Translate this page into:
ICMR's tryst with HIV epidemic in India: 1986-1991
Reprint requests: Dr Prema Ramachandran, Director, Nutrition Foundation of India C-13, Qutab Institutional Area, New Delhi 110 016, India e-mail: premaramachandran@gmail.com
-
Received: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
The Indian Council of Medical Research (ICMR) undertook screening of asymptomatic persons from high risk group with the ELISA test for HIV infection in 1986 and found that HIV infection has reached India. ICMR in collaboration with the central and State health services initiated the national sero- surveillance programme for HIV infection in 43 surveillance and five reference centres to determine the major modes of transmission and magnitude of infection. Data from the sero-surveillance showed that HIV infection was present in all the known high risk groups and in the general population in all the States both in urban and rural areas. HIV was getting transmitted through all the known modes of transmission. In most States heterosexual transmission was predominant but in Manipur intravenous (iv) drug use was the most common mode of transmission. Prevalence of HIV infection in high risk groups was not high and that in low risk groups was quite low. ICMR initiated hospital based sentinel surveillance in high risk groups and general population to obtain time trends in seroprevalence. Between 1986 and 1991, National AIDS Programme was carried out as a collaborative effort of ICMR, and central and State health services. As the dimensions of the epidemic unfolded, rational evidence based interventions which could be implemented within the existing health system, were initiated. National AIDS Control Programme (NACP) continued and upscaled all these interventions. Effective implementation of a multi-pronged, rational strategy for HIV infection containment and control right from the initial stages, and dedicated work done by committed professionals belonging to government and voluntary sectors, cultural ethos of the country, responsible behaviour of the population and relatively low iv drug use have resulted in rapid decline in new infection and in prevalence of infection within a quarter of a century after the initial detection of HIV.
Keywords
AIDS control programme
HIV epidemic
HIV infection
sentinel surveillance
sero-surveillance
Introduction
The second half of the twentieth century witnessed introduction of newer diagnostic tests, antibiotics, contraceptives, anaesthetics and operative techniques bringing with them unparalleled opportunity for management of health problems. These when coupled with improvement in access to health care at affordable cost in developing and developed countries, led to substantial improvement in the health status of population. The steep fall in morbidity and mortality due to infections led some health professionals to dream of “conquest of communicable diseases”. But these developments were not unmixed blessings. Widespread use of contraceptives to prevent pregnancy, and antibiotics to treat sexually transmitted diseases (STDs), resulted in behaviuoral changes in the populations, setting the stage for a potentially explosive epidemic of sexually transmitted diseases. Widespread use of antiseptics and antibiotics led to slackening of the infection control and waste management practices in health care settings, thereby increasing the risk of accidental spread of infections during health care. The microbes have shown tremendous capacity to adapt to and survive under a variety of adverse environmental conditions. With unfailing regularity newer microbes evolved and some of them caused diseases in human beings. Viewed in this perspective, the AIDS (acquired immune deficiency syndrome) pandemic has all the inevitability of a Greek Tragedy.
AIDS was first described in 1981 as an obscure disease of unknown aetiology affecting young men who had sex with men (MSM) and intravenous (iv) drug users in USA1. In the next two years, AIDS patients from these two groups were reported across North America, Western Europe and Australia. Simultaneously, a severe wasting disease in young men, women and young children (Slim's disease) was reported from Sub-Saharan Africa2. In 1984, human immunodeficiency virus (HIV) was isolated3 and in the subsequent year, ELISA tests for detection of antibodies to this virus were developed. The ELISA tests showed that AIDS cases reported in USA, Europe and Australia and the Sub- Saharan epidemic of Slim's disease were caused by the same organism45. AIDS pandemic was recognized as a major global public health problem and the global registry for reporting of AIDS cases was set up by the WHO in 19866. No AIDS case was reported from Asia the home of over a third of the global population, till 1985.
