Translate this page into:
Incidence & prognosis of acute kidney injury in individuals of snakebite in a tertiary care hospital in India
Reprint requests: Dr Ramulu Pulimaddi, Department of General Medicine, Osmania Medical College, Hyderabad 500 095, Telangana, India e-mail: ramulupulimaddi@gmail.com
-
Received: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
The snakebites are considered to be an occupational hazard in agriculture workers and the snake handlers, resulting in a considerable morbidity, mortality and economical implications. This study was conducted to determine the incidence, clinical presentation, renal injury and clinical outcome in snakebite victims who developed acute kidney injury (AKI).
Methods:
This hospital-based prospective, observational study was done on 100 cases who were admitted for the management of snakebite and found to develop AKI in a tertiary care hospital at Hyderabad, India. Renal function tests, complete blood picture, urine routine examination, ultrasound examination of abdomen and coagulation profile were done and the prognosis was assessed by noting recovery, mortality, morbidity and/or progress to chronic stage.
Results:
A total of 100 patients with a mean age of 43.80±12.63 yr (range 18-70); 62 males and 38 females were studied. All had bites on lower limbs. A total of 86 patients arrived in the hospital within 24 h, and 14 arrived after 24 h. Oliguria was found in 60, bleeding tendencies in 64, haemodynamic instability noted - tachycardia in 86. Systolic blood pressure (BP) was <120 mm Hg in 68 and BP was not recordable in four patients. Twelve patients were in stage III kidney disease and needed haemodialysis. Of the 100 cases of snakebite-induced acute kidney failure, 86 recovered and six died. On follow up, after six months eight patients developed chronic kidney failure.
Interpretation & conclusions:
A cascade of events tends to occur in severe haemotoxic envenomation such as bleeding disorders, hypotension/circulatory shock, intravascular haemolysis, disseminated intravascular coagulation and acute respiratory disease syndrome (ARDS). The findings of this study showed that early hospitalization, quick antisnake venom administration and adequate supporting care provided promising results.
Keywords
Acute kidney injury
antisnake venom
Russel's viper
snake bite
Incidence of snakebites is between 1.2 and 5.5 million worldwide each year, with 421,000-1,841,000 envenomations and 20,000-94,000 deaths1. In India, nearly 50 million people are at the risk of snakebite, which may occur any time in life with an estimated death of 50,000/yr2. Of the 216 species of snakes, 60 are considered poisonous in India3. The snakebite is considered to be an occupational hazard, especially for agriculture labourers/farm workers4 and snake handlers. The haemotoxic snakebites usually lead to the development of disseminated intravascular coagulation (DIC), renal failure, intravascular haemolysis and acute respiratory disease syndrome (ARDS)56. Acute renal damage is common cause of morbidity and mortality in most Indian patients with Russell's Viper bites7. Early administration of antisnake venom (ASV) along with appropriate supporting measures can minimize the fatality. The aim of this study was to observe the incidence and clinical profile of renal involvement in snakebite victims who developed acute kidney injury (AKI).
Material & Methods
A prospective hospital-based observational study was conducted with simple random sampling of 100 adult cases of AKI due to snakebite admitted in Medical Emergency department in Osmania General Hospital, a tertiary care hospital at Hyderabad, India, from November 2013 to July 2015. The snakebite victims who developed AKI after envenomation as proposed by AKI Network8 were considered for patients’ enrolment. Venous blood sample (5 ml) was collected in EDTA and Red Top/SST tubes (Becton Dickinson, NJ, USA) and serum was separated and stored at −20°C until further use. The study protocol was approved by the Ethics Committee of Osmania Medical College, Hyderabad, and written informed consent was obtained from patients/relatives.
Inclusion & exclusion criteria: AKI is defined as an abrupt (within 48 h) absolute increase in the serum creatinine concentration of ≥0.3 mg/dl from baseline, a percentage increase in the serum creatinine concentration ≥50 per cent or oliguria of 0.5 ml/kg body wt./h >six hours8. Those victims with pre-existing renal disease along with risk factors for developing renal disease with a history of snakebite (diabetes, hypertension, connective tissue disease and chronic infections) were excluded.
