Translate this page into:
Injecting drug use & HIV prevalence among female sex workers: Evidence from the National Integrated Biological & Behavioural Surveillance, India
For correspondence: Dr Sanjay Mehendale, P.D. Hinduja National Hospital & Medical Research Centre, Mumbai 400 016, Maharashtra, India e-mail: dr_sanjay.mehendale@hindujahospital.com
-
Received: ,
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Female sex workers (FSWs) who inject drugs (FSW-IDs) have a higher risk of HIV infection and transmission. Understanding the socio-demographic characteristics and other risk behaviours among FSW-IDs will help in strengthening targeted interventions for HIV prevention and management. In the present study, the HIV prevalence, associated socio-demographic characteristics and risk behaviours among FSWs who injected drugs (FSW-IDs) and those who did not ID (FSW-NIDs) was determined in India.
Methods:
The national cross-sectional, community-based, integrated biological and behavioural surveillance was conducted in 2014-2015 at 73 randomly selected FSW domains across 28 States and Union Territories in India. The sample size was fixed at 400 for each domain, and a probability-based sampling method was followed. The data were analyzed by logistic regression methods.
Results:
Data from 27,007 FSWs were included in the analysis, of which 802 (3%) were FSW-IDs. HIV prevalence among FSW-IDs was significantly higher than that in FSW-NIDs (4.5 vs. 1.9%). Univariate analysis showed that factors significantly associated with higher HIV prevalence among FSW-IDs were older age, sex work as the only source of income, dissolved marriage, living with a sex worker, urban locality of sex work and consumption of alcohol or oral drugs. In multivariable analysis, factors such as older age of FSW-IDs (35 yr and above), having a dissolved marriage and sex work being the only source of income were observed to be independently and significantly associated with higher HIV prevalence.
Interpretation & conclusions:
Scaling up the HIV preventive interventions for FSW-IDs, such as facilitating awareness and improved access to needle and syringe exchange programme (NSEP) and opioid substitution therapy (OST), encouraging safe sex and injecting practices, educating on the harmful effects of alcohol and drugs and providing alternative vocation options to secure their financial needs are several strategies that may reduce HIV transmission among FSWs.
Keywords
Female sex worker
HIV prevalence
India
injecting drug user
risk behaviours
HIV epidemic is highly heterogeneous across the States and districts of India and is more concentrated in the high-risk groups (HRGs) that include female sex workers (FSWs), men who have sex with men (MSM), injecting drug users (IDUs) and transgenders (TGs). The population living with HIV/AIDS in India was estimated to be 2.3 million in 2019, of which 44 per cent were females1. The highly vulnerable HRG population can potentially transmit the disease to the general population, as the heterosexual route is the major mode of HIV transmission in India2. While the adult HIV prevalence was estimated to be 0.22 per cent among HRGs in 2017, IDU had the highest HIV prevalence of 6.26 per cent, followed by TG (3.14%), MSM (2.69%) and FSW (1.56%). HIV epidemic in India is concentrated with substantially higher HIV prevalence in HRGs than in the general population (GP)3. Hence, limiting the disease spread among the HRGs and bridging populations was perceived to be the most effective method to prevent HIV transmission to the general population2.
Initially, HIV preventive interventions were focused on FSWs and TGs and were later gradually extended to MSM and IDUs, as a surge in HIV prevalence in these populations was identified. However, the initial programmes focused on creating awareness on HIV and promoting condom usage. The introduction of ‘Test and Treat’ policy in 2017 significantly revamped the strategies for targeted interventions (TIs) among HRG45. Consequently, the estimated HIV incidence per every 1000 uninfected population declined from 0.64 in 1995 to 0.05 in 20191. However, from 2010 to 2019, the decline in the incidence rate slowed down, as new infections declined only to about 37 per cent since 20101. Hitherto, the incidence rate continues to be much higher among the HRGs as compared to the general population, and zero transmission is still unachievable. Hence, there is a need for disaggregated analysis to facilitate decentralized, group-specific interventions1. Demographic and socio-culturally relevant risk factors for HIV infection among the HRGs and the risk structure of transmission need to be explored with a view to design group-specific interventional strategies6. Globally, studies suggest that a considerable proportion of FSWs are IDUs or vice versa, thus increasing their risk of HIV acquisition through yet another route of transmission. These studies have reported the risk factors associated with HIV transmission among those females who are both sex workers as well as IDUs7891011. While it is evident that injecting drug usage is a risk factor for HIV infection, the IDU interventions in India focus primarily on male IDUs, and females are often ignored owing to their smaller numbers. Nonetheless, limited studies on female IDUs have been reported in the northeastern regions of India, and these cannot be considered representative of the entire nation7,12,13.
Hence, in this study, the data from the National Integrated Bio-Behavioural Surveillance (IBBS)14 was analyzed to determine the HIV prevalence among FSW-IDs and FSW-NIDs in India. In addition, we have analyzed the association between various socio-demographic features and risk behaviour among FSW-IDs and FSW-NIDs were also analysed in the context of HIV prevalence.
