Translate this page into:
Importance of biomarkers in streptococcal acute tonsillitis & peritonsillar abscess
For correspondence: Dr Onur Unal, Department of Infectious Diseases and Clinical Microbiology, Suleyman Demirel University, 32260, Faculty of Medicine, Isparta, Turkey e-mail: onurunal@sdu.edu.tr
-
Received: ,
Abstract
Background & objectives
Acute tonsillitis is a disease that can often be cured with medical treatment. However, complications may occur during this disease process. One of these complications is peritonsillar abscess. In recent years, biomarkers have been frequently used in the diagnosis of diseases. The aim of the study was to reveal whether peritonsillar abscess develops after acute tonsillitis, and acute tonsillitis can be differentiated using biomarkers and which biomarker has higher predictive value for this differentiation.
Methods
The control group consisted of individuals who were operated for septoplasty in the otolaryngology clinic, and the acute tonsillitis group consisted of individuals diagnosed with acute tonsillitis in the same clinic. Both groups were statistically compared in terms of mean platelet volume (MPV), neutrophil to lymphocyte ratio (NLR), platelet to lymphocyte ratio (PLR), systemic immune inflammation index (SII), infection discrimination index (IDI), plateletcrit (PCT) and lymphocyte to monocyte ratio (LMR) biomarkers. Statistically, significant biomarker values were compared between the subgroups in the tonsillitis group of those who had only acute tonsillitis and those who had peritonsillar abscess due to acute tonsillitis. Receiver operating characteristics (ROC) curve analysis was performed on biomarkers for their ability to predict the presence of peritonsillar abscess.
Results
When the individuals who had only acute tonsillitis and those who had acute tonsillitis with peritonsillar abscess were compared in terms of biomarkers, there was a statistically significant difference between the mean MPV, SII and PCT (P=0.010, 0.021, 0.023, respectively). ROC analysis was performed to calculate the sensitivity and specificity of MPV, PCT and SII for the diagnosis of acute tonsillitis with peritonsillar abscess (sensitivity-specificity for MPV 51.9–72.7%, for SII 94.2–32.7%, for PCT 71.2–50.9%, respectively).
Interpretation & conclusions
MPV, SII and PCT biomarkers may be useful to help clinicians predict peritonsillar abscess due to acute tonsillitis.
Keywords
Acute tonsillitis
biomarkers
mean platelet volume
peritonsillar abscess
plateletcrit
systemic immune-inflammation index
Tonsillitis is a term used for acute inflammation of the palatine tonsil tissue. Although it is most often seen in school-age children, it can also be seen in adults. When complications occur due to this disease, significant loss of working days occurs1. One of the local complications of acute tonsillitis is peritonsillar abscess. Peritonsillar abscess is characterized by pus accumulation in the peritonsillar area following acute tonsillitis, and treatment includes surgical abscess drainage with antibiotic therapy. Early diagnosis and treatment of peritonsillar abscess is essential because it is a disease that can lead to mortality2, 4. Often, swelling in the upper palatine tonsils and pushing of the uvula across the swelling side suggest peritonsillar abscess, but these findings are unclear in some patients. Contrast-enhanced computed tomography can distinguish peritonsillar abscess from acute tonsillitis, but more easily accessible techniques are needed to diagnose peritonsillar abscess, since this imaging method is only available in tertiary hospitals, radiation is dispersed during the examination, and the examination is costly5.
In recent years, examination of the relationships between many biomarkers calculated from complete blood count (CBC) and infectious diseases has gained acceleration. These biomarkers have become popular due to the fact that they can be calculated on the basis of CBC and have low cost. Some of these biomarkers include mean platelet volume (MPV), neutrophil to lymphocyte ratio (NLR), platelet to lymphocyte ratio (PLR), systemic immune inflammation index (SII), infection discrimination index (IDI), plateletcrit (PCT), and lymphocyte to monocyte ratio (LMR)6, 12.
