Translate this page into:
Impact of telemedicine in STEMI care system: A five-year experience from Tamil Nadu, India
For correspondence: Prof Justin Paul Gnanaraj, Institute of Cardiology, Madras Medical College and Rajiv Gandhi Government General Hospital, Chennai 600 003, Tamil Nadu, India e-mail: drjustinpaul@yahoo.com
-
Received: ,
Accepted: ,
Abstract
Background & objectives
Timely reperfusion reduces mortality in ST-segment elevation myocardial infarction (STEMI). Telemedicine and social media have been shown to improve STEMI care in community settings as reported previously. We established a government-sponsored STEMI care system in the State of Tamil Nadu with a goal of enhancing guideline-directed revascularisation (GDR) in STEMI. This study aimed to improve GDR by networking non-percutaneous coronary intervention (PCI)-capable hospitals with PCI capable hospitals in a hub-and-spoke model and implementing telemedicine through social media groups.
Methods
Eighteen Government medical college hospitals were provided cardiac catheterisation laboratories and linked to 188 Taluk and non-PCI capable Government hospitals forming 18 STEMI clusters. Telemedicine guidance on STEMI management was provided through WhatsApp groups created for each cluster. Cumulative daily data on the number of STEMIs, the revascularisation provided, and mortality were collected through free online web forms. Annual cumulative data on STEMI volumes and GDR were analysed.
Results
A total of 71,907 individuals were treated for STEMI from 2019 to 2023. A 67 per cent annual increase in the total individuals treated for STEMI was observed. The proportion of individuals receiving pharmaco-invasive therapy (PIT) increased from 7.9 to 31.7 per cent. There was a 68 per cent increase in the individuals receiving primary PCI. The number of individuals without GDR decreased by 20 per cent. There was a 6.7-fold rise in the individuals referred from spoke to hub hospitals for catheter-based revascularization. Overall mortality showed a marginal decrease from 8.7 to 8.4 per cent.
Interpretation & conclusions
Findings of this study suggest that a government-sponsored STEMI care system in a hub-and-spoke model, guided by telemedicine through social media groups will improve GDR in STEMI care in developing nations.
Keywords
COVID-19
fibrinolysis
guideline directed revascularisation
hub-and-spoke model network
Timely reperfusion is critical for minimising morbidity and mortality related to ST-segment elevation myocardial infarction (STEMI). Randomised trials unequivocally support early reperfusion interventions in reducing mortality outcomes1,2. Although primary percutaneous coronary intervention (PPCI) is a class I indication for STEMI3,4, only six per cent of eligible patients receive it in the absence of a structured care delivery system. Furthermore, many eligible patients experience delayed or no revascularisation in developing nations5. Only a few hospitals in India provide round-the-clock PPCI services for STEMI6. Such facilities are rare in publicly funded healthcare systems. Expert consensus recommend a time-guided care system for early fibrinolysis at non-PCI capable centres in India, followed by referral to PCI-capable hospitals for pharmaco-invasive therapy (PIT)7. A study from Belgium has demonstrated that networking of non-PCI-capable hospitals to PCI-capable hospitals in a hub-and-spoke model improved adherence to reperfusion guidelines over time in STEMI8. The Tamil Nadu (TN) STEMI pilot study9,10, implemented under a special order by the Government of Tamil Nadu, demonstrated that the hub-and-spoke model facilitated early revascularisation in STEMI in Tamil Nadu, India. Telemedicine has been suggested as a tool to optimise care in STEMI networks11. The current study aimed to analyse the preliminary outcome of implementing a telemedicine incorporated STEMI care system in improving guideline-directed revascularisation (GDR) in STEMI and the role of social media in facilitating effective implementation.
Materials & Methods
This study was undertaken by the heart attack management program pillar of the Tamil Nadu Accident and Emergency Initiative (TAEI) of National Health Mission, Tamil Nadu.