Material & Methods
Surveillance design and methodology: The IBBS14 conducted in 2014-2015 in India was the first nationwide, large-scale, community-based, bio-behavioural surveillance among HRGs and bridge populations. Apart from estimating the HIV prevalence, the focus was also on collecting behavioural data among HRGs and bridge populations, which could be of programmatic importance.
The IBBS study was approved by the Ethics Committee of the NACO before the survey was undertaken. The IBBS survey was done after obtaining written informed consent from all the respondents. The voluntary nature of their participation was stressed upon giving clear information regarding the risks and benefits of their participation.
The data collected during the IBBS of FSW as part of IBBS 2014-2015 were used for this study. Self-identified FSWs aged 15 yr or more, who were engaged in consensual sex in exchange for cash/payment-in-kind in the previous month, were included in the survey. The study was carried out from October 2014 to November 2015 in 73 FSW domains (clusters) in India, with each sampled domain requiring three months to complete the study. The sampling domains selected to generate the bio-behavioural estimates were contiguous administrative geographical units spread over one or two districts. The domains covered in the study were randomly selected, from a total of 515 FSW domains prioritized for the targeted interventional programmes for FSWs by the National AIDS Control Organization (NACO) based on the reported size of the FSWs in all the domains.
The probability-based sampling method with a cluster sampling approach was adopted. A conventional cluster sampling approach was used for brothels or home-based FSWs, whereas a time location cluster sampling approach was used for mobile or dynamic street-based FSWs. The target sample size per domain was fixed at 40014. The targeted sample size could not be achieved in certain domains because of the non-availability of FSWs or a higher refusal rate than expected due to stigma or reluctance to identify themselves as FSWs. In all, 27,007 FSWs were enrolled from 73 sampling domains, covering 108 districts in 28 Indian States and Union Territories (UTs) of India.
The consented participants were interviewed with a questionnaire using a computer-assisted personal interview approach. The dry blood spot method was used to collect blood samples from the respondents, which were then tested for HIV in designated laboratories using the standard two-test protocol14. The first test was of high sensitivity using the MicroELISA HIV kit, and if the first test was positive, then the second test of high specificity was done using the SD Bioline HIV 1/2 3.0 kit. The detailed methodology, field monitoring and supportive supervision mechanism during data collection, ethical considerations including the informed consent process, weighing procedure and laboratory testing methods are available elsewhere14.
Measures:
Exposure: Injecting drug use - female sex workers who inject and did not inject drugs (FSW-IDs and FSW-NIDs): To identify the FSW-IDs, those who had answered yes to the question ‘Have you ever injected drugs for non-medical reasons in the last 12 months?’ were grouped as FSW-IDs and the rest were grouped as FSW-NIDs.
Outcome: HIV prevalence: Based on the results of the HIV tests, the HIV prevalence of the FSW in both groups was calculated as the percentage of those who tested positive for HIV infection out of the total FSW-IDs and FSW-NIDs.
Other covariates: Socio-demographic characteristics: Data on current age (in completed years), education status, marital status (e.g., single, unmarried, married, separated and divorced), co-partner (alone or living with family or spouse, sex worker, male partner, female friends and others), age of first sexual intercourse, duration of sex work and locality of sex work were considered.
Behavioural and psychosocial risks: These included type of sexual partners, frequency of condom usage and consumption of alcohol/oral drugs, alcohol consumption before or during sex, presence of sexually transmitted infection (STI) symptoms and having heard the term HIV. The respondents were asked about the type of their sexual partners (regular clients, occasional clients, regular non-paying partners and casual partners) and the consistency of condom usage with each of their partner types. Inconsistent condom usage was assessed by asking how often (every time, most of the time, sometimes and never) the respondent had used condoms during intercourse in the last month with each partner type. Those who answered most of the time or sometimes or never were coded as inconsistently using condoms. The respondents were asked whether they consumed alcohol and, if yes, whether they had consumed alcohol before or during sex. They were also asked whether they had consumed oral drugs in the last 12 months. The respondents were asked if they had any of the following symptoms suggestive of an STI: lower abdominal pain, foul-smelling vaginal discharge, burning pain during urination, genital ulcer/sore, swelling in the groin area and itching in the genital area. Those who had reported as having at least one of the symptoms were coded as having STI symptoms. Violence victimization was assessed by asking if the respondents had experienced physical and sexual violence at least once in the last 12 months. The respondents were also asked if they had ever heard the term ‘HIV’ to assess HIV awareness.
Data analysis: The unweighed proportions and HIV prevalence for the actual FSW sample size have been presented according to their status of injecting drug use. The socio-demographic and behavioural factors associated with the risk of HIV infection between the two groups of FSWs were analyzed by the Chi-square test and compared using risk ratios with 95% confidence intervals. Independent factors significantly associated with the HIV risk among the FSW-IDs were determined by logistic regression. All associated factors that were marginally significant at 5 per cent in the unadjusted logistic regression were selected for multivariable analysis. Factors with a P<0.05 were considered significant. IBM SPSS version 26.0 (IBM Corp., Armonk, NY, USA)15 was used for all analyses.
