Translate this page into:
Increased risk of mortality among haemodialysis patients with or without prior stroke: A nationwide population-based study in Taiwan
Reprint requests: Dr Chiou-Chuen Wu, Chung Hwa College of Medical Technology, Two 187 lanes, No. 12 of right way in the Rende, District of Tainan, Taiwan e-mail: wuchiou@ms13.hinet.net Dr Kao-Chang Lin, Department of Neurology, Chi Mei Medical Center, No. 901, Jong-Hwa Rd, Yung Kung City, Tainan, Taiwan e-mail: gaujang@mail2000.com.tw
-
Received: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Patients with prior stroke (PS) undergoing chronic dialysis are at a high risk of mortality. However, little is known about the cumulative risk and survival rate of dialysis patients with long-term follow up. The aim of this study was to assess risks for mortality between patients with and without PS undergoing chronic haemodialysis (HD).
Methods:
The Taiwan National Health Insurance Research Database (NHRI-NHIRD-99182) was used and all adult patients (≥18 yr) with end stage renal disease (ESRD) who started maintenance HD between January 1, 1999, and December 31, 1999, were selected. The patients were followed from the first reported date of HD to the date of death, end of dialysis or December 31, 2008. A Cox's proportional hazard model was applied to identify the risk factors for all-cause mortality.
Results:
Among 5672 HD patients, 650 patients (11.5%) had PS. A higher proportion of stroke history at baseline was found in men (52.8%) and those aged ≥ 55 yr (80.9%). After adjusting for age, sex and other covariates, the patients with PS were found to have a 36 per cent increased risk of mortality compared to those without PS (HR 1.36, 95% CI: 1.22-1.52). The cumulative survival rates among HD patients without PS were 96.0 per cent at the first year, 68.4 per cent at the fifth year, and 46.7 per cent at the ninth year, and 92.9, 47.3 and 23.6 per cent, respectively, in those with PS (log-rank: P<0.001).
Interpretation & conclusions:
Our findings showed that PS was an important predictor for all-cause mortality and poor outcome in patients undergoing chronic HD.
Keywords
All-cause mortality
ESRD
haemodialysis
prior stroke
risk factors
Atherosclerosis is widely acknowledged to occur more frequently in patients with chronic kidney disease (CKD)1. Uremia per se is a cardiovascular risk factor independent of classic cardiovascular risk factors2. There is growing evidence of an association between CKD and adverse cardiovascular disease. Collins et al3 reported that patients with CKD were associated with a two-fold increase in cardiovascular disease as compared with general population. The prevalence of stroke was higher among incident cases of end-stage renal disease (ESRD) compared with the general population4, and 7-14 per cent of ESRD patients had a prior history of stroke (PS) at the time of initiation of dialysis56789.
These observations have an important public health and socio-economic impact. The prevalence of ESRD has increased markedly globally during the past few years, especially in Taiwan which has been ranked first in the world since 20021011. Atherosclerotic cardiovascular disease is a major cause of morbidity1 and mortality812 in patients with ESRD. Many studies have tried to identify the predictors for mortality in dialysis patients, with most focusing on risk factors, such as age, diabetic mellitus (DM), hypertension (HTN), heart failure (HF), coronary artery disease (CAD) and duration of follow up, etc6131415. However, studies on PS and mortality among patients with dialysis are lacking. Some studies have reported on ischaemic stroke and dialysis, however, the results have been inconsistent. Herzog et al12 reported that PS independently increased the risk of all-cause mortality in dialysis patients, while Lamping et al5 did not find any significant association with PS5.
We hypothesize that PS is an important predictor for mortality and poor outcome in haemodialysis (HD) patients. We used data from the Taiwan National Health Insurance Research Database (NHIRD)16 to investigate whether the PS was associated with an increased risk of all-cause mortality or poor long-term prognosis in patients with or without PS undergoing chronic haemodialysis.
Material & Methods
The National Health Insurance (NHI) programme, which provides compulsory universal health insurance, was implemented in Taiwan since 1995. With the exceptions of prison inmates, all citizens are enrolled in the programme. Patients with ESRD are eligible for any type of renal replacement therapy under the NHI programme without the need for extra payment16.