Establishing the STEMI care system
The Tamil Nadu Government Heart Attack Management Program was developed to provide free of cost GDR to individuals with STEMI, irrespective of the time, location, and nativity. Tamil Nadu, the tenth largest State in India, has an area of 130,000 square kilometres, a population of 82 million, and is well-networked by at least 17,000 Km of highways. Eighteen government medical college hospitals were identified as hub hospitals. All of these were equipped with new cardiac catheterisation laboratories, to offer round-the-clock or office-hour PPCI based on the available human resources. Based on round-the-clock availability of medical officers, emergency rooms / intensive care units, and electrocardiograms (ECGs), 188 district or Taluk government hospitals were identified as spoke hospitals. A STEMI cluster was formed by networking 10-15 spoke hospitals with one hub hospital based on geographical proximity and transport logistics. Spoke hospitals were empowered to take ECGs for individuals presenting with chest pain, rule in or rule out STEMI with remote guidance from hub hospitals, and initiate fibrinolytic therapy when appropriate. After fibrinolysis, the spoke hospitals were encouraged to refer patients to the linked hub hospitals for PIT. This networking was done in two phases. During phase I of the programme, between 2017 and 2018, 12 hubs were linked to 154 spokes to form 12 STEMI clusters. During Phase II, between 2019 and 2020, six hub hospitals were linked to 34 spoke hospitals to create six more STEMI clusters (Supplementary Fig. 1). The extensive network of the Government’s 108 emergency ambulance services (Supplementary Fig. 2) was utilised to transport patients to the hub or spoke hospitals and also transfer them between facilities, all free of cost. The Chief Minster’s comprehensive health insurance scheme covered the treatment expenditures. This system of care was formally published as the government’s cardiac care policy by a government order [Health and Family Welfare (EAP II-1) Department (Ms) No 272].
Standard operating protocol
A standard operating protocol (SOP), peer-reviewed by international and national experts, was prepared to ensure uniformity in the management of STEMI across the system. GDR included PPCI performed within 12-24 h of symptom onset, fibrinolysis within 6-12 h of symptom onset, and timely PIT within 3-24 h of fibrinolysis12-14. Elective coronary procedures, done after the recommended time intervals, were not included in the GDR. Nodal officers were identified in each of the participating hubs and spoke to oversee the implementation of the protocol. In the spoke hospitals, timely diagnosis and immediate fibrinolysis, when indicated, were the key objectives. Post-lysis, patients were to be transferred to linked hub hospitals within 3-24 h for elective or emergency angiogram and revascularization as necessary. In the hub hospitals, PPCI was the recommended reperfusion strategy. However, when PPCI was not logistically feasible, fibrinolysis and PIT were recommended. Triage protocols and management flow charts were displayed in the study hospitals.
Monitoring and data collection
A State programme management unit (SPMU), led by the State nodal officer was established at Madras Medical College, to oversee and monitor the programme implementation. Each hub-and-spoke hospital independently submitted their cumulative daily data through an online spreadsheet created using Google Forms. Data collected from each participating hospital every day included the number of patients with STEMI reported within 48 h of symptom onset, number of PPCI, number of fibrinolysis done, number of PIT, interfacility transfer between hubs and spokes, number of STEMI deaths, number of non-STEMI, number of non-STEMI death among others. Based on the data received, the SPMU provided weekly and monthly feedback to the clusters to help improve the proportion of individuals receiving GDR.
Training the system
All the doctors, nurses, and 108 emergency ambulance technicians of the spoke and hub hospitals were provided training at their respective hub hospitals in STEMI diagnosis, management, counselling, appropriate referral, and data collection in three phases to ensure uniform protocol implementation, under the guidance of the State Nodal Officer. The financial support for the training was provided by the Tamil Nadu Innovation Initiative of the State’s planning commission. Though the first phase of the training started in October 2019, with the onset of the COVID-19 pandemic, the training was completed only in late 2022 for all 18 clusters.
Telemedicine and networking for STEMI management
To guide case-specific management of suspected myocardial infarction, 18 WhatsApp groups were created, one per cluster. These groups enabled seamless communication between hub hospital cardiologists and spoke hospital teams. Each group included hub cardiologists, spoke hospital medical officers, assigned nurses, the hub data entry operator, administrative members from National Health Mission (NHM), SPMU, and the State Nodal Officer.