Participants’ time spent during the survey was compensated. Furthermore, all possible efforts were made to link the FSWs surveyed to Integrated Counselling and Testing Centres (ICTCs) to get their HIV status investigated, by providing them with referral cards. Similarly, any non-registered FSWs were referred to the nearest NGO (non-government organization) and were encouraged to utilize HIV prevention and control services.
Results
Of the 27,007 FSWs who participated in IBBS 2014-2015, 802 (3%) were FSW-IDs, and the rest were FSW-NIDs. The age of the FSW-IDs ranged from 16 to 59 yr with a median age of 29 yr, and that of FSW-NIDs ranged from 15 to 70 yr with a median age of 30 yr. The proportion and HIV prevalence for each subgroup based on their socio-demographic and behavioural profiles are presented in Table I.
| Variables | FSW-ID (n=802) | FSW-NID (n=26,205) | Risk raito# | ||||
|---|---|---|---|---|---|---|---|
| n | % | HIV | n | % | HIV | ||
| Age group (yr) | |||||||
| ≤24 | 196 | 24.4 | 3.1 | 5077 | 19.4 | 1.4 | 2.22 (0.98-5.05) |
| 25-34 | 407 | 50.7 | 2.9 | 13,203 | 50.4 | 1.9 | 1.59 (0.90-2.81) |
| ≥35 | 199 | 24.8 | 9.0 | 7925 | 30.2 | 2.4 | 3.77 (2.38-5.99)*** |
| Education | |||||||
| Literate (can read and write) | 559 | 70.1 | 4.1 | 17,357 | 66.3 | 1.5 | 2.67 (1.76-4.06)*** |
| Illiterate | 239 | 29.9 | 5.4 | 8820 | 33.7 | 2.7 | 2.02 (1.17-3.47)* |
| Source of income | |||||||
| Sex work alone | 377 | 47.0 | 6.1 | 10,726 | 41 | 1.8 | 3.48 (2.29-5.30)*** |
| Bar girl, beauty/massage parlour | 155 | 19.3 | 5.2 | 5207 | 19.9 | 2.1 | 2.47 (1.23-4.97)* |
| Otder tdan sex work@ | 269 | 33.5 | 1.9 | 10,252 | 39.2 | 2.0 | 0.92 (0.38-2.21) |
| Marital status | |||||||
| Married | 411 | 51.3 | 1.5 | 16,698 | 63.8 | 1.5 | 1.00 (0.45-2.22) |
| Unmarried | 223 | 27.8 | 4.0 | 4439 | 16.9 | 2.0 | 1.97 (1.05-3.74)* |
| Separated/widowed/divorced | 167 | 20.8 | 12.6 | 5054 | 19.3 | 3.4 | 3.73 (2.41-5.75)*** |
| Currently living | |||||||
| Alone | 120 | 15 | 3.3 | 3626 | 13.8 | 2.8 | 1.19 (0.45-3.18) |
| Witd family/spouse | 571 | 71.4 | 4.0 | 20,198 | 77.1 | 1.6 | 2.51 (1.68-3.76)*** |
| Witd sex worker | 54 | 6.8 | 13.0 | 602 | 2.3 | 3.5 | 3.34 (1.66-6.71)*** |
| Witd anotder male partner | 19 | 2.4 | 0.0 | 720 | 2.7 | 3.2 | - |
| Witd otder female friends | 34 | 4.3 | 5.9 | 584 | 2.2 | 2.7 | 2.08 (0.54-8.03) |
| Witd otders | 2 | 0.3 | 0.0 | 462 | 1.8 | 5.6 | - |
| Age of first sexual intercourse | |||||||
| ≤17 yr | 321 | 40 | 5.3 | 11,109 | 47.5 | 1.8 | 2.88 (1.78-4.67)*** |
| ≥18 yr | 481 | 60 | 4.0 | 12,298 | 52.5 | 2.1 | 1.88 (1.19-2.96)* |
| Duration of sex work | |||||||
| 0-1 yr | 54 | 6.7 | 3.7 | 1667 | 6.4 | 1.7 | 2.17 (0.55-8.49) |
| >1-10 yr | 469 | 58.6 | 4.5 | 16,038 | 61.3 | 1.8 | 2.40 (1.57-3.67)*** |
| >10 yr | 278 | 34.7 | 4.7 | 8477 | 32.4 | 2.1 | 2.16 (1.26-3.71)** |
| Locality of place of sex work | |||||||
| Rural | 102 | 12.7 | 0.0 | 5297 | 20 | 1.9 | - |
| Urban | 414 | 51.6 | 8.0 | 11,778 | 45.2 | 2 | 3.80 (2.72-5.30)*** |
| Botd | 286 | 35.7 | 1.0 | 9105 | 34.8 | 1.8 | 0.58 (0.19-1.80) |
| Experienced physical violence¥ | 342 | 42.6 | 4.7 | 6158 | 23.5 | 1.9 | 2.44 (1.47-4.07)*** |