ICMR's search for HIV infection
ICMR Task Force on AIDS, met in October 1985 and recommended that in view of the potential threat posed by HIV infection, ICMR should initiate sero-surveillance of HIV infection (using the ELISA test) among asymptomatic persons from high risk groups and find out whether the infection has reached India. The National Institute of Virology in Pune and the ICMR's Virology Research Centre at Christian Medical College, Vellore, tested serum samples from female sex workers in Chennai and Mumbai, respectively and in April 1986, reported presence of HIV infection in India7. The first two AIDS cases in Indians were reported in May 1986; one had received blood transfusion abroad7 and the other received blood product infusion abroad. These reports sounded the warning bell that HIV infection has entered India1. Spurred by the Indian reports, other Asian countries followed similar approach and soon confirmed presence of asymptomatic HIV infected persons in their countries.
ICMR's sero-surveillance programme for HIV infections
In May 1986, ICMR AIDS Task Force reviewed these findings and recommended that a national sero-surveillance programme for screening high risk and vulnerable groups for HIV infection should be initiated. India had the unique distinction of being the first country in the world to initiate under ICMR a systematic national sero-surveillance among men and women belonging to high risk and vulnerable groups to determine the major modes of transmission of HIV in the country and estimate the magnitude of the infection. Initiating a national clinical and serological surveil-lance for HIV infection in India was a major task. It was decided that the national surveil-lance would be established as a collaborative effort of ICMR, Directorate General of Health Services (DGHS), and State Health Authorities. In six months ICMR established a network of five reference centres and 43 surveillance centres7 (Fig. 1). These centres functioned within the existing infrastructure in medical colleges/ICMR institutions with the minimum essential additional input of a laboratory technician. Within the next six months the Principal Investigators (usually from Department of Microbiology) and laboratory personnel were trained in the detection of HIV infection by ELISA. The five reference centres undertook confirmation of the infection by Western blot tests7. Between 1986 and 1991 every year (i) the Ministry of Health provided the funds from the STD programme, for procuring the needed equipment and consumables (kits) essential for sero-surveillance for HIV infection. ICMR funded the budget of the surveillance and reference centres and the co-ordinating unit at the ICMR headquarters; (ii) WHO took the responsibility of procuring the ELISA readers, ELISA and Western blot kits and delivering these in Delhi to ICMR; (iii) all the major Delhi institutions with large cold rooms and all major ICMR institutions in different parts of the country with good cold room facilities, stored the ELISA and Western blot kits required for the surveillance centres. Each institution took the responsibility of checking the cold room on a daily basis for ensuring that the kits have been stored safely at the right temperature; (iv) as courier services were in infancy in India at that time, chiefs of various technical divisions and scientists from ICMR headquarters, experts coming to ICMR meetings became the committed careful couriers for ferrying safely precious ELISA and Western blot kits to the reference centres, ICMR institutions and surveillance centres. If ELISA kits were urgently needed by surveillance centres, they persuaded academia, administrative and judicial service officers from their city who were coming to Delhi for official work to bring back the kits. These unorthodox steps ensured safe transit of the kits at a nominal cost; and (v) all surveillance and reference centres reported the findings every month and the monthly report and major findings were reported every month in the ICMR Bulletin, an in-house bulletin of the ICMR. November/December issues of the ICMR Bulletin always had the comprehensive article on ongoing activities in HIV /AIDS programme7–13.

- AIDS surveillance centres and reference centres.
Data from the sero-surveillance in the first two years showed that HIV infection was present in all the States where testing was done. HIV infection was detected in high risk groups such as sex workers, iv drug users, sexually promiscuous persons and recognised vulnerable groups such as those receiving repeated blood transfusion and blood product infusions in the previous five years. HIV positive persons were detected among pregnant women (spouse to spouse transmission as well as sex workers who were pregnant), professional and voluntary blood donors. It was obvious that HIV infection had reached the general population. HIV positive infants born to seropositive mothers proved that mother-to-child transmission was happening in the country. Detection of HIV positive children who had received multiple blood transfusions and blood product infusions in the earlier years documented that transmission of HIV infection through infected blood occurred in the country. In most of the States heterosexual transmission was the major mode of HIV transmission. In Manipur, iv drug use was the predominant mode of transmission of HIV infection.