Operational Guidelines for telemedicine implementation, training, and coordination included, (i) Sharing de-identified clinical data: Spoke Medical officers shared patient details and ECGs in WhatsApp groups to seek diagnostic and management guidance; (ii) Telemedicine support: Hub hospital cardiologists provided real-time advice on diagnosing STEMI and selecting the most appropriate GDR for STEMI; (iii) Direct communication: Duty cardiologists at the hub hospital were available via dedicated mobile numbers for additional clarifications; (iv) Telemedicine guidance: The SPMU monitored and ensured timely telemedicine guidance through active coordination between the hub-and-spoke hospitals via WhatsApp; (v) Interfacility transfers: Transfers within clusters were streamlined through prior communication to ensure smooth GDR protocol execution. Hub hospitals provided feedback to the spoke medical officers on transferred patients; (vi) Online training: The SPMU conducted periodic training on SOPs via Zoom; (vii) Cluster-level education: Hub hospitals regularly trained spoke hospital team on STEMI recognition and management through online sessions.
COVID-19 pandemic
During the COVID-19 pandemic, most human resources involved in STEMI care were diverted to pandemic management. However, the coronary care units continued functioning with a minimum workforce, with thrombolysis as the predominant mode of revascularisation. Telemedicine support and data collection using social and internet media continued to be effective. Two focused recommendations for managing cardiac patients during the pandemic were developed to guide our system to optimise STEMI care during the pandemic. A position statement was developed to guide antithrombotic therapy during the COVID pandemic to help healthcare professionals optimise treatment15.
Periodic review of the STEMI care system
A monthly review of the performance of the various clusters was done by a team of cardiology experts under the auspices of the NHM, Tamil Nadu. Methodologies and guidelines were developed for the reviewers and the reviewed teams to ensure a goal-oriented review. The hub-and-spoke coordination, the type of revascularisation provided, and mortality were assessed, and suggestions for improvement were provided. The review also considered infrastructural shortcomings and evaluation of the steps taken to optimise care. Feedback was periodically obtained from the participants to identify areas that need improvement.
Data analysis
The cumulative annual data on the type of revascularisation provided, the proportion of GDR, and mortality were compared over the five periods from January 2019 to December 2023. A comparison was done separately for the data from the Phase I and II hubs. In addition, the volume of STEMI, the revascularisation pattern, and the outcome in our care system during the COVID pandemic were analysed. The cumulative data of the peak pandemic period (April to December 2020) were compared with that of the corresponding period in 2019 (April to December 2019) to identify the impact of the pandemic on our system. Categorical variables have been presented as frequencies and percentages.
Results
In total, 71,907 individuals with STEMI were treated over five years (2019-2023). During this period, the system achieved a 67 per cent increase in the number of individuals treated, a 300 per cent rise in PIT use, and a 20 per cent reduction in the number of individuals not receiving GDR (Table I and Fig. 1). PIT use increased by 3.6 and 28 times in Phase I and Phase II hubs, respectively. The proportion of individuals receiving GDR also improved significantly during the study, particularly in Phase II hubs, driven by an increase in use of fibrinolysis (Tables I, IIA and B). PPCI usage rose by 68 per cent system wide and and by 70 per cent in Phase I hubs.
| Year | Total number of STEMI patients | Primary PCI, n (%) | Fibrinolysis, n (%) | PI PCI, n (%) | Death, n (%) | Guideline based revascularisation, n (%) |
|---|---|---|---|---|---|---|
| 2019 | 11363 | 563 (5) | 7342 (64.6) | 898 (7.9) | 994 (8.7) | 7905 (69.6) |
| 2020 | 11242 | 154 (1.4) | 7941 (70.6) | 279 (3.5) | 1030 (9.2) | 8095 (72) |
| 2021 | 13287 | 118 (0.9) | 9972 (75.1) | 1154 (11.6) | 1175 (8.8) | 10,090 (75.9) |
| 2022 | 17030 | 990 (5.8) | 11993(70.4) | 3201 (27) | 1432 (8.4) | 12,983 (76.3) |
| 2023 | 18985 | 1588 (8.4) | 12804 (67.4) | 4058 (31.7) | 1573 (8.3) | 14392 (75.8) |
| Total | 71907 | 3413 (4.8) | 50052 (69.6) | 9590 (13.3) | 6204 (8.6) | 53465 (74.4) |
STEMI, ST-segment elevation myocardial infarction; PCI, percutaneous coronary intervention; PI PCI, pharmaco-invasive PCI
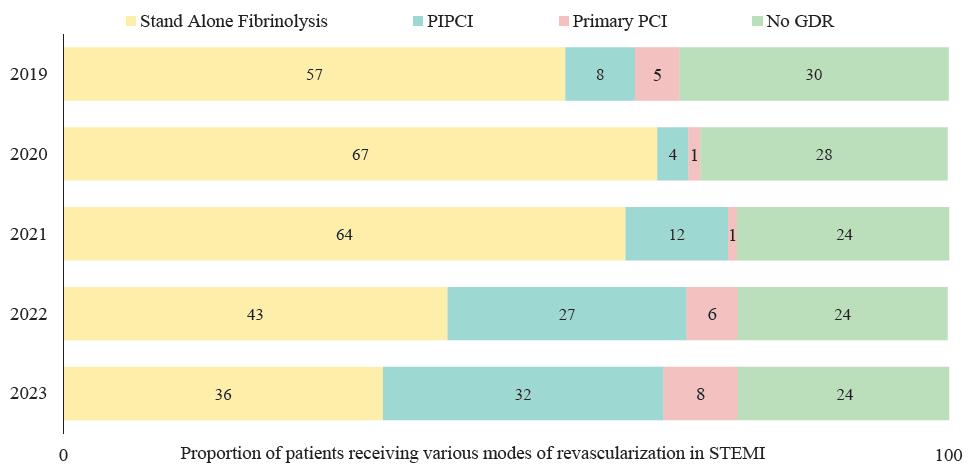
- Proportion STEMI patients receiving various modes of revascularisation in STEMI from 2019 to 2023 in the Tamil Nadu Government heart attack management program.