Patients in this study were drawn from NHIRD with trial registration number (NHRI-NHIRD-99182). In cooperation with NHI, a specific search was applied and all patients on dialysis with applying payment for dialysis from 1998 to 2008 in Taiwan were drawn. The NHIRD covers nearly all (>99%) inpatient and outpatient claims for approximately 23 million population of Taiwan. It is one of the largest and most comprehensive databases of its kind in the world, and had been used extensively in various studies1617. The NHIRD provides encrypted patient identification numbers, gender, date of birth, dates of admission and discharge, the medical institutions providing the services, the ICD-9-CM (International classification of diseases, ninth revision, Clinical modification)18 codes of diagnoses (up to five) and procedures (up to five), and outcomes. Information from the NHIRD was considered appropriately for the derivation of accurate estimation of chronic diseases as ESRD and co-morbidities. All NHIRD can be interlinked with each individual personal identification number.
Patient selection and definition: A longitudinal cohort study was designed in dialysis patients. Adult patients (age ≥18 yr) of ESRD on maintenance HD (who initiated HD treatment between January 1, 1999, and December 31, 1999) were selected. Several studies have been published in Taiwan using NHIRD for mortality1920212223. The Bureau of NHI issues major illness/injury certificate to patients who suffer from ESRD on maintenance dialysis. We linked the major illness/injury certificate file to get the date of death. The enrolled subjects were followed up from the first reported HD session to the date of death, end of dialysis or December 31, 2008. Patients who underwent peritoneal dialysis (PD) or switched type of dialysis were excluded based on the standard rules24. A total of 5672 incident HD patients were analyzed in this study.
Ascertainment of demographic and co-morbid variables: The diagnostic codes were linked through the outpatient and hospitalization claims databases of the NHI and were searched for the survival status, date of death, demographics and other relevant co-morbid variables. Co-morbidity was crucial for the survival rate and mortality, and all subjects were enrolled including those with PS, DM, HTN, HF, CAD, peripheral vascular disease (PVD), systemic lupus erythematous (SLE), liver cirrhosis (LC) and polycystic kidney disease (PCKD). The ICD-9-CM18 codes were used to define each co-morbidity: (i) DM (ICD-9-CM code 250.x x, 357.2, 362.0x, 366.41); (ii) HTN (362.11, 401.x -405.x, 437.2); (iii) HF (428.0-428.43, 428.9, 398.91); (iv) CAD (410.xx - 414.xx); (v) stroke (430-438.xx); (vi) PVD (440.x x-444.xx); (vii) LC (571.2, 571.5, 571.6, 456.20, 789.5); (viii) SLE (710); and (ix) PCKD (753.12-753.14).
Statistical analysis: All statistical analyses were performed with the Statistical Package for Social Sciences software package for Windows version 17.0 (SPSS Inc, USA). Baseline characteristics of with and without PS groups were compared using Pearson chi-square tests. Age was entered as a categorical variable (18-54 vs. ≥ 55 yr)25. The survival rate was estimated using the Kaplan-Meier method by PS and age-group (<55, ≥55 yr). The Cox's proportional hazard model was used to identify the risk factors for mortality with covariates such as age, sex, DM, HTN, PS, HF, CAD, PVD, SLE, LC and PCKD, and a multivariate regression model estimating all-cause mortality with hazard ratios (HRs) and 95% confidence intervals (CI) was derived. Interaction terms between PS and the two age groups were also tested. Further analyses included stratifying patients on the basis of age-group.