It was clear that in India: (i) HIV infection transmission was occurring through all known modes of transmission; (ii) HIV infection was present in all the recognised high risk groups and general population in all States of the country both in urban and rural areas; (iii) prevalence of HIV infection was not high in the high risk groups; highest prevalence was reported in iv drug users; female sex workers had the second highest prevalence; and (iv) prevalence of HIV infection in general population was very low.
Inter-State differences in prevalence of HIV infection
Data from ongoing ICMR HIV sero-surveillance indicated that there were substantial inter-State and urban rural differences in the prevalence of HIV infection8. These differences might in part be due to variations in the type and number of persons screened and/or due to differences in actual prevalence of HIV infection. The load of HIV infection in the community depends upon the prevalence of infection in three groups of population – the high-risk group, the interphase group and the low risk group. The high risk group (HRG) such as commercial sex workers, iv drug users, form relatively very small proportion of the population. Soon after the introduction of infection in the community, there is a steep rise in prevalence of infection in this group because they are frequently exposed to the risk of infection. The interphase group is a somewhat larger group who acquires the infection from HRG and transmits it to other uninfected persons from HRG and to the low risk general population. In the setting where heterosexual transmission is the major mode of transmission, the interphase group consists mainly of men and women who have multiple sex partners. They form the link through which infection spreads to the numerically vast low risk group of the general population. The general population (low risk group) acquires HIV infection mainly from spouses who have multiple sex partners (Fig. 2)13. The size of the three groups and the extent of the interphase between them determine the magnitude of the HIV infection in any country or community. Data from ongoing socio-behavioural studies indicated that these factors account for most of the observed differences between States in the prevalence of HIV infection.
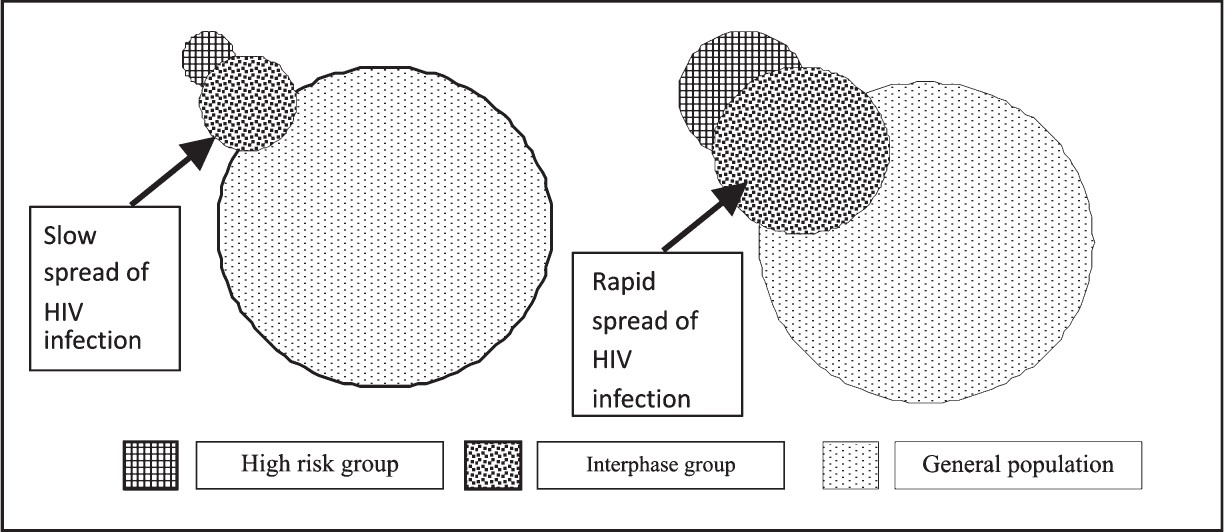
- Spread of HIV infection in population.