Laboratory investigations: All routine laboratory investigations were done based on standard clinical procedures and protocols, and patient-related clinical information was recorded on the proforma from the time of hospital admission till discharge or death. The laboratory investigations performed were blood urea, serum creatinine, creatine kinase by fully automated Erba Chem-7 Chemistry Analyzer (Transasia Bio-Medicals Ltd, Mumbai), complete urine examination by microscopy. Haematology parameters included complete blood counts (Mindray Hematology Analyzer BC 2800, Mindray Bio-Medical Electronics Co., Ltd., China); 20 min whole blood clotting time (WBCT); prothrombin time (PT); international normalized ratio (INR) (Coagulation Analyzer - STart Max - STAGO, UK); ultrasonography (USG) (Esaote portable ultrasound systems, Italy) abdomen by standard procedure. The renal functions were monitored on a daily basis, and the prognosis was assessed by noting recovery (improvement in renal parameters and urine output); mortality, morbidity and/or progress to chronic stage. All these patients were administered ASV as per the National Snakebite Protocol9 and patients were monitored for changes in requirement of ASV basing on their individual clinical profile in line with the WHO SEARO Guidelines10 for anti-haemostatic envenomation.
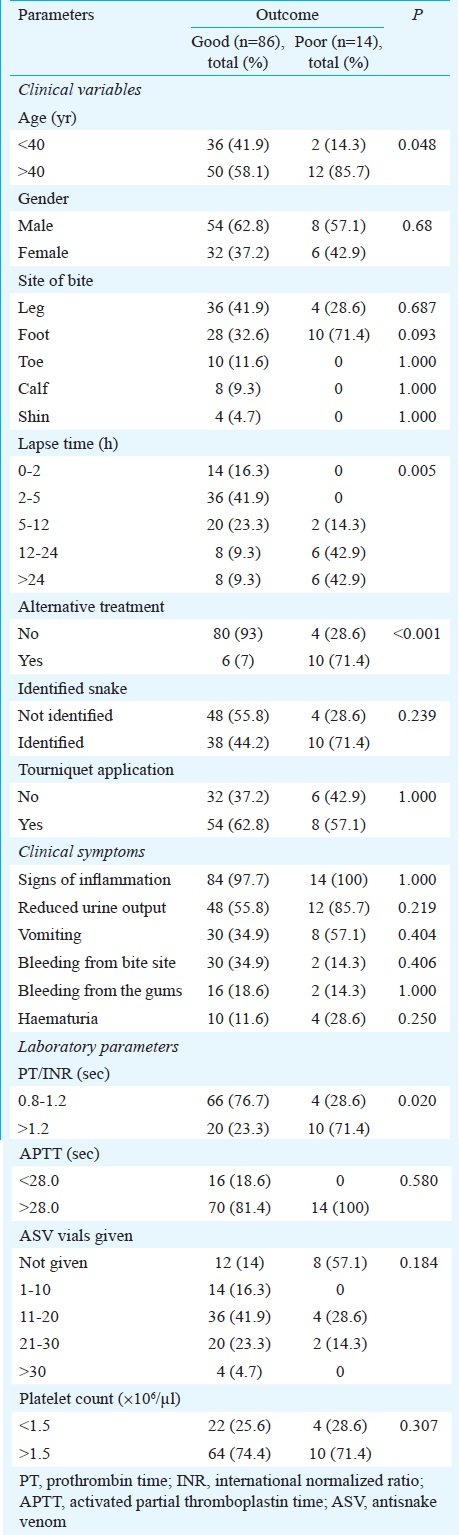
Statistical analysis: The patients were classified into two groups according to good outcome (recovered from AKI) and poor outcome (not recovered from AKI). The differences between the two groups were compared using the Chi-square test, the Fisher's exact probability test, or the Student's t test, wherever applicable.