Results
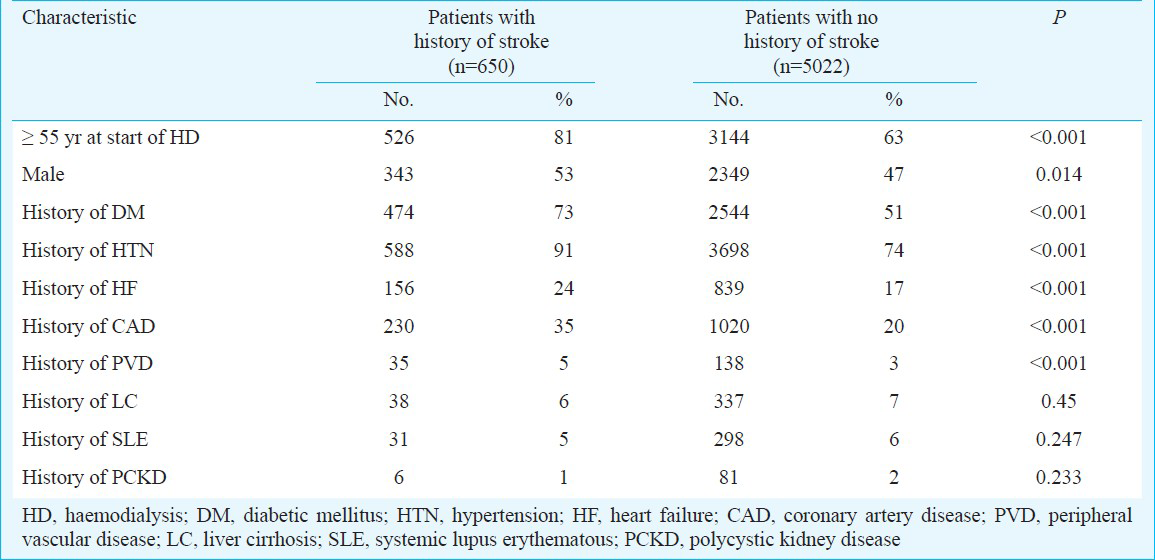
Table I shows the characteristics of the enrolled HD patients with and without PS. Among the eligible patients, 650 patients (11.5%) had PS compared to the majority of non-PS. There were substantial differences between between the two groups in numerous prognostic indicators of death, such as the proportion that were male (P<0.05), elderly (P<0.001), had a history of DM, HTN, HF, CAD, or PVD (P<0.001).
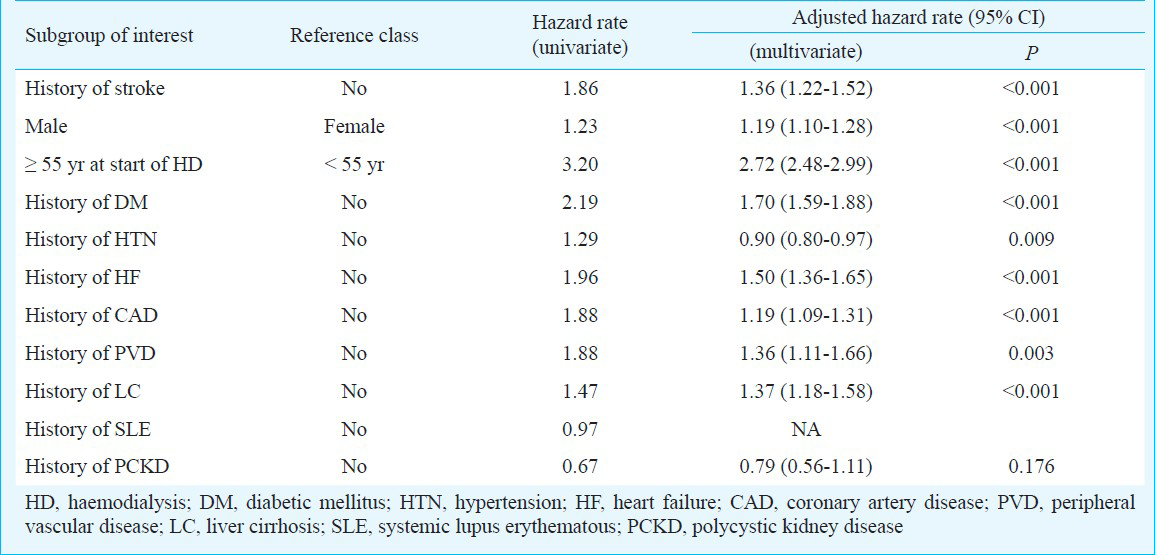
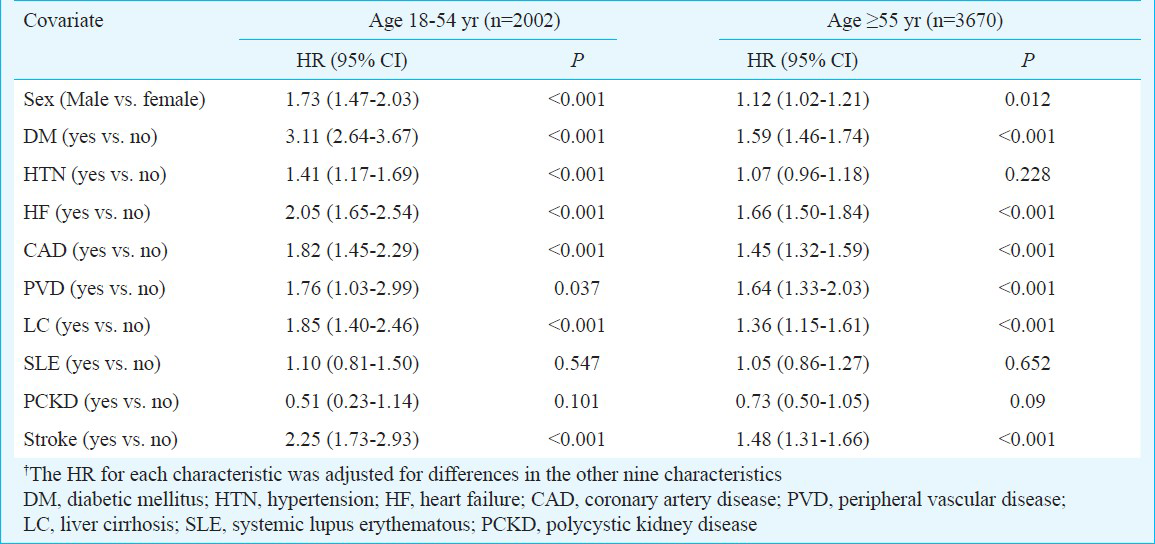
Risk factors for all-cause mortality in 1999 incident HD patients: The risks for all-cause mortality are listed in Table II. Using crude and multivariate analyses, sex, age, DM, HTN, HF, CAD, stroke, PVD, and LC were shown to have associations with mortality. The interaction between PS and different age groups was found to be statistically significant (P=0.005). Therefore, data were further analyzed stratified by different age groups (aged 18-54 and ≥55 yr). Table III shows the hazard ratios for all-cause mortality by age stratification (aged 18-54 and ≥55 yr). Male gender, DM, HF, CAD, PVD, LC and PS were associated with an increased risk of mortality. The patients with PS who were aged 18-54 yr had a 2.25-fold (HR 2.25, 95% CI: 1.73-2.93) increased risk of mortality, and those aged ≥55 had a 1.48-fold (HR 1.48, 95% CI: 1.31-1.66) increased risk of mortality