As per author knowledge, no literature exists on simultaneous evaluation of the efficacy of many biomarkers to reveal the presence of peritonsillar abscess after acute tonsillitis. This study aimed to evaluate the biomarkers for their ability to suggest, with high predictive value, the presence of peritonsillar abscess in patients with acute tonsillitis.
Material & Methods
This study was conducted in the departments of Infectious Diseases and Clinical Microbiology, and Otorhinolaryngology clinics after obtaining study protocol approval from the Institutional Ethics Committee. Due to the retrospective nature of the study, informed consent forms could not be obtained from the participants. The study was designed as a retrospective review of hospital records between January 2010 and January 2021.
The study included two groups (control and acute tonsillitis groups). The control group consisted of individuals who had undergone septoplasty in the otorhinolaryngology department and the acute tonsillitis group consisted of acute tonsillitis individuals who were admitted to the departments of Infectious Diseases and Clinical Microbiology, and Otorhinolaryngology. In order to make a more detailed statistical analysis of the acute tonsillitis group, it was divided into two subgroups as ‘acute tonsillitis with peritonsillar abscess’ and ‘only acute tonsillitis’. The blood samples for the control group were taken before septoplasty, while the samples for the acute tonsillitis group were taken when the patients were admitted.
The common inclusion criteria for both groups were determined as follows: (i) being 18 yr or older; (ii) having a CBC test taken between 08:00 and 10:00 in the morning following at least eight hours of fasting; (iii) absence of comorbid conditions (hypertension, diabetes mellitus, chronic kidney failure etc.); and (iv) absence of continuous medication.
In order to be included in the acute tonsillitis group, the following additional criteria were determined: (i) applying hospital within five days at the latest from the onset of symptoms; (ii) not having received antibiotics and/or other treatments before attendance; (iii) growth of group A beta-haemolytic streptococcus in throat culture for patients with acute tonsillitis without peritonsillar abscess; and (iv) diagnosis being confirmed by contrast-enhanced computed tomography of the neck and surgical drainage of the abscess for patients who had acute tonsillitis with peritonsillar abscess.
Venous blood samples were placed in tubes containing ethylenediaminetetraacetic acid (EDTA) for the measurement of CBC for individuals included in the study. CBC of the samples was performed using the Beckman Coulter UniCelDxH 800 haematology analyser (Beckman Coulter, Brea, USA). The manufacturer’s instructions for the device were followed for all analyses. Then, MPV, NLR, PLR, SII, IDI, PCT and LMR were calculated from CBC data (Supplementary Table I).
Statistical analysis
Data analysis was performed using SPSS 24.0 (SPSS Inc, Chicago, IL). In the descriptive findings, categorical variables are presented as percentage and continuous variables are presented as mean ± standard deviation. The chi-squared test was used to determine the differences between categorical variables. The Kolmogorov-Smirnov test was used to verify the normal distribution of continuous variables between the groups. Independent samples t test was used for those with normal distribution and the Mann-Whitney U test was used for those with non-normal distribution. Statistical significance was considered at P<0.05. The ability of MPV, SII and PCT values to predict the presence of acute tonsillitis with peritonsillar abscess was analysed using receiver operating characteristics (ROC) curve analysis. The Youden index was used to calculate the cut-off value. If a significant cut-off value was observed, the sensitivity and specificity values were presented. According to the F test results performed in the G*Power (software ver. 3.1.9.2, https://www.psychologie.hhu.de/arbeitsgruppen/allgemeine-psychologie-und-arbeitspsychologie/gpower), the power (1-β error probability) was calculated as 0.842 (α error probability: 0.05, medium effect size: 0.25).