| Year | Total STEMI (n) | Primary PCI, n (%) | Fibrinolysis, n (%) | PI PCI, n (%) | Death, n (%) | Guideline based revascularization, n (%) |
|---|---|---|---|---|---|---|
| 2019 | 9619 | 548 (5.7) | 6439 (66.9) | 882 (9.1) | 845 (8.8) | 6987 (72.6) |
| 2020 | 8891 | 148 (1.7) | 6279 (70.6) | 227 (3.6) | 778 (8.8) | 6427 (72.3) |
| 2021 | 10959 | 110 (1) | 7929 (72.4) | 1097 (13.8) | 993 (9.1) | 8039 (73.4) |
| 2022 | 14191 | 977 (6.9) | 9549 (67.3) | 2874 (30.1) | 1259 (8.9) | 10,526 (74.2) |
| 2023 | 16109 | 1563 (9.7) | 10323 (64.1) | 3431 (33.2) | 1406 (8.7) | 11886 (73.8) |
| Total | 59769 | 3346 (5.6) | 40519 (67.8) | 8511 (21) | 5281(8.8) | 43865 (73.4) |
| Year | Total STEMI (n) | Primary PCI, n (%) | Fibrinolysis, n (%) | PI PCI, n (%) | Death, n (%) | Guideline based revascularization, n (%) |
|---|---|---|---|---|---|---|
| 2019 | 1744 | 15 (0.9) | 903 (51.7) | 16 (0.9) | 149 (8.5) | 918 (52.6) |
| 2020 | 2351 | 6 (0.3) | 1662 (70.6) | 52 (2.2) | 252 (10.7) | 1668 (70.9) |
| 2021 | 2328 | 8 (0.3) | 2043 (87.8) | 57 (2.4) | 182 (7.8) | 2051 (88.1) |
| 2022 | 2839 | 13 (0.5) | 2444 (86.1) | 327 (11.5) | 173 (6.1) | 2457 (86.5) |
| 2023 | 2876 | 25 (0.9) | 2481 (86.3) | 627 (25.3) | 167 (5.8) | 2506 (87.1) |
| Total | 12138 | 67 (0.6) | 9533 (78.6) | 1079 (8.8) | 923 (7.6) | 9600 (79.1) |
Over five years, overall mortality, including Phase I and II hubs, saw a modest 4.6 per cent relative reduction, from 8.7 to 8.3 per cent. Phase II hubs, however, achieved a striking 68 per cent reduction, from 8.5 to 5.8 per cent (Fig. 2). This mortality reduction in Phase II hubs aligned with a rise in GDR from 52.6 to 87.1 per cent, driven largely by increased fibrinolysis rates, and pharmaco-invasive PCI rates, which rose from 51.7 to 86.3 per cent and 0.9 to 25.3 per cent, respectively. Referrals for PIT from spoke to hub hospitals increased by 6.7-fold over five years. Additionally, the proportion of individuals treated at the hub hospitals referred from linked spoke hospitals rose from 5.9 to 23.8 per cent (Fig. 3).