compared to those without PS (P<0.001). After multivariate adjusted hazards ratios analyses, patients with PS were still at a higher risk of mortality than those without PS. The increased risk was 54 per cent (95% CI: 18%-102%) for patients aged 18-54 yr, and 34 per cent (95% CI: 18%-51%) in those aged ≥55 yr.
Cumulative survival rate: The cumulative survival rate in patients without PS was 96 per cent at the first year, 68 per cent at the fifth years and 47 per cent at the ninth years. These rates declined to 93, 47 and 24 per cent, respectively, in those with PS. Therefore, patients with PS had a shorter survival than those without PS, and this difference was significant from the first to ninth years (log-rank: P<0.001). The mean survival rate of the patients without PS was 85.0 months (95% CI: 83.8-86.2) compared to 65.6 months (95% CI: 62.3- 68.9) in those with PS (Fig. a), and the older patients had a worse survival rate. Further stratified by PS and different age groups, the younger patients (18-54 yr) without PS had the longest mean survival of up to 102.2 months (95% CI: 100.7-103.7), followed by the younger patients with PS of 85.8 months (95% CI: 78.8-92.9), the older (≥55 yr) patients without PS of 73.6 months (95% CI: 72.1-75.1), and the older patients with PS of 60.20 months (95% CI: 56.6-63.8), all of which were statistically significant (log-rank: P<0.001) (Fig. b).