| Experienced sexual violence∞ | 424 | 52.9 | 2.6 | 4423 | 17.0 | 1.9 | 1.33 (0.72-2.48) |
| Had occasional clients | 691 | 86.3 | 4.8 | 19,684 | 75.2 | 2 | 2.32 (1.66-3.25)*** |
| Inconsistent condom use^ | 300 | 43.4 | 4.3 | 5975 | 30.4 | 2.3 | 1.84 (1.08-3.13)* |
| Had regular clients | 716 | 89.3 | 4.7 | 21,249 | 81.1 | 1.9 | 2.48 (1.78-3.46)*** |
| Inconsistent condom use | 340 | 47.5 | 4.1 | 7563 | 35.6 | 2 | 2.01 (1.20-3.35)* |
| Had regular non-paying partner | 556 | 69.4 | 3.4 | 15,979 | 61 | 1.7 | 1.99 (1.28-3.11)** |
| Inconsistent condom use^ | 358 | 64.4 | 3.6 | 10,906 | 68.3 | 1.8 | 2.03 (1.18-3.46)* |
| Had casual partner | 392 | 48.9 | 1.8 | 5060 | 19.3 | 2 | 0.91 (0.44-1.89) |
| Inconsistent condom use^ | 215 | 54.8 | 2.3 | 2596 | 51.3 | 2.5 | 0.92 (0.39-2.17) |
| Consumed alcohol$ | 543 | 67.7 | 5.9 | 8158 | 31.1 | 2.6 | 2.24 (1.56-3.21)*** |
| Consumed alcohol before sex | 419 | 77.3 | 5.7 | 5420 | 66.4 | 2.6 | 2.12 (1.44-3.10)*** |
| Consumed oral drugs (ganja/heroine)$ | 386 | 48.1 | 7.0 | 949 | 3.6 | 1.8 | 3.90 (2.15-7.08)*** |
| STI symptoms (at least one) | 558 | 69.6 | 4.5 | 13,099 | 50 | 1.9 | 2.24 (1.53-3.30)*** |
| Heard HIV/AIDS | 726 | 90.5 | 4.5 | 22,848 | 93.3 | 1.9 | 2.31 (1.65-3.23)*** |
| HIV prevalence | 36 | 4.5 | 4.5 | 505 | 1.9 | 1.9 | 2.29 (1.66-3.18)*** |
Totals may not match due to non-response/don’t know; #Reference category non-injecting FSW’s; @Labours, business, service (Pvt./Govt.), hotel staff, etc.; $Consumed in the last 12 months; ¥Physical violence: physically beaten by someone (hurt, hit, slapped, pushed, kicked, punched, burned and but not using weapon) at least once in the last 12 months; ∞Sexual violence: Forced by someone in the last 12 months to have sexual intercourse; ^Not use of a condom at each sex act; P *<0.05; **<0.005; ***<0.001. STI, sexually transmitted infection; FSWs, female sex workers; FSW-ID, FSWs who inject drug; FSW-NID, FSWs who did not inject drug
Although the distribution of FSW-IDs and FSW-NIDs was comparable for various socio-demographic characteristics, the proportion of FSW-IDs practising risk behaviours was higher than that of FSW-NIDs. HIV prevalence was significantly (P<0.001) higher among the FSW-IDs (4.5%) than that among the FSW-NIDs (1.9%), suggestive of a stronger association between injecting drug use behaviour and HIV infection in the case of FSWs. It was observed that HIV prevalence was significantly higher among the FSW-IDs aged ≥35 yr, FSW who had sex work alone as the primary source of income or who were working in bars, beauty or massage parlours, FSW in sex work for more than a year and FSW practising sex work in urban areas. HIV prevalence was also found to be significantly higher among FSW-IDs who reported inconsistent condom usage with their sexual partners. Similarly, HIV prevalence was significantly higher among FSW-IDs who experienced physical violence and who consumed alcohol and oral drugs in comparison with FSW-NIDs. The results indicated that injecting drug use was significantly associated with high HIV prevalence among the FSWs (Figure).