Results
There were 67 study participants in the control group in the study, 27 (40.3%) females and 40 (59.7%) males. In the acute tonsillitis group, there were 107 study participants, 41 (38.3%) females and 66 (61.7%) males. While the mean age of the control group was 38.59±7.13 yr, it was 36.21±12.31 yr in the acute tonsillitis group. When the groups were compared in terms of gender and age, there was no statistically significant difference (P=0.794, P=0.108, respectively). The values obtained from the CBC of the control and acute tonsillitis groups are presented in Table I.
| Parameter |
Control, (n=67) Mean±SD (Median) |
Acute Tonsillitis, (n=107) Mean±SD (Median) |
P value |
|---|---|---|---|
| WBC (103/μl) | 6.72±1.23 (6.5) | 12.77±4.85 (12.4) | <0.001a |
| Neutrophil (103/μl) | 3.82±1.01 (3.7) | 9.76±4.68 (9.2) | <0.001b |
| Lymphocyte(103/μl) | 2.02±0.54 (2) | 1.92±1.07 (1.9) | 0.061a |
| Monocyte (103/μl) | 0.51±0.13 (0.5) | 0.97±0.48 (0.9) | <0.001a |
| Hgb (g/dl) | 15.04±1.04 (14.8) | 14.12±1.36 (14.2) | <0.001b |
| Plt (103/μl) | 228.95±44.66 (228) | 261.49±67.61 (250) | 0.002a |
| MPV (fl) | 8.74±0.86 (8.7) | 8.39±0.91 (8.4) | 0.012b |
| NLR | 2.07±1.05 (1.8) | 6.82±6.11 (5.21) | <0.001a |
| PLR | 123.57±55.45 (114.44) | 170.99±105.62 (150) | <0.001a |
| SII | 469.82±221.75 (439.6) | 1806.65±1959.03 (1388.4) | <0.001a |
| IDI | 1.56±0.5 (1.48) | 4.11±3.82 (3.26) | <0.001a |
| PCT | 0.1987±0.0357 (0.201) | 0.2167±0.0505 (0.207) | 0.042a |
| LMR | 4.17±1.44 (4) | 2.3±1.26 (1.9) | <0.001a |
Statistical significance at P<0.001. aMann-Whitney U and bIndependent samples t test. CBC, complete blood count; WBC, white blood cell count; Hgb, haemoglobin; Plt, platelet count; MPV, mean platelet volume; NLR, neutrophil to lymphocyte ratio; PLR, platelet to lymphocyte ratio; SII, systemic immune inflammatory index; IDI, infection discrimination index; PCT, plateletcrit; LMR, lymphocyte to monocyte ratio; SD, standard deviation
The values calculated from the CBC of the subgroups in the acute tonsillitis group (only tonsillitis and tonsillitis with peritonsillar abscess) are presented in Table II.
| Parameter |
Acute tonsillitis (n=55) Mean±SD (Median) |
Acute tonsillitis with peritonsillar abscess (n=52) Mean±SD (Median) |
P value |
|---|---|---|---|
| WBC (103/μl) | 11.52±5.13 (10.1) | 14.09±4.19 (13.1) | 0.001a |
| Neutrophil (103/μl) | 8.59±4.94 (7.5) | 11.00±4.09 (10.45) | 0.001a |
| Lymphocyte (103/μl) | 1.92±1.06 (1.7) | 1.93±1.08 (1.9) | 0.784a |
| Monocyte (103/μl) | 0.86±0.44 (0.7) | 1.09±0.5 (1.1) | 0.004a |
| Hgb (g/dl) | 14.05±1.39 (14.1) | 14.19±1.34 (14.25) | 0.531b |
| Plt (103/μl) | 242.61±66.04 (239) | 281.46±63.96 (272) | 0.002b |