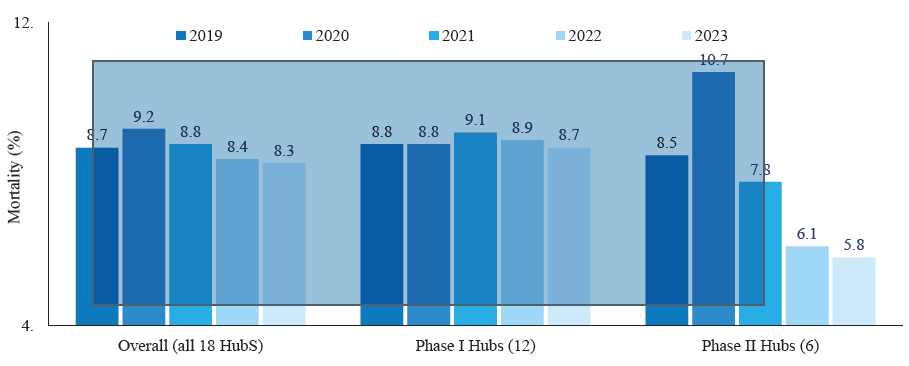
- Mortality trend in STEMI over five years: Tamil Nadu Government heart attack management program: all hubs, phase I hubs and phase II hubs.
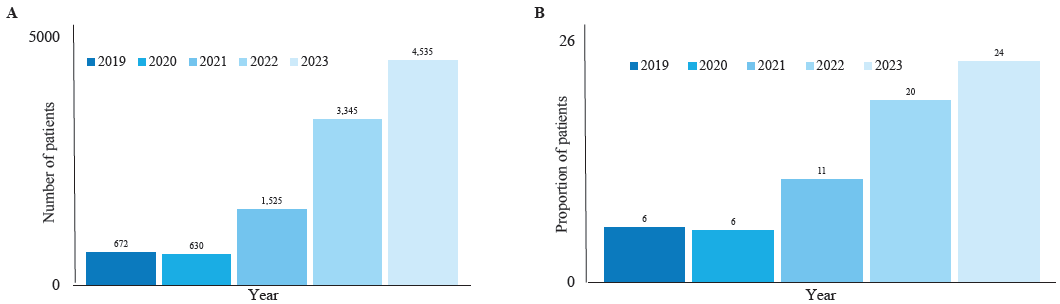
- Number of individuals with STEMI referred from the spoke hospitals to hub hospitals for catheter-based therapies.
COVID experience
There was a significant drop in the number of STEMI cases reported during 2020, corresponding to an increase in reported COVID-19 cases16 (Fig. 4A). There was a sharp decrease in the proportion of individuals undergoing catheter-based revascularisation during the pandemic period. However, there was a 12.3 per cent absolute increase in the proportion of individuals receiving fibrinolysis (Fig. 4B), and there was no change in mortality during this period.
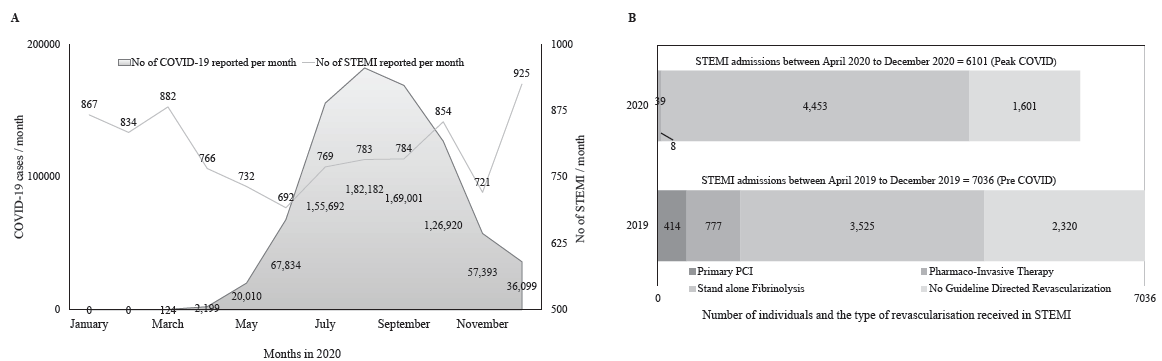
- (A) Relationship of number of cases of STEMI reported to the number of cases of COVID-19 reported in the State. (B) Comparison of STEMI cases and treatment modalities during peak COVID-19 months vs. corresponding months in the previous year.