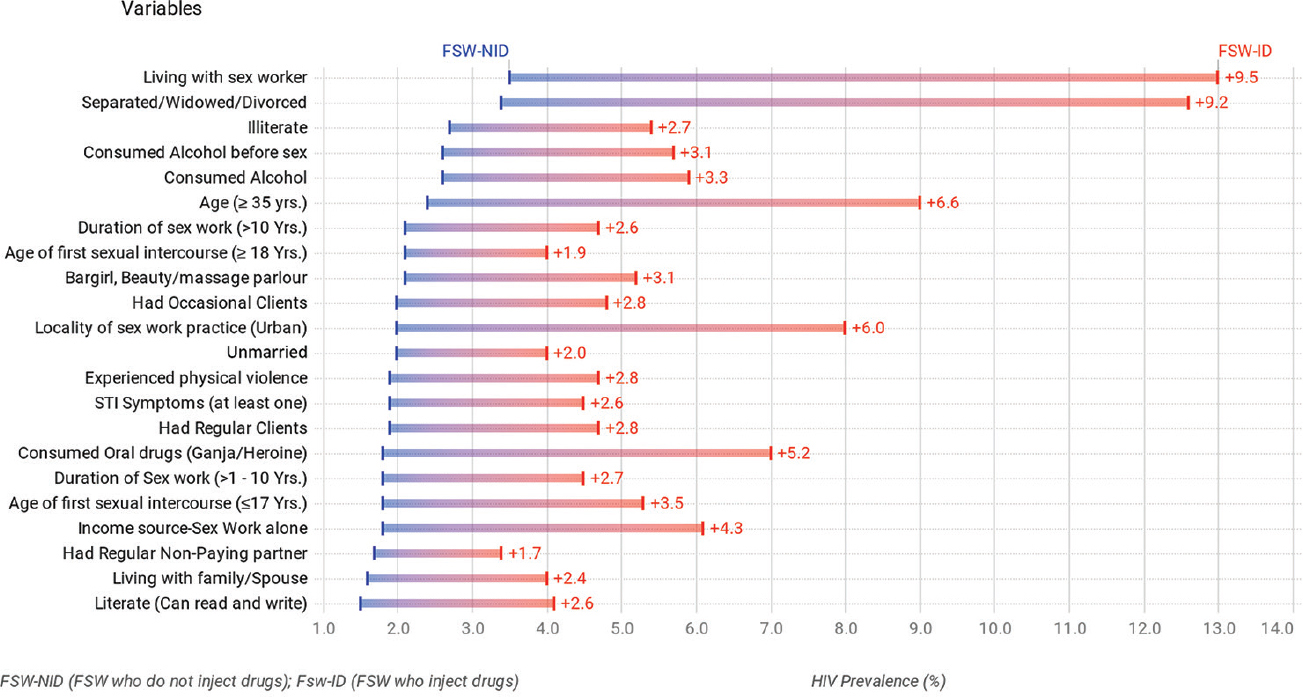
- HIV prevalence (%) and its difference among female sex workers who inject drug and female sex workers who do not inject drug: IBBS2014-2015.
The factors associated with a higher risk of HIV infection within the FSW-IDs analyzed using the logistic regression method using bivariate, and multivariable analyses are presented in Table II. Bivariate analysis showed that the independent variables significantly associated with a higher risk of HIV infection among the FSW-IDs were age, source of income, marital status, type of partners/members the FSW was living with, locality of sex work and consumption of alcohol and oral drugs. Multivariable analysis demonstrated that HIV prevalence was higher among FSW-IDs who were aged 35 and above [adjusted odds ratio (aOR): 6.22, confidence interval (CI): 2.06-18.78], those who relied upon sex work alone for a source of income (aOR: 2.71, CI: 0.92-7.94) and those who had dissolved marriage (aOR: 6.79, CI: 2.48 - 18.55) as compared to FSW-IDs who were younger than 24 yr, had sources of income other than sex work and who were married.
| Variables | HIV prevalence (%) | OR (95% CI) | aOR (95% CI) |
|---|---|---|---|
| Age group (yr) | |||
| ≤24 | 3.1 | 1 | 1 |
| 25-34 | 2.9 | 0.96 (0.36-2.60) | 1.15 (0.40-3.32) |
| ≥35 | 9.0 | 3.15 (1.22-8.11)* | 6.22 (2.06-18.78)*** |
| Education | |||
| Literate | 4.1 | 1 | |
| Illiterate | 5.4 | 1.34 (0.67-2.69) | |
| Source of income | |||
| Sex work alone | 6.1 | 3.43 (1.29-9.14)* | 2.71 (0.92-7.94)* |
| Bar girl, beauty/massage parlour | 5.2 | 2.87 (0.92-8.94) | 2.33 (0.68-7.99) |
| Other than sex work | 1.9 | 1 | 1 |
| Marital status | |||
| Married | 1.5 | 1 | 1 |
| Unmarried | 4.0 | 2.84 (1.00-8.08)* | 2.37 (0.69-8.13) |
| Separated/widowed/divorced | 12.6 | 9.71 (3.84-25.53)*** | 6.79 (2.48-18.55)*** |
| Currently living | |||
| Alone | 3.3 | 1 | |
| With family/spouse | 4.0 | 1.22 (0.41-3.59) | |
| With sex worker | 13 | 4.32 (1.21-15.45)* | |
| With another male partner | 0.0 | - | |
| With other female friends | 5.9 | 1.81 (0.32-10.35) | |
| With others | 0.0 | - | |
| Age of first sexual intercourse (yr) | |||
| ≤17 | 5.3 | 1.36 (0.70-2.66) | |
| ≥18 | 4.0 | 1 | |
| Duration of sex work (yr) | |||
| 0-1 | 3.7 | 1 | |
| >1-10 | 4.5 | 1.22 (0.27-5.35) | |
| >10 | 4.7 | 1.28 (0.28-5.82) | |
| Locality of place of sex work | |||
| Rural | 0 | - | |
| Urban | 8.0 | 8.17 (2.48-26.91)** | |
| Both | 1.0 | 1 | |
| Experienced physical violence | |||
| Yes | 4.7 | 1.08 (0.55-2.12) | |
| No | 4.3 | 1 | |
| Experienced sexual violence | |||
| Yes | 2.6 | 0.38 (0.18-0.78)* | 0.77 (0.33-1.82) |
| No | 6.6 | 1 | |
| Had occasional clients | |||
| Yes | 4.8 | 1.79 (0.54-5.94) | |
| No | 2.7 | 1 | |
| Had regular clients | |||
| Yes | 4.7 | 2.09 (0.49-8.87) | |
| No | 2.3 | 1 | |
| Had regular non-paying partner | |||
| Yes | 3.4 | 0.48 (0.24-0.93)* | 0.75 (0.33-1.69) |
| No | 6.9 | 1 | 1 |
| Had casual partner | |||
| Yes | 1.8 | 0.24 (0.10-0.55)** | 0.28 (0.10-0.75)* |
| No | 7.1 | 1 | 1 |
| Consumed alcohol (in the last 12 months) | |||
| Yes | 5.9 | 3.99 (1.40-11.41)* | 2.66 (0.83-8.58) |
| No | 1.5 | 1 | 1 |
| Consumed alcohol before sex | |||
| Yes | 5.7 | 0.87 (0.38-1.99) | |
| No | 6.5 | 1 | |
| Consumed oral drug (ganja/heroine) | |||
| Yes | 7 | 3.40 (1.58-7.33)** | 2.25 (0.93-5.44) |
| No | 2.2 | 1 | 1 |