ICMR's sentinel surveillance for HIV infection
In India, HIV infection was detected in the early phase of HIV epidemic. It was essential to obtain information on time trends in prevalence of infection in the selected high risk groups and general population attending surveillance centres so that the course of epidemic could be monitored at national and State levels. This is an essential prerequisite for initiation of region specific timely interventions and also for monitoring the impact of ongoing interventions. ICMR drew up the protocol and initiated a hospital based unlinked anonymous sentinel surveillance in selected high risk groups and general population in all the regions of the country1213. Sentinel surveillance was continued and considerably expanded under National AIDS Control Programme (NACP) 1, 2 and 314. Data from sentinel surveillance showed that there was a progressive increase in the seropositivity rates in the nineties but in the last decade the steepness of the slope of the epidemic curve decreased and in many regions a plateau was reached14.
ICMR and national AIDS programme
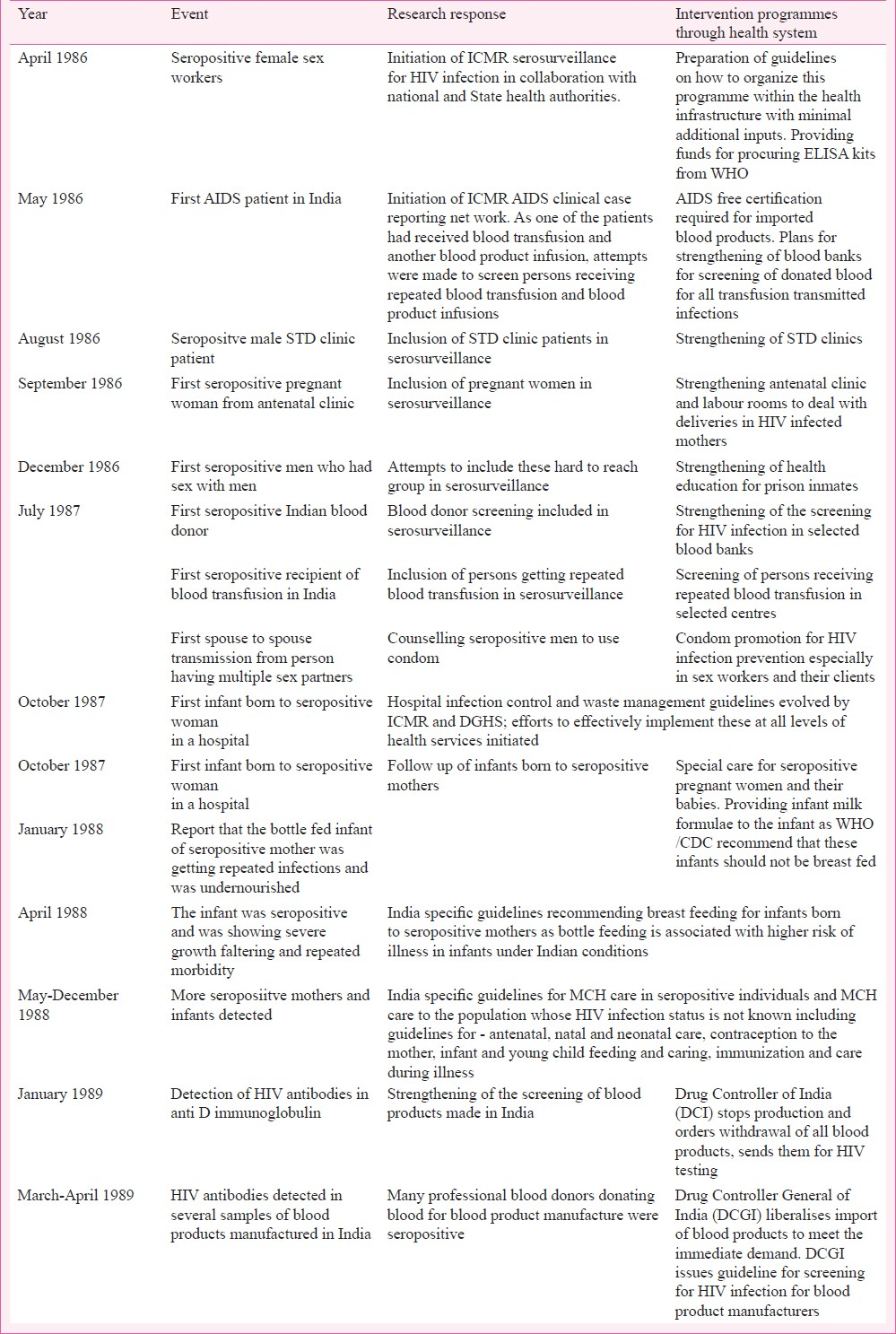
India got the unique opportunity of detecting a major public health problem very early in the course of the epidemic and facing the challenge of containing and controlling it within the existing constraints of health system in developing countries. Organisation of a National AIDS Control Programme had posed a formidable challenge to the health care system even in developed countries. Between 1986 and 1991 the National AIDS Programme was carried out as a collaborative effort of ICMR, national and State health services (Fig. 3). Because of their conviction that the opportunity to tackle HIV infection early in the course of the epidemic should not be missed due to paucity of resources, ICMR, the investigators in the surveillance centres, national and State health services coped with the additional work load by overstretching their infrastructure and human resources. The findings from sero-surveillance and the response in terms of the intervention for prevention, detection and management of HIV infection between 1986 and 19897–9 are given in the Table.