| MPV (fl) | 8.60±0.9 (8.5) | 8.16±0.88 (8) | 0.01b |
| NLR (%) | 6.17±4.98 (4.35) | 7.50±7.1 (5.58) | 0.134a |
| PLR (%) | 158.62±79.15 (144.28) | 184.08±127.33 (150.58) | 0.456a |
| SII (%) | 1430.39±1107.29 (1147.25) | 2204.61±2522.75 (1584.46) | 0.021a |
| IDI (%) | 3.63±2.25 (2.96) | 4.62±4.95 (3.44) | 0.19a |
| PCT (%) | 0.2057±0.0478 (0.19) | 0.2284±0.0511 (0.22) | 0.023b |
| LMR (%) | 2.54±1.38 (2) | 2.04±1.08 (1.82) | 0.085a |
Statistical significance at P<0.05. aMann-Whitney U and bIndependent samples t test
ROC analysis showed that MPV, SII and PCT had diagnostic value for predicting acute tonsillitis with peritonsillar abscess (AUC: 0.644, 95% CI: 0.54–0.749, P=0.01; AUC: 0.63, 95% CI: 0.524–0.735, P=0.021; AUC: 0.627, 95% CI: 0.522–0.733, P=0.023, respectively). On the basis of the analysis, the optimum cut-off values were determined as 8.05 for MPV, 686.88 for SII and 0.1975 for PCT. With these cut-off values, the sensitivity and specificity of MPV, SII and PCT were 51.9–72.7, 94.2–32.7 and 71.2–50.9 per cent, respectively, for predicting acute tonsillitis with peritonsillar abscess (Table III, Fig. 1 and 2; and Supplementary Table II-IV).
| Biomarker/Cut-off | Acute tonsillitis, n(%) | Acute tonsillitis with peritonsillar abscess, n(%) | Sensitivity (%) | Specificity (%) |
|---|---|---|---|---|
| MPV | ||||
| <8.05 | 15(27.3) | 27(51.9) | 51.9 | 72.7 |
| ≥8.05 | 40(72.7) | 25(48.1) | ||
| SII | ||||
| <686.88 | 18(32.7) | 3(5.8) | 94.2 | 32.7 |
| ≥686.88 | 37(67.3) | 49(94.2) | ||
| PCT | ||||
| <0.1975 | 28(50.9) | 15(30.8) | 71.2 | 50.9 |
| ≥0.1975 | 27(49.1) | 37(71.2) |
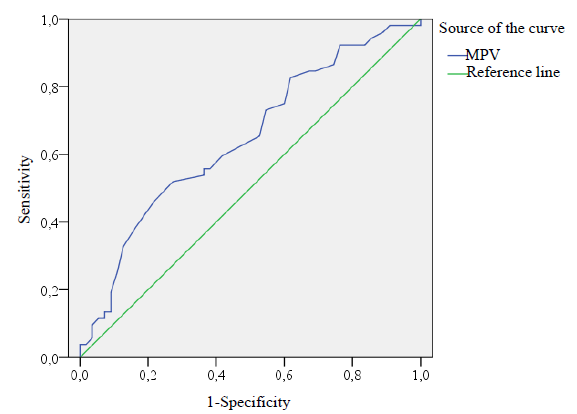
- ROC curve analysis for MPV in the acute tonsillitis with peritonsillar abscess group (cut-off values 8.05). ROC, receiver operating characteristics; MPV, mean platelet value.

- ROC curve analysis for SII and PCT values in the acute tonsillitis with peritonsillar abscess group (cut-off values 686.88 and 0.1975, respectively). SII, systemic immune inflammation index; PCT, plateletcrit.
Discussion
CBC is performed during the treatment of many infectious diseases. CBC can be performed in most centres and is relatively inexpensive. For this reason, biomarkers calculated with the parameters in CBC are also easily obtained. The use of these biomarkers has gained popularity in recent years. These biomarkers have also been investigated for the diagnosis and prognosis of diseases6, 12. In this study, examining the ability of biomarkers to predict the development of peritonsillar abscesses in patients with tonsillitis, important findings were obtained for MPV, SII and PCT.