| STI symptoms (at least one) | |||
| Yes | 4.5 | 0.99 (0.48-2.05) | |
| No | 4.5 | 1 | |
| Heard HIV/AIDS | |||
| Yes | 4.5 | 1 | |
| No | 3.9 | 0.86 (0.26-2.88) |
P*<0.05; **P<0.005; ***P<0.001. OR, odds ratio; CI, confidence interval; aOR, adjusted OR; STI, sexually transmitted infection
Discussion
FSWs have been reported to play a major role in HIV transmission to the general population through their clients (bridge population)2. The practice of female sex work is diverse and is traditionally followed among a few communities in various regions in India, such as north Karnataka and Rajasthan16. Various preventive interventions undertaken by the NACO and other organisations at the State and district levels have significantly contributed to the slowing down of HIV transmission. This is evident from the decline in adult HIV prevalence over the years in India1. The preventive measures among FSWs have predominantly focused on creating general awareness of HIV testing and management and encouraging condom usage. Studies show that FSWs, however, often indulge in injecting drug use due to the socio-environmental factors associated with their living or work conditions and peer practices, which increases the risk of HIV acquisition among the FSWs7. Various studies on FSWs conducted globally have indicated injecting drug use to be a significant risk factor for HIV infection7891011. While the IDU interventions in India predominantly focus on male IDUs, the FSW interventions have not adequately covered preventive measures for injecting practice-associated HIV acquisition risk. Identifying and addressing such lacunae in the current FSW interventions is essential for halting HIV transmission among FSWs.
The present study highlights the need for integrated interventions addressing risky behaviours associated with sexual as well as injecting drug use-related HIV transmission among FSWs. The prevalence of HIV among female IDUs and the factors associated with high HIV prevalence in FSWs were analyzed with dual risk behaviours in this study. The results suggest that prevention strategies for FSWs must include scrutiny to assess injecting drug practice and implementation of specially designed intervention programmes for older and unmarried FSWs who continue to practice sex work for day-to-day existence.
Theories such as life course and syndemic theory have been used to explain the higher risk of infection among HRG1718. Life course theory suggests that circumstances such as age at first commercial sex activity, duration of sexual activity, current age, education and violence victimization have an impact on condom usage and associated infection risks17. In our study, specific life course conditions such as age at first sex and duration of sex work were associated with higher HIV prevalence among FSW-IDs. A study conducted among FSWs in Kolkata, India, proposed an integrated theoretical model of life course vulnerabilities, economic insecurity, risk perceptions and empowerment attitudes that influence consistent condom usage among FSWs in India. It has been reported that Information Education Communication (IEC) activities for HIV prevention and increased condom usage were observed to be beneficial only among FSWs who were financially secure14; however, the majority of the vulnerable FSWs are financially dependent on sex work alone.