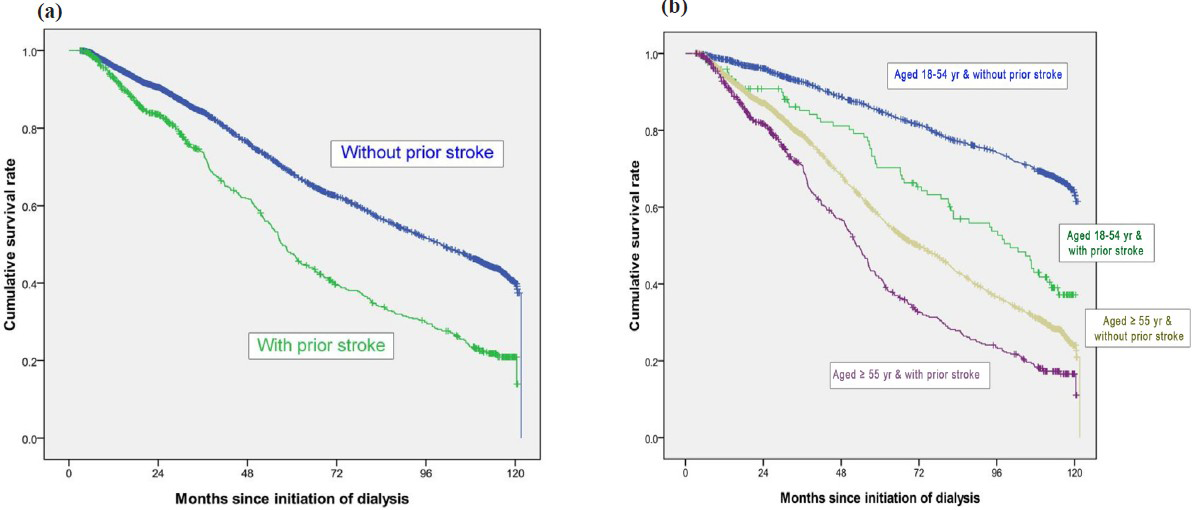
- Crude overall Kaplan-Meier survival curves for incident end-stage renal disease haemodialysis patients stratified by history of stroke (a) (log-rank: P<0.001) and different age groups, (b) (log-rank: P<0.001).
Discussion
We compared all-cause mortality between patients with and without PS among the registered HD population from the Taiwan NHIRD. After adjusting for age, gender and other covariates, PS was found to play an important role in mortality and poor outcome. The risk of mortality increased by 54 and 34 per cent in those aged 18-54 and ≥55 yr, respectively. No relevant data were found after a search of the literature, and we hypothesized that stroke type (e.g. intracranial haemorrhage or ischaemic stroke), or relative/absolute mortality to dialysis may be the cause.
The number of incident cases in our study was different from the report of Taiwan Society of Nephrology (TSN)11. The reasons were different definitions of ESRD on maintenance dialysis and inclusion criteria. In the report of TSN11, ESRD on maintenance dialysis was defined as received maintenance dialysis therapy for > 1 month. However, we used the definition of maintenance dialysis for more than 90 days. In addition, only adult patients (age ≥18 yr) on pure HD were included in our study. The TSN report included all incident cases, including HD, PD and switched type of dialysis.
In our study, 11.5 per cent of the ESRD patients had PS at the initiation of HD. The proportion of PS in dialysis population beyond the factor of age reflects the health status and the co-morbid conditions as cardiovascular disease. Inrig et al26 reported that only 2.6 per cent of dialysis patients with PS had a lower prevalence of co-morbid disease with a mean age at onset of ESRD of 47 years, and 35.5 per cent had DM co-morbidity. From the result of HEMO study27, 19.5 per cent of HD patients had a clinical diagnosis of PS at baseline, in which age, presence of any cardiac disease and DM were significantly associated. This finding is similar to our results. In our nation-wide database, 6.2 per cent of aged 18-54 and 14.3 per cent of aged 55 yr had PS, and had co-morbidity with DM (72.9%), HTN (90.5%), HF (24.0%), CAD (35.4%) and PVD (5.4%), which were all associated with cardiovascular disease. Taken together, it is reasonable to speculate that age and co-morbidity are relevant to mortality in dialysis patients with PS.