- Organisation chart of National AIDS Programme 1986-1991.
The interventions were evidence based and took into account the strengths and weaknesses of the Indian health care system. India specific prog-rammes8–1315 were drawn up for (i) prevention of blood /blood product transmission of HIV infection; the opportunity was used to strengthen and streamline safe blood banking in the country; (ii) prevention of sexual transmission; opportunity was used to re-energise STD control programmes; (iii) provision of counselling services, screening for HIV infection and follow up care for seropositive persons; (iv) provision of anti-retroviral therapy (ART) to all those who needed it; (v) strengthening of hospital infection control and waste management systems to prevent accidental infection in health care settings; and (vi) strengthening of maternal and child health (MCH) services for HIV infected mother child dyad.
India specific guidelines were drawn up9–1315 and widely disseminated for (i) care of HIV infected persons and AIDS patients; (ii) pre-and post-test counselling and follow up care for persons seeking voluntary testing; (iii) antenatal, natal and post-natal care for seropositive mothers; (iv) antenatal, natal and post-natal care for women during HIV epidemic; (v) contraceptive care for seropositive women; (vi) contraceptive care for women during HIV epidemic; (vii) infant and young child feeding in seropositive mothers; (viii) infant and young child feeding in general population during HIV epidemic; (ix) immunization of infants born to seropositive mothers; (x) immunization programme during HIV epidemic; and (xi) infection control and waste management to prevent accidental infection during health care.
All the HIV related services were provided by appropriate strengthening of existing health care system. It is noteworthy that unlike many developing countries, providing needed care for HIV infected persons and AIDS cases, did not have any adverse impact on providing appropriate health care for persons with other ailments. During the last ten years, India has steeply scaled up access to ART and has been providing generic drugs for ART at a relatively affordable cost16.
