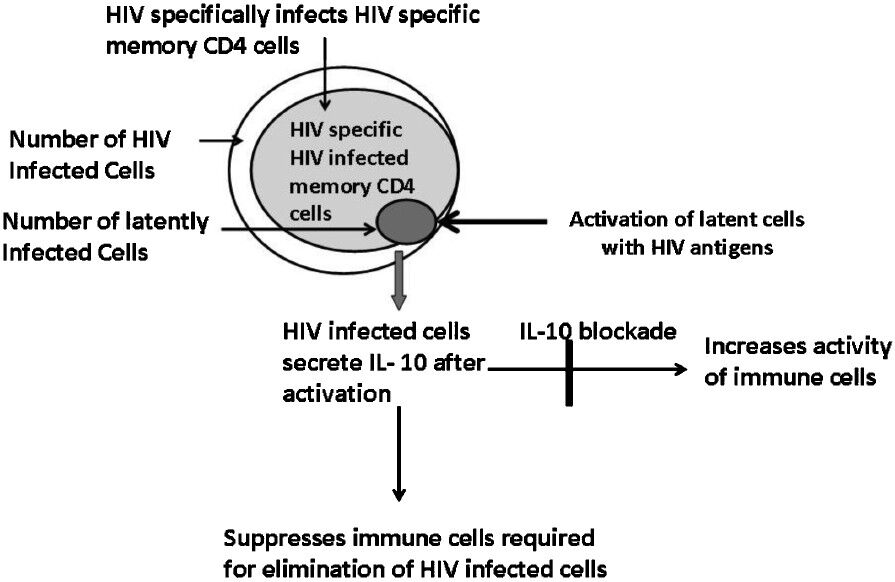
- Activation of latent HIV by antigens- Findings of the NARI study: Since the pool of HIV infected cells consists of HIV specific CD4 memory cells, it is possible to reativate HIV from these cells with HIV antigens. These cells also include HIV reservoirs which are essentially latently infected cells. HIV infected cells predominately secrete IL-10 upon reactivation, which can suppress immune cells required for elimination of HIV infected cells. Hence, IL-10 blockade is essential to eliminate these cells by activation.
“Berlin case” report
Bone marrow transplantation to replace most of the cells in body with the cells resistant to HIV infection is also considered as one of the ways of achieving HIV cure. A rare genetic mutation called as delta 32 in CCR5 gene, which encodes CCR5 (a co-receptor for HIV entry in CD4+ cells), results in conferring resistance to HIV infection. A well known “Berlin case” exemplifies HIV cure by bone marrow transplantation from a donor having delta 32 mutation18. The bone marrow transplantation was done as a treatment for leukaemia to this HIV infected patient. Twenty months after the procedure, no trace of HIV could be found in the recipient's body and in 2008, doctors announced about cure of HIV in this patient. However, bone marrow transplantation is dangerous, expensive as well as not a feasible approach for widespread use as a cure and hence is usually used as a last resort in treating life-threatening diseases. But it does raise hope for the related approaches. Gene therapy could be another way of inducing delta 32 mutation in the existing body cells and thus would confer the same sort of protection against HIV as transplantation from donor with delta 32 mutation. Research in this area is in its very early stages and may be many years before a useful treatment is found, if at all.
Boston patients report
Two adult patients from Boston, USA, have also been reported to be cured from HIV after they received stem cell transplants to treat lymphoma19. These cases differed from the “Berlin case” as the stem cells transplanted in them were without the protective mutation. It is thought that the transplanted cells must have been protected from infection by the antiretroviral drugs taken during cancer treatment. Also, graft-versus-host reaction was thought to have cleared patients’ HIV reservoirs, resulting in HIV cure in them. Viral unbound was noted in both of these patients indicating failure of this therapy as presented in a recent conference at Florida, USA, on HIV persistence.