Results
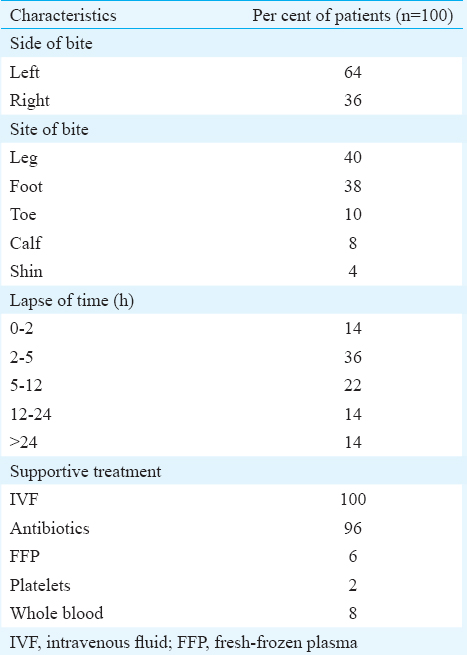
The age range of the patients (n=100, 62 male, 38 female) was from 18 to 70 yr with mean age of 43.80±12.63 yr (Table I). Thirty eight patients were in the age group of 18-40 yr, 58 in 41-60 yr and four were above 60 years. All patients had bites on lower limbs; of them 64 per cent had on the left side and 36 per cent on the right side (Table I). It was noted that the lapse of time in hours of patients’ arrival to hospital varied (Table I). Only 62 patients applied tourniquet at the area above the bite as a precautionary step to slow the spread of the venom before coming to the hospital. Forty eight patients had identified the snake in the event of the bite (viper 46 and cobra 2).
Clinical features noticed included reduced urine output in 60 associated with increased severity of AKI and need for haemodialysis in 12 patients and bleeding tendencies in 64 (site of the bite 32, gums 16, haematuria 14 and others 2). Tachycardia was seen in 86, systolic blood pressure (BP) was <120 mm Hg in 68, not recordable in four, diastolic BP was <80 mm Hg in 38 cases. USG abdomen was normal in 66 patients and was abnormal in 34 patients showing alteration in cortical echotexture with normal kidney size. Haematology data showed haemoglobin <10 g% in 54, total white cells <4000/μl in eight and >11,000/μl in 16 and platelets <1.5 ×106/μl in 26 patients. The whole blood clotted in <20 min in 70 patients, but prolonged bleeding time was found in only 16 patients. All patients had elevated blood urea and serum creatinine at the time of hospitalization. Mean blood urea levels at baseline 0, 24, 48 and 72 h were 61.01; 81.92; 74.26 and 64.83 mg/dl, respectively. Serum creatinine levels at the time of admission (0), 24, 48 and 72 h were 2.32 3.02; 2.94 and 2.52 mg/dl, respectively. All patients included in the study had elevated serum creatinine kinase levels with a mean of 266.58±122.53 U/l. PT-INR was prolonged (>1.2 sec) in 34 patients and activated partial thromboplastin time (APTT) was prolonged (>28 sec) in 88 patients. The mean 24 h urine output at 0, 24, 48 and 72 h was 1205.40; 1433.67; 1742.20 and 1981.00 ml, respectively with significant (P<0.001) variation.
Development of AKI Stages I, II and III were found in 84, 4 and 12 patients respectively. ASV administration criteria were as per the National Snakebite Protocol9. The requirement of ASV was 1-10 vials in 14 patients, 11-20 vials in 36 patients; 21-30 vials in 20 patients and >30 vials in four patients. All patients received intravenous fluid and other supportive treatment such as antibiotics, FFP, platelets and whole blood (Table I). Our study showed comparison between good outcome (recovered from AKI) and poor outcome (not recovered from AKI) of few parameters having significance (Table II). Of the 100 patients, 86 recovered; six patients died during hospital stay and eight developed chronic kidney disease (found after six months during follow up) and were referred to the department of Nephrology for further management.