It is often stated that lack of ready access to current research findings comes in the way of early initiation of evidence based effective interventions. This factor is cited as one of the major reasons for the wide time gap between publication of research results and their application in health care delivery system. The ICMR reported the findings of ongoing studies on HIV infection every month in the ICMR Bulletin and provided a yearly comprehensive review in the Nov/Dec issue of ICMR bulletin7–13 so that all available information is widely disseminated among the research workers, health service personnel, policy makers and programme managers. As all the stakeholders had access to updated information on HIV infection, it was possible to evolve intervention programmes and guidelines as soon as a problem was identified with the co-operation and inputs from all stakeholders. This was one of the major reasons for the successful initiation of appropriate HIV related interventions prior to establishment of National AIDS Control Programme. The initial impetus and the collaboration built up in the eighties enabled a seamless transition to National AIDS Control Programme (NACP) in 1992 and continued to pay rich dividends over the next two decades. India in 2012 has succeeded in remaining as one of the countries with low prevalence of HIV infection14.
National AIDS Control Programme
Taking into account the epidemiological data provided by ICMR studies and interventions already initiated between 1986 and 1991 by the Ministry of Health, NACP I was initiated in 199217 with the following objectives:
(i) Developing capacity for hospital and community-based low cost care for people living with HIV and AIDS patients. (ii) Strengthening services for prevention and management of STD. (iii) Reducing HIV transmission among high risk group population by strengthening targeted intervention, STD control and condom promotion programmes. (iv) Reducing blood-borne transmission by screening donated blood for blood transfusion/blood product preparation. (v) Reducing mother to child transmission. (vi) Improving infection control and waste management in health care settings for reducing accidental infection. (vii) Promoting voluntary testing and counselling. (viii) Forging inter-sectoral linkages between public, private and voluntary sectors. (ix) Strengthening implementation capacity at the national, State and Panchayat level through appropriate arrangements and increasing timely access to reliable information. (x) Strengthening sentinel surveillance.
In NACP 2 and 3 there was added emphasis on prevention of mother-to-child transmission through perinatal ART; improved access to ART services and care of AIDS patients; and improved surveillance to obtain epidemiological data on time trends in HIV infection.
Current status of HIV infection in India
Global epidemiological data on HIV infection indicate that soon after the introduction of the infection in the community seropositivity rates are low. In the next phase, the infection spreads to susceptible persons in the vulnerable groups resulting in steep rise in seropositivity rates. Finally, in the third phase the seropositivity rates plateau when the number of persons who get infected is similar to the number who die of HIV infection. The steepness of the slope of the epidemic curve and the rapidity with which plateau is reached are determined by the proportion of susceptible at risk persons in the community and the effective use of prophylactic measures by the risk groups18.
Based on sentinel surveillance data on seropositivity rates reported in various groups in different States in India, it was estimated that number of HIV infected persons in India rose from 1-2 million in 1991, to 3.5 million in 1998 and 3.9 million in 2000. More than 50 per cent of infected persons were women and children. Every year, approximately 30,000 deliveries in India occur among sero-positive women and about 8,000 infants were infected with HIV17. The UN Population Division had computed the impact of HIV infection on longevity in different countries/regions. After the advent of HIV infection there had been a steep fall in longevity in Sub-Saharan Africa. In India, there has been only a small reduction in expected improvement in longevity because prevalence of HIV infection in general population is low17. India's census19 confirmed that HIV infection had no major adverse impact on expected improvement in longevity in Indian population; population projections20 have shown that the trend will be similar in the next decade.
Recognising the limitations of estimation of HIV prevalence on the basis of sentinel surveillance, Ministry of Health and Family Welfare (MoHFW), New Delhi, decided that an unlinked anonymous testing for HIV infection would be taken up as a part of the National Family Health Survey-3 (NFHS-3)21. Estimation of HIV prevalence from this database indicated that the prevalence of HIV infection was only 0.36/1000. NACO made a downward revision of the estimated number of persons living with HIV infection in India to about 2.2 million. In 2009, NACO estimated that seroprevalence in men was 0.36/1000 and in women 0.25/1000; estimated number of persons infected with HIV was 2.4 million (95% CI 1.9-3.1 million). There has been a progressive decline in prevalence of seropositivity rate from 0.36/1000 in 2006 to 0.31/1000 in 2009 and estimated new infections from 0.27 million in 2000 to 0.12 million in 200914.