MPV is a parameter that shows variances in platelet volume and is calculated directly from CBC6. It was stated that in the early stages of infection, there may be an increase in the MPV due to platelet activation11,13,14. In the inflammatory process, a decrease in MPV can be observed due to the use of active or large platelets and/or defective thrombopoiesis13. While an increase in MPV was reported in various inflammatory diseases (sepsis, infective endocarditis), it was reported that there was a decrease in some conditions (gastroenteritis, acute appendicitis, acute pancreatitis)15, 20. MPV has been evaluated in studies involving patients with peritonsillar abscess; has been documented to MPV increase in patients with abscess in one of the studies and decreased in the other in accordance with our findings2,3. Even though it is not clear why patients with tonsillitis and peritonsillar abscess have lower MPV, depletion of active or large platelets and/or defective thrombopoiesis during severe inflammation could be the most likely causes2. In addition, in the study by Albayrak et al18, MPV values were lower in patients with acute appendicitis attending clinics with considerable time/gap following appearance of symptoms. Peritonsillar abscess development occurs in the late stage of tonsillitis. In this study, individuals with peritonsillar abscess had lower MPV values than healthy individuals and study participants with acute tonsillitis only. Comparing the literature on the topic with our study findings, it seems that the prolongation in the duration of inflammation causes a decrease in the MPV value in the CBC18. Noticeably, SII, a recently developed biomarker is currently being used in the prognostic evaluation of various diseases, especially in cancer patients9,11. There are a limited number of publications evaluating the relationship between bacterial infections and SII, a few of the researchers have emphasized that SII may be useful in predicting mortality in community-acquired pneumonia11. Another study used SII to determine the severity of odontogenic infections21.The findings of our study support the SII index as a helpful parameter, both in the diagnosis of acute tonsillitis and in predicting the presence of peritonsillar abscess. This is attributed to the significant increase in neutrophil and platelet counts two parameters included in the SII formula during these infections. Of course, as the severity of an event increases, that is, if there is peritonsillar abscess development along with acute tonsillitis, the SII value increases even more.
PCT, which shows the proportion of blood volume occupied by platelets, is thought to be a potential marker of inflammation22. In addition to viral diseases such as hepatitis A and COVID-19, there are studies investigating the contribution of PCT to prognosis in bacterial diseases such as tuberculosis22,23. In a study in COVID-19 patients, low PCT values were associated with severe disease14. Contrarily in another study, PCT was detected as a positive acute phase reactant in patients with hepatitis A infection22. Similarly, in the study by Stefanescu et al23 in tuberculosis patients, high PCT values were associated with active tuberculosis disease, and they found that the PCT value decreased in patients with negative culture results after treatment23. The contribution of PCT in demonstrating the development of peritonsillar abscess was evaluated for the first time in our study. This index acted as a positive acute phase reactant, and it appeared that PCT might be of help both in the diagnosis of acute tonsillitis and in predicting the development of peritonsillar abscess.
Although there are studies evaluating the clinical significance and diagnostic benefit of LMR in the COVID-19 patients, the number of studies evaluating its contribution to the course of bacterial infections is limited14. In studies evaluating patients with liver cirrhosis, low LMR value contributed to the prediction of bacterial infection and mortality in those with septic shock12,24. As the severity of bacterial infections increases, lymphocytes remain indifferent to the increasing trend of monocytes and the LMR value decreases. Our study supports the view that low LMR value can indicate inflammation in the tonsillar tissue, but it is insufficient to predict the development of peritonsillar abscess after acute tonsillitis.
IDI is a new index defined by Kumbul et al10 calculated according to the following formula:
This index is helpful in discriminating acute tonsillitis that may develop due to group A β-haemolytic streptococcus or Epstein-Barr virus. The criteria for inclusion in the tonsillitis group in this study were group A β-haemolytic streptococcus growth in throat culture and development of peritonsillar abscesses. It is known that the development of peritonsillar abscesses is mostly due to bacterial agents10. Therefore, the IDI value in the tonsillitis group (acute tonsillitis and acute tonsillitis with peritonsillar abscess) was higher than the control group in this study due to the increased neutrophil count during bacterial infections (P<0.001). Unfortunately, this statistically significance did not contribute significantly to the clinical prediction for the development of peritonsillar abscess. This could be attributed to the parallel increases in neutrophil and monocytes in both acute tonsillitis and peritonsillar abscess.