LTNPs as a model of functional cure
Elite controllers (EC) and long term non progressors (LTNPs) constitute ideal models for understanding mechanisms responsible for spontaneous virologic control and may provide clue for functional cure20. Elite controllers typically have no detectable viral particles in blood even in absence of ART and LTNPs, although may not have undetectable viral levels, can control disease progression and remain asymptomatic for prolonged periods, ideally for more than 10 years, without ART. However, this population is heterogeneous and may have differing mechanisms for such a viral control. There could be many viral, immunologic or genetic factors, which could contribute to viral control2122. Determining the role of viral fitness versus host factors in these patients is critical as it would have possible implications in devising strategies for viral control. There are several studies reporting major gene mutations in viral isolates from LTNPs indicating reduced viral fitness responsible for the possible control of the infection. However, this attenuation itself can result from strong immune responses pressurizing the virus to undergo mutations for rendering it weaker23. Hence, host barriers would be more important for maintaining this long term host-virus quasi-equilibrium in most LTNPs with virus attenuation reflecting host's selective pressure. Moreover, elite controllers would also have viruses transmitted from progressors as demonstrated in one study addressing the importance of host factors in the control of infection24. Associations of host genetic factors like HLA-B57, HLA-B27, delta32 CCR5 and HLA-C/KIR interactions have been demonstrated in genome-wide comparisons between LTNP and progressors25. However, these have been found to account for only around 20 per cent of the variability in the control26. Association of genetic variants of major histocompatibility complex (MHC) Class I genes with control of viral load and disease progression has been shown to be mediated through modulation of the response of CD8+ and natural killer (NK) cells27. CD8+ T cells have been extensively studied in control of HIV-1 infection, and strong evidence supports their key role in delaying disease progression2829. HIV-1-specific CD8+ T cells from EC were found to be qualitatively superior in terms of proliferative capacity, cytotoxic activity and polyfunctionality to those from patients with progressive disease282930. Apart from CD8 cells, role of CD4 cells, NK cells and antibody dependent cell mediated toxicity (ADCC) has also been implicated in viral control in several studies25. Identification of such immunological mechanisms responsible for viral control would be important for developing vaccines or immune therapies for viral control.
“Visconti cohort” report
Functional cure can also result from limiting the size of HIV reservoir by initiating ART soon after the HIV infection, which was possibly responsible for cure in the recent “Mississippi case”1. Similarly, functional cure has also been reported in a cohort of 14 adult French patients known as the ‘Visconti cohort’31. The patients started taking antiretrovirals soon after they became infected. They stopped taking ART after three years of medication. But instead of viral resurge, they also were able to maintain low levels of the virus in their systems for an average of seven years. Thus, the cohort showed that the ART initiation soon after HIV infection can lead to reduction in viral reservoir making functional cure possible.
Conclusions
Elimination of HIV reservoirs is the basis for HIV cure and different anti-latency agents for its elimination are being attempted worldwide. Alternatively, immune therapies for keeping the reservoirs under control leading to functional cure are also being investigated using LTNPs and ECs as models. However, it appears that it would take a long time for these strategies to become available for clinical use. Limiting development of HIV reservoirs by early initiation of ART seems to be a possible approach for functional cure as is evident from these recent reports. However, these reports are in isolation and need to be confirmed on a larger number of patients. Initiation of ART immediately after infection may not be possible in adult patients as they may not access health care system that soon and also it is not feasible to detect infection immediately after exposure to the virus. But, it certainly will change the way newborns of infected mothers are treated all over the world. Hence, at present studies are being planned to see if early testing and aggressive treatment can work for other children as well. Unlike the bone marrow transplantation in Berlin case, the Mississippi treatment is a practical approach for HIV cure and could become a new standard of care. Treating the children for only a year or two would also be cost-effective than waiting for CD4 counts to drop and giving the treatment lifelong which is being practiced currently.
Thus, to conclude, although HIV cure has been thought as an impossible target to achieve by many scientists worldover, these Mississippi and Berlin cases have resulted in restoring our belief in HIV cure. One has to be optimistic for HIV cure so as to ultimately develop strategies to achieve it.
References
- Functional HIV cure after very early ART of an infected infant. Available from: wwwretroconferenceorg/2013b/Abstracts/47897htm2013
- [Google Scholar]
- Redefining the viral reservoirs that prevent HIV-1 eradication. Immunity. 2012;37:377-88.
- [Google Scholar]
- Reduction of the HIV-1-infected T-cell reservoir by immune activation treatment is dose-dependent and restricted by the potency of antiretroviral drugs. AIDS. 2000;14:659-69.