Older age is often associated with higher HIV infection risk among FSWs because of the higher chances of exposure risk as a result of the longer duration of their commercial sexual activity in most cases19. However, in the present study, it was observed that HIV prevalence was three times higher among older FSW-IDs than among older FSW-NIDs. The financial instability due to older age with potentially lesser clients20, reliance on sex work alone for their source of income or being divorced or being alone or widowed21 thus may impede their ability to negotiate condom usage with their clients. Such associated risks along with injection practices make older FSW-IDs more vulnerable to the risk of HIV acquisition.
The syndemic theory suggests that certain psychosocial behaviours and conditions such as depression, drug use and violence victimization are mutually reinforced, leading to a synergistic amplification effect on concentrated HIV prevalence among HRGs. A recent study of the syndemic model on MSM suggests that substance use and violence victimization interacted synergistically and had significantly higher odds of HIV transmission risk behaviour (inconsistent condom usage)17. In the present study, although FSW-IDs and FSW-NIDs did not differ by most of the demographic characteristics (age, education, source of income, marital status or locality), there was a significant difference in their sexual and social behaviours (Table I). For instance, the proportion of those who had casual clients was much higher among FSW-IDs than FSW-NIDs. The proportion exhibiting inconsistent condom usage among their clients was considerably higher among FSW-IDs. In addition, the proportion of those consuming alcohol, oral drugs or having at least one STI symptom was higher among the FSW-IDs (Table I). Apart from drug abuse, violence victimization and lack of social support have been reported to be associated with inconsistent condom usage, leading to higher HIV prevalence2223. The proportion of FSW-IDs who experienced either physical or sexual violence was much higher even in our study (Table I).
Notably, social behaviour can also be influenced by other factors such as environmental conditions. For instance, the HIV prevalence was significantly higher among FSW-IDs who were co-living with sex workers or spouse or family and those practicing sex work in urban areas than FSW-NIDs under similar living conditions (Table I). Co-living with other sex workers may increase the odds of unsafe injection practices through peer pressure. Similarly, spousal pressure or depression due to domestic violence can influence drug usage, which, inturn, may increase the infection risk as conceptualized by the chain of risk model10,17,24.
The needle syringe exchange programme (NSEP) is an IDU intervention that offers sterile injecting kits in exchange for used needles and syringes. However, IDUs sought non-NSEP sources to buy injection kits due to deficit supply at NSEP centres or environmental and social factors that hamper the utilization of NSEP. These centres are functional only in domains with high IDU population and FSW-IDs from other areas may not be aware of NSEP or might not have access to them2526. Owing to inaccessibility to sterile injections or financial constraints, FSWs often share needles or reuse the old needles/syringes. Some female IDUs have also been reported to be looking for used injections in hospital bins13. IDUs in the northeast reveal their HIV status and follow strategies such as serosorting and being the last receiver to prevent transmission risks to other FSWs who are HIV negative. A HIV-positive FSW is usually the last one to use the shared needle. Although effective to a certain extent, this puts HIV-infected FSW at risk of acquiring other infections such as HBV, HCV and other HIV infection due to other subtypes21. Studies reveal the origin of flash blood concept among FSWs in Tanzania, wherein a portion of the blood from an IDU who had just injected the drug is drawn and shared by the rest instead of the drug27. This is done to compensate for the unaffordability of the drugs; however, no studies are available to know the prevalence of such practices in India.
The results indicate a higher prevalence of HIV among FSW-IDs who were older, divorced, separated or widowed or were dependent on sex work for their source of income. Measures to incorporate integrated interventions with a special focus on facilitating awareness and improved access to NSEP and opioid substitution therapy (OST), encouraging safe sex and injecting practices, educating on the adverse effects of alcohol and drugs and securing the financial needs of the FSWs, are recommended for immediate consideration. Interventions for FSWs should attempt their rehabilitation by providing alternative means of survival, ensuring improved linkage to HIV prevention programmes and better adherence to anti-retroviral therapy to reduce the possibility of HIV transmission.
The National IBBS conducted in 2014-2015 is the latest, large-scale, bio-behavioural data on key populations, and its analysis can induce direct strategic planning for appropriate interventions for FSWs. It would, however, be critically important to generate the same periodically. Our study is, however, not without certain limitations. For lack of specific data and tools in the data management programme on the migration of FSWs and their potential duplication across the domains could not be studied. Data on ART knowledge, ART uptake and behavioural aspects/HIV status of the clients of FSWs were not analyzed as this information was not collected during the survey. Furthermore, no attempt was made to analyse the data to explore geo-cultural variations in HIV prevalence in the key sub-population of FSWs in this study.
Overall, awareness of injection risks and IEC activities on the adverse effects of injecting drugs and other sedative substances such as alcohol and oral drugs might result in behavioural changes among FSWs. Periodic HIV testing coupled with interventions for safe injection strategies are needed to achieve the sustainable development goal (SDG) ‘To End HIV by 2030’.
Acknowledgment
Authors acknowledge the project directors of all the State AIDS control societies, regional institutes, referral laboratories, State surveillance team members, and sentinel site personnel for their support in completing the surveillance activities on time.