NLR has a similar formula to IDI, except that it does not evaluate the monocyte count. Baglam et al7 reported that the NLR value in patients with acute bacterial tonsillitis with deep neck infection was higher than that in patients with acute bacterial tonsillitis without deep neck infection, and it may be helpful in the early diagnosis of deep neck infection complications7. In our study, the NLR value was higher in the tonsillitis group than in the control group due to the increase in the neutrophil count in the bacterial infection process, but no statistical difference was observed between the mean NLR values in the acute tonsillitis and peritonsillar abscess groups. In particular, two points differed when our study was compared with the study by Baglam et al7: firstly, in our study, NLR comparison was made only in study participants with peritonsillar abscesses. However, Baglam et al7 evaluated NLR in deep neck infections. Therefore, they included a more heterogeneous group than our patient population. Secondly, in our study, the number of patients who had peritonsillar abscesses was higher than in the study mentioned above, which could contribute to the difference in results due to sampling variation.
PLR elevation is linked to reactive thrombocytosis and/or lymphopenia. Depending on elevated cytokines during infectious disorders, mega-karyopoiesis may be stimulated and an increase in platelet count can be observed8. In our study, the PLR value in the group with acute tonsillitis was found to be higher than that in the control group. Noticeably, although the PLR value in study participants with acute tonsillitis and peritonsillar abscess was higher than that of individuals with acute tonsillitis only, it was not found to be sufficient to differentiate the diseases.
As per author knowledge, our study is the first to examine various biomarkers in a single study in order to discriminate between acute tonsillitis and tonsillitis with peritonsillar abscess. Despite this strength, there are some limitations. First, our study is a retrospective clinical study. Second, only patients with group A β-haemolytic streptococcus were included in the acute tonsillitis group without peritonsillar abscess in our study. Although this bacterium is one of the microorganisms causing frequent infections in tonsil tissue, it cannot be expected to represent all microorganisms. Third, in our study no comparison was made with individuals having diseases such as pharyngitis, laryngopharyngeal reflux and more, which are included in the differential diagnosis of acute tonsillitis. Fourth, unfortunately the blood tests of each patient during the follow-up period in the study were performed at different periods. There were also differences in the treatment regimens prescribed. It was predicted that the additional inflammation caused by the drainage process could also affect these parameters. For these reasons, values during the follow-up period were not included in the study.
In conclusion, MPV, SII and PCT values may help predict the development of peritonsillar abscesses. However, they should not be interpreted directly in favour of peritonsillar abscess. Because changes in these markers can also be seen in severe infections and other abscesses occurring in the neck cavities, we think they can help the clinician decide on radiological examination in the presence of suspicion of peritonsillar abscess.
Financial support & sponsorship
None.
Conflicts of Interest
This study was presented as an oral presentation at the 5th International Health Science and Life Congress held in Burdur, Turkey on March 10-12, 2022 (https://drive.google.com/file/d/1_sRxVBZvQLO-vDz8vb0jVCgrEXNdHxUE/view?pli=1).
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of AI-assisted technology for assisting in the writing of the manuscript and no images were manipulated using AI.
References
- Clinical practice guideline: Tonsillitis I. Diagnostics and nonsurgical management. Eur Arch Otorhinolaryngol. 2016;273:973-87.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Diagnostic role of mean platelet volume in tonsillitis with and without peritonsillar abscess. J Laryngol Otol. 2018;132:615-8.