Discussion
Our study brings key information regarding establishing a new STEMI care system in developing nations. Through this study, we demonstrated that social media groups are a cost-effective way of networking hubs and spokes into a STEMI care model to provide telemedicine guidance for early diagnosis and management of STEMI. Though WhatsApp groups have been used for the management of STEMI in the past17,18, this is the first time these have been used for telemedicine guidance in a State-sponsored STEMI care system. Latin America Telemedicine Infarct Network (LATIN) used the services of three remote telemedicine command centres exclusively for telemedicine guidance from expert cardiologists in STEMI management19. However, hub hospital cardiologists offered telemedicine guidance to their respective clusters in our system. In addition, we used these groups for pre-arrival intimation before the interfacility patient transfers and monitored the networking process. AHA scientific statement highlights the importance of this coordination between STEMI referring hospitals, receiving centres, and interfacility transport providers20.
Telemedicine to improve GDR
Telemedicine, implemented through social media groups, increased the number of patients treated within the STEMI care system, improved GDR rates, and reduced mortality. Notably, this system of care also increased referrals from spoke hospitals to hub hospitals for catheter-based therapies. By 2022, nearly one in five patients treated at hub hospitals came from spoke hospitals. The modest decrease in absolute mortality may reflect the small increase in GDR rates from 69.6 to 74.4 per cent (4.7% increase). In contrast, the phase II hubs, with a 29.5 per cent absolute GDR increase, showed a more significant reduction in mortality. This suggests that mortality improvements align more closely with the magnitude of GDR change than the type of GDR. Two meta-analyses of RCTs comparing PPCI and fibrinolysis report only about a two per cent absolute decrease in mortality21,22. Therefore while striving to provide PPCI universally, timely fibrinolysis must not be overlooked23-an especially critical message for low- and middle- income countries (LMICs) and low-income countries (LICs), where many STEMI patients receive no revascularisation24. Establishing STEMI diagnosis and fibrinolytic therapy systems, which are cost-effective and easier to implement, should be prioritised. Fibrinolysis serves as the foundation for developing and establishing PIT systems, as healthcare capabilities expand.
Telemedicine in data collection and monitoring
We demonstrated that cumulative daily data collection—using free online forms and spreadsheets – can effectively assess, monitor, and improve GDR in STEMI care. This approach provided valuable insights into STEMI volumes and GDR rates at each hospital within the system. Leveraging this data, we could identify the type and extent of support needed by participating hospitals to enhance GDR outcomes. This method holds particular relevance in developing nations, where digitised health records are often unavailable.
Sustained care during COVID pandemic
This model sustained its functionality during the COVID-19 pandemic. Congruent to the previous reports, this study showed a decrease in STEMI reported to our healthcare systems during the pandemic25,26. Despite a shift in the mode of revascularisation to predominantly fibrinolysis during the pandemic, the STEMI mortality remained unchanged, suggesting fibrinolysis is an acceptable revascularisation in unprecedented situations like this. A recent meta-analysis of 14 studies involving 50,136 patients similarly reported increased use of fibrinolysis without change in all-cause mortality in STEMI during COVID-1927.
Despite the benefits of this model, implementing a State-wide system of care for STEMI posed significant challenges. These included equipping both hub-and-spoke hospitals with essential infrastructure and equipment, ensuring round-the-clock availability of trained personnel – including cardiologists, medical officers, catheterisation laboratory nurses and catheterisation laboratory technicians – and carefully planning workflow distribution. Additionally organising regular training on care processes and protocols, maintaining a steady supply of necessary consumables and hardware, and establishing dedicated monitoring and support systems were critical hurdles. Public awareness campaigns and educating beneficiaries about the system of care were essential but demanding. Finally, securing sufficient financial resources for both recurring (e.g., human resources, consumables, etc.) and non-recurring (e.g., infrastructure, equipment, etc.) expenditures remained a major challenge.
However, these challenges were systematically addressed through the proactive efforts of the Government of Tamil Nadu. Despite the robust implementation measures, the modest increase observed in primary PCI and PIT rates underscores the complexity and scale of these challenges.