Financial support & sponsorship: The National AIDS Control Organization (NACO) (Government of India) funded to conduct the National IBBS, NACO Grant No. T-11020/36/09-NACO (surveillance).
Conflicts of Interest: None.
References
- National AIDS Control Organization & ICMR-National Institute of Medical Statistics. In: India HIV Estimates 2019: Report. New Delhi: NACO, Ministry of Health and Family Welfare, Government of India; 2020.
- [Google Scholar]
- HIV/AIDS in India:An overview of the Indian epidemic. Oral Dis. 2016;22(Suppl 1):10-4.
- [Google Scholar]
- HIV Sentinel Surveillance: Technical Brief, India 2016-17. New Delhi: NACO, Ministry of Health and Family Welfare, Government of India; 2017.
- National AIDS Control Organization. Ministry of Health and Family Welfare, Government of India. In: Revamped and revised elements of targeted intervention for HIV prevention and care continuum among core population, strategy document 2019. New Delhi: NACO, MoHFW, GOI; 2019.
- [Google Scholar]
- HIV prevention &treatment strategies –Current challenges &future prospects. Indian J Med Res. 2018;148:671-4.
- [Google Scholar]
- Clusters of sexual behavior in human immunodeficiency virus-positive men who have sex with men reveal highly dissimilar time trends. Clin Infect Dis. 2020;70:416-24.
- [Google Scholar]
- Factors associated with history of drug use among Female Sex Workers (FSW) in a high HIV prevalence state of India. BMC Public Health. 2012;12:273.
- [Google Scholar]
- Mujer Mas Segura (Safer Women):A combination prevention intervention to reduce sexual and injection risks among female sex workers who inject drugs. BMC Public Health. 2012;12:653.
- [Google Scholar]
- Prevalence and correlates of female condom use and interest among injection drug-using female sex workers in two Mexico-US border cities. AIDS Behav. 2012;16:1877-86.
- [Google Scholar]
- Factors associated with pathways toward concurrent sex work and injection drug use among female sex workers who inject drugs in northern Mexico. Addiction. 2013;108:161-70.
- [Google Scholar]
- Determinants of HIV infection among female sex workers in two cities in the Republic of Moldova:The role of injection drug use and sexual risk. AIDS Behav. 2013;17:2588-96.
- [Google Scholar]
- The prevalence of HIV in female sex workers in Manipur, India. J Commun Dis. 1999;31:23-8.
- [Google Scholar]
- Spatial distribution and characteristics of Injecting Drug Users (IDU) in five Northeastern states of India. BMC Public Health. 2011;11:64.
- [Google Scholar]
- National Integrated Biological and Behavioural Surveillance (IBBS), India 2014-15. High Risk Groups. New Delhi: NACO, MoHFW, GOI; 2015.
- IBM SPSS Statistics for Windows, Version 26.0. Armonk, NY: IBM Corp; 2019.
- Sex Workers of India:Diversity in practice of prostitution and ways of life. New Delhi, India: Allied Publishers Private; 2006. p. :346.
- The syndemic of violence victimisation, drug use, frequent alcohol use, and HIV transmission risk behaviour among men who have sex with men:Cross-sectional, population-based study in India. SSM Popul Health. 2019;7:100348.
- [Google Scholar]
- Consistent condom use by female sex workers in Kolkata, India:Testing theories of economic insecurity, behavior change, life course vulnerability and empowerment. AIDS Behav. 2016;20:2332-45.
- [Google Scholar]
- Factors associated with HIV infection among female sex workers in Brazil. Medicine (Baltimore). 2018;97:S54-61.
- [Google Scholar]
- Are female sex workers able to negotiate condom use with male clients?The case of mobile FSWs in four high HIV prevalence states of India. PLoS One. 2013;8:e68043.
- [Google Scholar]
- Rates of HIV, syphilis, and HCV infections among different demographic groups of female sex workers in Guangxi China:Evidence from 2010 national sentinel surveillance data. AIDS Care. 2013;25:1433-41.
- [Google Scholar]
- Social environmental factors and condom use among female injection drug users who are sex workers in China. AIDS Behav. 2014;18(Suppl 2):S181-91.
- [Google Scholar]
- Measuring vulnerability among female sex workers in India using a multidimensional framework. PLoS One. 2018;13:e0204055.
- [Google Scholar]
- Inconsistent condom use among female sex workers:Partner-specific influences of substance use, violence, and condom coercion. AIDS Behav. 2020;24:762-74.
- [Google Scholar]
- Social-structural contexts of needle and syringe sharing behaviours of HIV-positive injecting drug users in Manipur, India:A mixed methods investigation. Harm Reduct J. 2011;8:9.
- [Google Scholar]
- Dual HIV risk and vulnerabilities among women who use or inject drugs:No single prevention strategy is the answer. Curr Opin HIV AIDS. 2012;7:326-31.
- [Google Scholar]
- Flashblood:Blood sharing among female injecting drug users in Tanzania. Addiction. 2010;105:1062-70.
- [Google Scholar]