Many studies have demonstrated that stroke survivors have a higher mortality risk than individuals in the general population282930. However, little is known about the long-term prognosis among stroke survivors on dialysis. In the present study, the 1-year survival rates were 92.9 and 96.0 per cent in patients with and without PS, respectively, which were higher than the report of TSN (85.1%)11. This may be due to different inclusion criteria and definition for ESRD on maintenance dialysis. The 5-year survival rate among patients without PS was 68.4 per cent, which was higher than the report of TSN (53.7%)11. In contrast, the 5-year survival rate among patient with PS was 47.3 per cent, which was lower than the TSN report (53.7%)11. These findings suggested that the survival curve after PS had a deteriorated long-term prognosis than without PS. This time-dependent poor outcome is the result of CAD co-morbidity, systemic vascular disease as stroke or PVD, ageing factor, metabolic derangement, or secondary infection before and during dialysis31.
Our findings indicated that all patients with PS had an increased risk of mortality. Petty et al32 reported that CAD (particularly in younger patients) and HF were the most important predictors of mortality in patients with cerebral infarction. Taken together, we hypothesize that beyond age, vascular origin is the most important factor related to the risk of mortality in patients on dialysis. Further studies are warranted to investigate the predictors of mortality among stroke survivors.
There were several limitations to this study. First, the diagnosis of co-morbidities relied on the claim data and ICD-9-CM diagnosis codes, which might have resulted in potential disease misclassification33. Second, co-morbidities were assessed on the basis of a simple classification (present/ absent) that did not take into account the disease severity. Third, our study lacked data on duration and treatment regimens of diseases, biochemical data and socio-economic characteristics, which may have some influences in mortality. These should be considered as confounders or modifiers in future analysis. Finally, using the definition of ESRD on maintenance dialysis as starting dialysis for more than 90 days might be missing some early mortality within 90 days after initiation of dialysis.
In conclusion, based on nearly a 10-year period of longitudinal cohort analysis, our results showed that PS was an important predictor for all-cause mortality and poor long-term outcomes in patients on maintenance HD. Age was a decisive factor on outcomes, and the older patients had a higher cumulative mortality rate. Awareness of the relationship between stroke survivor and mortality is essential to dialysis patients especially in those with a prior history of stroke.
Acknowledgment
The study was performed in Chi-Mei Medical Center and supported by grant CMFHR10032 from hospital and grant NHRI-NHIRD-99182 from National Health Research Institutes in Taiwan. Authors thank all the staff in Professor Jhi-Joung Wang's Department of Medical Research, Chi-Mei Medical Center, Tainan, Taiwan.
References
- Chronic kidney disease as cause of cardio-vascular morbidity and mortality. Nephrol Dial Transplant. 2005;20:1048-56.
- [Google Scholar]
- Does renal failure cause an atherosclerotic milieu in patients with end-stage renal disease? Am J Med. 2001;110:198-204.
- [Google Scholar]
- Chronic kidney disease and cardiovascular disease in the Medicare population. Kidney Int. 2003;87(Suppl):S24-31.
- [Google Scholar]
- Elevated risk of stroke among patients with end-stage renal disease. Kidney Int. 2003;64:603-9.
- [Google Scholar]
- Clinical outcomes, quality of life, and costs in the North Thames Dialysis Study of elderly people on dialysis: a prospective cohort study. Lancet. 2000;356:1543-50.
- [Google Scholar]
- The differential impact of risk factors on mortality in hemodialysis and peritoneal dialysis. Kidney Int. 2004;66:2389-401.
- [Google Scholar]
- Propensity-matched mortality comparison of incident hemodialysis and peritoneal dialysis patients. J Am Soc Nephrol. 2010;21:499-506.
- [Google Scholar]
- Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med. 2004;351:1296-305.
- [Google Scholar]
- Traditional cardiovascular disease risk factors in dialysis patients compared with the general population: the CHOICE Study. J Am Soc Nephrol. 2002;13:1918-27.