This study highlights the key learning points from the first State-sponsored system of care for STEMI in a developing nation, underscoring its value in addressing STEMI management challenges in resource-limited settings. However, several limitations must be acknowledged. Individual patient-level data was not collected, and critical metrics such as symptom onset to first medical contact time, door-to-needle time, door-in-to-door out time, door-to-balloon time, causes of delay, and complications were unavailable. Additionally, cumulative daily STEMI reperfusion data collection from all 188 spoke hospitals could not be fully implemented, limiting our ability to provide a complete picture of system-wide performance. While all STEMI patients within 48 h of symptom onset were included in the daily data entry, the total number of revascularisation-eligible STEMI per day were not captured. This omission could have led to an underestimation of the true proportion of GDR achieved within our system.
While the STEMI care system we developed seems appropriate for Tamil Nadu, it may not serve as a universal model for other regions in India or globally. Each nation or healthcare system must design its own STEMI care system based on factors such as geographical landscape and highway network, number and proximity of potential hub-and-spoke hospitals, the strength of the ambulance network (ambulances are the currency of a STEMI care system), availability of qualified cardiologists and medical officers, the health care system’s capacity is to expand workforce and infrastructure, the role of State healthcare or insurance in funding, and mechanisms to ensure a regular supply of consumables for revascularisation therapy. The chosen reperfusion strategy – whether fibrinolysis, PIT, or PPCI—must align with the logistics and capabilities of the public healthcare system. Since timely PPCI remains challenging even in developed nations, PIT remains the preferred revascularisation strategy in India and most other LMICs. Developing a STEMI care system centred on PIT requires a strong focus on timely STEMI diagnosis and fibrinolysis, which forms the foundation for establishing such systems.
Overall, the experience from this study suggests that establishing a State-sponsored STEMI care system in a hub-and-spoke model and leveraging social media groups for networking and telemedicine, improves GDR rates. Such groups can facilitate chest pain evaluation, enable timely and appropriate fibrinolysis in non-PCI-capable hospitals, and ensure efficient post-fibrinolysis transfer to linked hub hospitals. Additionally, daily data collection using Google Forms can support a structured process for monitoring and review, further enhancing system performance. The model has also demonstrated its resilience during unprecedented crises, such as the COVID-19 pandemic, ensuring continuity in care delivery. Appropriate revascularisation in STEMI is a social and governmental responsibility. Every health care system must develop customised appropriate STEMI care systems, to ensure that all patients with STEMI receives appropriate and timely GDR. The findings have important implications in managing STEMI and other time-sensitive medical emergencies in resource-limited healthcare settings worldwide.
Acknowledgment
The authors acknowledge the proactive efforts and dedication of the entire healthcare machinery of the Government of Tamil Nadu in approving and implementing this system of care. This includes Ministry of Health and Family Welfare, National Health Mission, Tamil Nadu Health Systems Project, Chief Ministers Comprehensive Health Insurance Scheme, 108 Emergency Ambulance Services-Tamil Nadu, Tamil Nadu Medical Services Corporation, Tamil Nadu Innovation Initiative -State Planning Commission, Directorate of Medical Education & Research, Directorate of Medical Services and Directorate of Public Health. The authors also extend their heartfelt thanks to all the cardiologists of the 18 hub hospitals and the medical officers of the 188 spoke hospitals for their active involvement, hard work, and support in implementing this system of care. Without the unwavering support of the entire healthcare system, a programme of this scale would not have been possible.
Financial support & sponsorship
The Government of Tamil Nadu funded the purchase and establishment of cardiac catheterization laboratories through the National Health Mission, Tamil Nadu in this study. The networking of cluster hospitals and training programmes were supported by the Tamil Nadu Innovation Initiative of the Planning Commission, Government of Tamil Nadu.
Conflicts of Interest
None.
Use of Artificial Intelligence (AI)-Assisted Technology for manuscript preparation
The authors confirm that there was no use of AI-assisted technology for assisting in the writing of the manuscript and no images were manipulated using AI.
References
- Effectiveness of intravenous thrombolytic treatment in acute myocardial infarction. Gruppo Italiano per lo Studio della Streptochinasi nell’Infarto Miocardico (GISSI) Lancet. 1986;327:397-402.
- [Google Scholar]
- Randomised trial of intravenous streptokinase, oral aspirin, both, or neither among 17,187 cases of suspected acute myocardial infarction: ISIS-2. ISIS-2 (Second International Study of Infarct Survival) Collaborative Group. Lancet. 1988;332:349-60.