Discussion
India has the highest mortality due to snakebites1 with an estimation of roughly 46,000 people dying every year11 and other study2 noted the magnitude of death even reaching to an estimated 50,000/yr. Venomous snake bites are classified as haemotoxic and neurotoxic. Hemotoxic venom induces several abnormalities leading to AKI and haematological disorder. It was observed that a cascade of events occurred in severe haemotoxic envenomation such as bleeding disorders, hypotension/circulatory shock, intravascular haemolysis, DIC and ARDS.
In our study, of the 100 patients, the snake was identified only in 48 cases (Viper 46 and Cobra 2) and the remaining cases were treated according to the clinical presentation. Majority of bites were of viper snake, which was supported by other studies1213. In this study, maximum number of victims (62 %) was males. Similar findings showing male preponderance were noted in many previous studies141516. However, some reports showed female predominance in their area17.
AKI was seen as an important consequence in Russell's viper bite and renal damage might have already occurred as most of our patients were referral cases previously managed in a resource-poor clinical setting such as primary and secondary health-care centres. Hence, our study was limited in ascertaining the incidence of renal failure in the population because of distance from the peripheral units to the tertiary care unit. The other major limitation was small sample size, non-identification of snake in some cases and lack of investigation performed like renal biopsy.
Early institution of ASV as mainstay therapy18 to the patients at the time of admission was beneficial in terms of their recovery, however, severe was the envenomation. Our study also showed comparison between good outcome (recovered from AKI) and poor outcome (not recovered from AKI) showing significance for ‘lapse of time in hours’ in presenting to the hospital after snake bite (P=0.005) and ‘alternative treatment taken’ before coming to the hospital (P<0.001).
In conclusion, our findings showed that early hospitalization, quick ASV administration and adequate supporting care gave promising results with recovery of 86 cases. However, if the patient developed grade III renal failure, the recovery was grim.
Conflicts of Interest: None.
References
- The global burden of snakebite: A literature analysis and modelling based on regional estimates of envenoming and deaths. PLoS Med. 2008;5:e218.
- [Google Scholar]
- Correlation between timing of ASV administration and complications in snake bites. J Assoc Physicians India. 2006;54:717-9.
- [Google Scholar]
- Acute kidney injury caused by bothrops snake venom. Nephron Clin Pract. 2011;119:c131-6.
- [Google Scholar]
- Vasculotoxic snake bite presenting with sepsis, acute renal failure, disseminated intravascular coagulation, and acute respiratory distress syndrome. Med J DY Patil Univ. 2013;6:197-9.
- [Google Scholar]
- Acute renal failure in snake envenomation: A large prospective study. Saudi J Kidney Dis Transpl. 2008;19:404-10.
- [Google Scholar]
- Acute Kidney Injury Network: Report of an initiative to improve outcomes in acute kidney injury. Crit Care. 2007;11:R31.
- [Google Scholar]
- National snakebite management protocol. New Delhi: Health & Family Welfare Department; 2007.
- [Google Scholar]
- Southeast Asian J Trop Med Public Health. 1999;30(Suppl 1):1-85.
- Snakebite mortality in India: a nationally representative mortality survey. PLoS Negl Trop Dis. 2011;5:e1018.
- [Google Scholar]
- Acute renal failure following snake bite (viper) J Assoc Physicians India. 1977;25:883-90.
- [Google Scholar]
- A study on the clinico-epidemiological profile and the outcome of snake bite victims in a tertiary care centre in Southern India. J Clin Diagn Res. 2013;7:122-6.
- [Google Scholar]
- A study of clinical profile of snake bite at a tertiary care centre. Toxicol Int. 2014;21:203-8.
- [Google Scholar]
- Epidemiology of cobra bite in Manipal, Southern India. J Indian Acad Forensic Med. 2010;32:224-7.
- [Google Scholar]
- Profile of snakebite envenoming in rural Maharashtra, India. J Assoc Physicians India. 2008;56:88-95.
- [Google Scholar]