- [Google Scholar]
- United States Renal Data System. Excerpts from the USRDS 2009 Annual Data Report: atlas of end-stage renal disease in the United States. Available from: http://www.usrds.org
- [Google Scholar]
- Taiwan Society of Nephrology. Incidence, prevalence and mortality trends of dialysis end-stage renal disease in Taiwan from 1990 to 2001: the impact of national health insurance. Nephrol Dial Transplant. 2008;23:3977-82.
- [Google Scholar]
- Poor long-term survival after acute myocardial infarction among patients on long-term dialysis. N Engl J Med. 1998;339:799-805.
- [Google Scholar]
- Survival comparison between hemodialysis and peritoneal dialysis based on matched doses of delivered therapy. J Am Soc Nephrol. 2002;13:S48-52.
- [Google Scholar]
- Comparing the risk for death with peritoneal dialysis and hemodialysis in a national cohort of patients with chronic kidney disease. Ann Intern Med. 2005;143:174-83.
- [Google Scholar]
- Comparative mortality of hemodialysis and peritoneal dialysis in Canada. Kidney Int. 2000;57:1720-6.
- [Google Scholar]
- Available from: www.doh.gov.tw/statistic/index.htm [in Chinese] http://www.doh.gov.tw/EN2006/index_EN.aspx [in English]
- Predictors of longterm mortality in patients with and without systemic lupus erythematosus on maintenance dialysis: a comparative study. J Rheumatol. 2011;38:2390-4.
- [Google Scholar]
- Chinese Hospital Association ICD-9 CM. Taipei, Taiwan: Chinese Hospital Association Press; 2000.
- [Google Scholar]
- Epidemiology and predictors of short-term mortality in symptomatic venous thromboembolism. Circ J. 2011;75:1998-2004.
- [Google Scholar]
- Survival rate in nasopharyngeal carcinoma improved by high caseload volume: a nationwide population-based study in Taiwan. Radiat Oncol. 2011;11:92.
- [Google Scholar]
- Lower mortality among stroke patients with schizophrenia: a nationwide population-based study. Psychosom Med. 2011;73:106-11.
- [Google Scholar]
- Do children of parents with mental illness have lower survival rate? A population-based study. Compr Psychiatry. 2010;51:250-5.
- [Google Scholar]
- Outcomes of prolonged mechanic ventilation: a discrimination model based on longitudinal health insurance and death certificate data. BMC Health Serv Res. 2012;12:100.
- [Google Scholar]
- United States Renal Data System: Treatment history (chapter V) Researcher's Guide to the USRDS Database 1999. Available from: http://www.usrds.org
- [Google Scholar]
- Survival analysis: comparing peritoneal dialysis and hemodialysis in Taiwan. Perit Dial Int. 2008;28(Suppl 3):S15-20.
- [Google Scholar]
- Mortality by dialysis modality among patients who have end-stage renal disease and are awaiting renal transplantation. Clin J Am Soc Nephrol. 2006;1:774-9.
- [Google Scholar]
- Cerebrovascular disease in maintenance hemodialysis patients: results of the HEMO Study. Am J Kidney Dis. 2006;47:131-8.
- [Google Scholar]
- Five-year survival after first-ever stroke and related prognostic factors in the Perth Community Stroke Study. Stroke. 2000;31:2080-6.
- [Google Scholar]
- Mortality and causes of death after first ischemic stroke: The Northern Manhattan Stroke Study. Neurology. 2001;57:2000-5.
- [Google Scholar]
- Long-term survival after first-ever stroke: The Oxfordshire Community Stroke Project. Stroke. 1993;24:796-800.
- [Google Scholar]
- Influence of co-morbidity on mortality and morbidity in patients treated with hemodialysis. Am J Kidney Dis. 1994;24:1010-8.
- [Google Scholar]
- Survival and recurrence after first cerebral infarction: a population-based study in Rochester, Minnesota, 1975 through 1989. Neurology. 1998;50:208-16.
- [Google Scholar]
- Risk of malignant neoplasms of liver and biliary tract in diabetic patients with different age and sex stratifications. Hepatology. 2010;52:155-63.
- [Google Scholar]