Effective implementation of a multi-pronged, rational strategy for HIV infection containment and control right from the initial stages, and dedicated work done by committed professionals belonging to government and voluntary sectors, cultural ethos of the country, responsible behaviour of the population and relatively low i.v. drug use, are some of the factors which have played a crucial role in achieving rapid decline in new infection and prevalence of infection within a quarter of a century after the initial detection of HIV. At this stage, it is essential to ward off complacency and continue intensive interventions for prevention, early detection and effective management of HIV infection. If this were done perhaps India can rapidly achieve zero new cases at least with respect to mother-to-child and blood transfusion transmitted HIV infection.
Lessons learnt and the way forward
AIDS pandemic caught the world in its most complacent, post Alma Ata decade, when all seemed well on the surface and progressive improvement in health was inevitable and achievable if not by the magical 2000 AD, at least a decade later. With startling suddenness, the HIV pandemic ripped the surface veneer, exposing the global ugly realities including unhealthy lifestyles of persons infected with HIV and those at risk of HIV infection, shortcomings and prejudices of health system providing care and the entire social structure. The initial reaction was predictably panic, passionate protests and aggressive postures or depression and desperation. But soon the challenge brought forth the best in mankind - organiza-tion of a truly global systematic effort to define the magnitude and major mode of transmission of infection, to obtain natural history of the disease, and to provide rational and effective interventions for prevention, early detection and effective management of the infection and control of the epidemic.
It is noteworthy that counselling and care are being provided not only for the person but also the families of the persons with HIV infection so that their suffering can be alleviated. Never before has so much been done, for so many, by so many, in so short a time.
Twenty five years after detection of the first HIV infected person in India14, the epidemic has plateaued, and new infection rates have come down. Prevalence of HIV infection continues to be low though over 2 million Indians are infected with HIV. India appears to have risen to the challenge posed by HIV infection and remained one of the least affected counties by AIDS epidemic. However, there are numerous challenges ahead.
Three decades ago AIDS was perceived as a rapidly fatal disease in young men and women; today we know that HIV infection/AIDS is a chronic disease. Like persons with other chronic diseases, HIV infected persons have to face the challenges of adherence to long term follow up and ART. Interventions such as counselling and persuading at risk individuals to undergo screening to identify seropositive individuals, following up and counselling of seropositive persons, persuading high risk groups to change their lifestyles are being implemented through targeted intervention programmes with varying degrees of success.
In the eighties, HIV/AIDS was known to be a wasting disease and for the last three decades the major focus has been to provide food security to the HIV infected persons and their families, and to provide nutrient supplements to combat infection related nutrient depletion in HIV infected persons. In the eighties, ICMR developed India specific guidelines for infant and young child feeding practices and maternal and child health care in seropositive persons10. India also played an important role when WHO was evolving guidelines on these aspects for developing countries. These guidelines saved enormous number of children from morbidity, undernutrition and untimely death. Implementation of these will continue to be accorded high priority in India. It is ironical that both in developed and developing countries obesity, abdominal adiposity and metabolic syndrome are emerging as important problems in persons on long term ART22; there are reports of deaths due to cardiovascular diseases in HIV infected persons23. It would appear that eventually HIV infected persons will also face dual nutrition and disease burden.