- [CrossRef] [PubMed] [Google Scholar]
- The role of the mean platelet volume and neutrophil-to-lymphocyte ratio in peritonsillar abscesses. Braz J Otorhinolaryngol. 2016;82:662-7.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Epidemiological and microbiological aspects of the peritonsillar abscess. Int J Environ Res Public Health. 2020;17:1.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Computed tomography use patterns for pediatric patients with peritonsillar abscess. Int J Pediatr Otorhinolaryngol. 2019;123:22-5.
- [CrossRef] [PubMed] [Google Scholar]
- Are mean platelet volume and platelet distribution width useful parameters in children with acute rheumatic carditis? Pediatr Cardiol. 2014;35:53-6.
- [CrossRef] [PubMed] [Google Scholar]
- Predictive value of the neutrophil-to-lymphocyte ratio in patients with deep neck space infection secondary to acute bacterial tonsillitis. Int J Pediatr Otorhinolaryngol. 2015;79:1421-4.
- [CrossRef] [PubMed] [Google Scholar]
- Primary and secondary thrombocytosis in childhood. Br J Haematol. 2005;129:165-77.
- [CrossRef] [PubMed] [Google Scholar]
- Systemic immune-inflammation index predicts prognosis of patients after curative resection for hepatocellular carcinoma. Clin Cancer Res. 2014;20:6212-22.
- [CrossRef] [PubMed] [Google Scholar]
- New index for the discrimination of acute streptococcal tonsillopharyngitis and infectious mononucleosis: Infection discrimination index. Eur J Rhinol Allergy. 2020;3:64-8.
- [Google Scholar]
- Comparison of inflammation markers with prediction scores in patients with community-acquired pneumonia. Bratisl LekListy. 2021;122:418-23.
- [CrossRef] [PubMed] [Google Scholar]
- Lymphocyte-to-monocyte ratio as the best simple predictor of bacterial infection in patients with liver cirrhosis. Int J Environ Res Public Health. 2020;17:1727.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Mean platelet volume as a potential predictor of cholesteatoma in children. J Craniofac Surg. 2016;27:575-8.
- [CrossRef] [PubMed] [Google Scholar]
- Association between platelet indices and the severity of the disease and mortality in patients with COVID-19. Eur Rev Med Pharmacol Sci. 2021;25:6731-40.
- [CrossRef] [PubMed] [Google Scholar]
- Platelet and mean platelet volume kinetics in adult patients with sepsis. Platelets. 2015;26:331-5.
- [CrossRef] [PubMed] [Google Scholar]
- Mean platelet volume is increased in infective endocarditis and decreases after treatment. Med Princ Pract. 2013;22:270-3.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Decreased mean platelet volume in children with acute rotavirus gastroenteritis. Platelets. 2014;25:51-4.
- [CrossRef] [PubMed] [Google Scholar]
- Mean platelet volume: A new predictor in confirming acute appendicitis diagnosis. Clin Appl Thromb Hemost. 2011;17:362-6.
- [CrossRef] [PubMed] [Google Scholar]
- Mean platelet volume as an indicator of disease severity in patients with acute pancreatitis. Clin Res Hepatol Gastroenterol. 2012;36:162-8.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of platelet indices in patients with deep neck space infection as a complication of acute tonsillitis. Tr-ENT. 2017;27:179-84.
- [Google Scholar]
- Hematologic and inflammatory parameters for determining severity of odontogenic infections at admission: A retrospective study. BMC Infect Dis. 2022;22:931.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Plateletcrit: A possible biomarker of inflammation in hepatitis A infection. Niger J Clin Pract. 2019;22:27-30.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of prognostic significance of hematological profiles after the intensive phase treatment in pulmonary tuberculosis patients from Romania. PLoS One. 2021;16:0249301.
- [Google Scholar]
- Lymphocyte-to-monocyte ratio predicts mortality in cirrhotic patients with septic shock. Am J Emerg Med. 2021;40:70-6.
- [CrossRef] [PubMed] [Google Scholar]