- [Google Scholar]
- Pilot study of the effects of intermittent interleukin-2 on human immunodeficiency virus (HIV)-specific immune responses in patients treated during recently acquired HIV infection. J Infect Dis. 2002;185:61-8.
- [Google Scholar]
- Effects of interleukin-2 plus highly active antiretroviral therapy on HIV-1 replication and proviral DNA (COSMIC trial) AIDS. 2002;16:1479-87.
- [Google Scholar]
- OKT3 and IL-2 treatment for purging of the latent HIV-1 reservoir in vivo results in selective long-lasting CD4+ T cell depletion. J Clin Immunol. 2001;21:218-26.
- [Google Scholar]
- Small-molecule screening using a human primary cell model of HIV latency identifies compounds that reverse latency without cellular activation. J Clin Invest. 2009;119:3473-86.
- [Google Scholar]
- Administration of vorinostat disrupts HIV-1 latency in patients on antiretroviral therapy. Nature. 2012;487:482-5.
- [Google Scholar]
- Activation of latent HIV-1 expression by protein kinase C agonists. A novel therapeutic approach to eradicate HIV-1 reservoirs. Curr Drug Targets. 2011;12:348-56.
- [Google Scholar]
- Histone deacetylase inhibitor Scriptaid reactivates latent HIV-1 promoter by inducing histone modification in in vitro latency cell lines. Int J Mol Med. 2010;26:265-72.
- [Google Scholar]
- Valproic acid in association with highly active antiretroviral therapy for reducing systemic HIV-1 reservoirs: results from a multicentre randomized clinical study. HIV Med. 2012;13:291-6.
- [Google Scholar]
- Prolonged valproic acid treatment does not reduce the size of latent HIV reservoir. AIDS. 2008;22:1125-9.
- [Google Scholar]
- Histone deacetylase inhibitors for purging HIV-1 from the latent reservoir. Mol Med. 2011;17:466-72.
- [Google Scholar]
- Short communication: HIV antigen-specific reactivation of HIV infection from cellular reservoirs: implications in the settings of therapeutic vaccinations. AIDS Res Hum Retroviruses. 2012;28:835-43.
- [Google Scholar]
- Evidence for the cure of HIV infection by CCR5Delta32/Delta32 stem cell transplantation. Blood. 2011;117:2791-9.
- [Google Scholar]
- Stem-cell transplants may purge HIV- Nature News. Available from: http://wwwnaturecom/news/stem-cell-transplants-may-purge-hiv-113297
- [Google Scholar]
- “Elite controllers” provide clues to keeping HIV infection in check. Interview by Tracy Hampton. JAMA. 2012;308:328-9.
- [Google Scholar]
- Human immunodeficiency virus type 1 long-term non-progressors: the viral, genetic and immunological basis for disease non-progression. J Gen Virol. 2011;92:247-68.
- [Google Scholar]
- Transmission of human immunodeficiency virus type 1 from a patient who developed AIDS to an elite suppressor. J Virol. 2008;82:7395-410.
- [Google Scholar]
- Innate and adaptive immunity in long-term non-progression in HIV disease. Front Immunol. 2013;4:95.
- [Google Scholar]
- Lessons to be learned from natural control of HIV - Future directions, therapeutic, and preventive implications. Front Immunol. 2013;4:162.
- [Google Scholar]
- A whole-genome association study of major determinants for host control of HIV-1. Science. 2007;317:944-7.
- [Google Scholar]
- HIV-specific CD8+ T cell proliferation is coupled to perforin expression and is maintained in nonprogressors. Nat Immunol. 2002;3:1061-8.
- [Google Scholar]
- HIV controllers exhibit potent CD8 T cell capacity to suppress HIV infection ex vivo and peculiar cytotoxic T lymphocyte activation phenotype. Proc Natl Acad Sci USA. 2007;104:6776-81.
- [Google Scholar]
- HIV nonprogressors preferentially maintain highly functional HIV-specific CD8+ T cells. Blood. 2006;107:4781-9.
- [Google Scholar]
- Post-Treatment HIV-1 Controllers with a Long-Term Virological Remission after the Interruption of Early Initiated Antiretroviral Therapy ANRS VISCONTI Study. PLoS Pathog. 2013;9:e1003211.
- [Google Scholar]