India is a global manufacturing hub for antiretroviral drugs and supplies generic anti-retroviral drugs to many developing countries. Inspite of the use of generic drugs, the cost of ART continues to be high. The emergence of drug resistance to first and even second line ART is a cause of major concern. Research studies have shown that early initiation of ART prior to fall of CD4 count can successfully prolong good quality life and postpone symptomatic phase of HIV infection and progression to AIDS. Emboldened by the success of efforts to prevent mother-to-child transmission, research workers are exploring other potential areas for chemoprophylaxis. Research studies are underway to explore ART for prevention of infection among sero-discordant couples and ART in the post-exposure period for prevention of HIV infection. But these interventions may bring in their own sets of problems. What are the likely consequences of these prevention programmes in terms of side effects of drugs, compliance with therapy for decades, drug resistance, and cost of care? In the coming decade these are some of the difficult issues that will confront the research workers who have to find the answers, health planners, policy makers and health care providers who will implement rational interventions, and last but perhaps the most important the people themselves who will play a crucial role in the success of these interventions.
In the final analysis it was the human resources for health and behavioural ethos of the people that enabled India to succeed in the first round of battle against HIV. Investing adequately in human resources for health, providing needed supplies and services and taking people as partners in AIDS control programme will be crucial for combating HIV infection and its adverse health consequences in future also.
References
- A cluster of Kaposi's sarcoma and Pneumocystis carinii pneumonia among homosexual male residents of Los Angeles and Orange Counties, California. MMWR Morb Mortal Wkly Rep. 1982;31:305-7.
- [Google Scholar]
- Slim disease: a new disease in Uganda and its association with HTLV-III infection. Lancet. 1985;2:849-52.
- [Google Scholar]
- Isolation of a T-lymphotropic retrovirus from a patient at risk for acquired immune deficiency syndrome (AIDS) Science. 1983;220:868-71.
- [Google Scholar]
- AIDS: A worldwide pandemic. In: Gottlieb MS, Jeffries DF, Mildvan D, Pinching AJ, Quinn TC, Weiss RA, eds. Current topics in AIDS. Vol 2. Chichester: John Wiley & Sons; 1989.
- [Google Scholar]
- Anonymous. HIV infection – ongoing studies and future research plans. ICMR Bull. 1988;18:109-19.
- [Google Scholar]
- Anonymous. HIV infection – ongoing studies and future research plans. ICMR Bull. 1989;19:115-29.
- [Google Scholar]
- Hospital policies on care of HIV infected persons and prevention of accidental infection. ICMR Bull. 1990;20:29-35.
- [Google Scholar]
- HIV infection –ongoing studies and future research plans. ICMR Bull. 1990;20:120-9.
- [Google Scholar]
- HIV infection –ongoing studies and future research plans. ICMR Bull. 1991;21:125-44.
- [Google Scholar]
- National AIDS Control Organisation technical report. In: India HIV estimates. New Delhi: National Institute of Medical Statistics and National AIDS Control Organisation; 2010.
- [Google Scholar]
- Planning Commission, Government of India, New Delhi. Eighth, Ninth, Tenth and Eleventh Five Year Plans. National AIDS Control Programme. Available from: http://planningcommission.nic.in/plans/planrel/fiveyr/index9.html
- [Google Scholar]
- Basic epidemiology and natural history of basic epidemiology and natural history of HIV/AIDS. Available from: http://www.whoindia.org/LinkFiles/Care_and_Support_Activities_Basic_Epidemiology_and_Basic_History_of_HIV_AIDS.pdf,
- [Google Scholar]
- Registrar General & Census Commissioner, New Delhi, India. Population projections for India and states 2001-2026. Available from: http://nrhm-is.nic.in/UI/Public%20Periodic/Population_Projection_Report_2006.pdf
- [Google Scholar]
- Census India. 2011. Available from: http://censusindia.gov.in/2011-common/CensusDataSummary.htm
- [Google Scholar]
- National Family Health Survey (NFHS-3) Available from: http://mohfw.nic.in/nfhsfactsheet.htm
- [Google Scholar]
- Metabolic syndrome among HIV-infected patients: Prevalence, characteristics, and related factors. Diabetes Care. 2005;28:132-7.
- [Google Scholar]
- Coronary heart disease in HIV-infected individuals. J Acquir Immune Defic Syndr. 2003;33:506-12.
- [Google Scholar]