- [Google Scholar]
- 2021 ACC/AHA/SCAI Guideline for Coronary Artery Revascularization. A report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2022;79:e21-129.
- [CrossRef] [PubMed] [Google Scholar]
- 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The task force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European society of cardiology (ESC) Eur Heart J. 2018;39:119-77.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment and outcomes of acute coronary syndromes in India (CREATE): A prospective analysis of registry data. Lancet. 2008;371:1435-42.
- [CrossRef] [PubMed] [Google Scholar]
- Choosing the right model for STEMI care in India - focus should remain on providing timely fibrinolytic therapy, for now. Indian J Med Res. 2022;156:17-20.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- 2013 consensus statement for early reperfusion and pharmaco-invasive approach in patients presenting with chest pain diagnosed as STEMI (ST elevation myocardial infarction) in an Indian setting. J Assoc Physicians India. 2014;62:473-83.
- [PubMed] [Google Scholar]
- STEMI mortality in community hospitals versus PCI-capable hospitals: Results from a nationwide STEMI network programme. Eur Heart J Acute Cardiovasc Care. 2012;1:40-7.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Protocol for a prospective, controlled study of assertive and timely reperfusion for patients with ST-segment elevation myocardial infarction in Tamil Nadu: The TN-STEMI programme. BMJ Open. 2013;3:e003850.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- A system of care for patients with ST-segment elevation myocardial infarction in India. JAMA Cardiol. 2017;2:498.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Telemedicine: The future of global STEMI care. Interv Cardiol Clin. 2012;1:623-9.
- [CrossRef] [PubMed] [Google Scholar]
- Cardiological society of India: Position statement for the management of ST elevation myocardial infarction in India. Indian Heart J. 2017;69:S63-97.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction. J Am College Cardiol. 2013;61:e78-e140.
- [Google Scholar]
- ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J. 2012;33:2569-619.
- [CrossRef] [PubMed] [Google Scholar]
- Antithrombotic therapy in COVID-19 - A scientific position statement by heart disease management program, national health mission, government of Tamil Nadu. J Assoc Physicians India. 2021;69:82-7.
- [PubMed] [Google Scholar]
- Impact of COVID-19 pandemic on a developing STEMI care system from a low-middle income country- a prospective observational study. European Heart J. 2021;42
- [CrossRef] [Google Scholar]
- Time-to-reperfusion in STEMI undergoing interhospital transfer using smartphone and WhatsApp messenger. Am J Emerg Med. 2015;33:1382-4.
- [CrossRef] [PubMed] [Google Scholar]
- Implementing “Chest Pain Pathway” Using Smartphone Messaging Application “WhatsApp” as a Corrective Action Plan to Improve Ischemia Time in “ST-Elevation Myocardial Infarction” in Primary PCI Capable Center “WhatsApp-STEMI Trial”. Crit Pathw Cardiol. 2021;20:179-84.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Impact of a telemedicine-guided, population-based, STEMI network on reperfusion strategy, efficiency, and outcomes. Asia Intervention. 2021;7:18-26.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Delays in ST-elevation myocardial infarction care during the COVID-19 lockdown: An observational study. CJC Open. 2020;3:565-73.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Comparison of primary coronary angioplasty and intravenous thrombolytic therapy for acute myocardial infarction: A quantitative review. JAMA. 1997;278:2093-8.
- [PubMed] [Google Scholar]
- Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials. Lancet. 2003;361:13-20.
- [CrossRef] [PubMed] [Google Scholar]
- Reperfusion paradox in ST-segment elevation myocardial infarction. Ann Intern Med. 2011;155:389-91.
- [CrossRef] [PubMed] [Google Scholar]
- Underutilization of fibrinolysis despite timely arrival in STEMI. JACC Asia. 2023;3:534.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Impact of coronavirus disease 2019 (COVID-19) outbreak on ST-segment-Elevation myocardial infarction care in Hong Kong, China. Circ: Cardiovascular Quality and Outcomes. 2020;13:e006631.
- [Google Scholar]
- COVID-19 pandemic and admission rates for and management of acute coronary syndromes in England. Lancet. 2020;396:381-9.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Effect of fibrinolytic therapy on ST-elevation myocardial infarction clinical outcomes during the COVID-19 pandemic: A systematic review and meta-analysis. World J Cardiol. 2023;15:309-23.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]






