Translate this page into:
HLA-G 3’UTR polymorphisms & response to a yoga-based lifestyle intervention in rheumatoid arthritis: A randomized controlled trial
For correspondence: Dr Rima Dada, Department of Anatomy, Laboratory for Molecular Reproduction & Genetics, All India Institute of Medical Sciences, New Delhi 110 029, India e-mail: rimadadaaiims20@gmail.com
-
Received: ,
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Human leucocyte antigen (HLA)-G plays a vital role in immunomodulation in rheumatoid arthritis (RA). The mounting evidence suggests a link between HLA-G gene polymorphisms, disease susceptibility and methotrexate treatment response. Various environmental factors influence the onset and progression of RA and its treatment outcomes. The aim is to identify the treatment response of HLA-G 3’ untranslated region polymorphisms to yoga-based lifestyle intervention (YBLI).
Methods:
In this eight-week single-blinded randomized controlled trial (CTRI/2017/05/008589), patients with RA (n=140) were randomized into two groups namely, yoga group or non-yoga group. Baseline genomic DNA was isolated using salting-out method. PCR-based methods were used for genotyping. The levels of soluble (s) HLA-G and disease activity were assessed by ELISA and disease activity score-28–erythrocyte sedimentation rate (DAS28-ESR), respectively, at baseline (day 0) and after eight weeks of intervention.
Results:
Low-producing sHLA-G genotypes, i.e. +3142GG and 14 bp ins/ins, showed a significant increase in sHLA-G levels after YBLI. The association analysis between HLA-G polymorphisms and treatment for RA showed no considerable differential treatment remission in either of the groups (P>0.05). The percentages of improvement were higher in the yoga group as compared to the non-yoga group in both the HLA-G +3142G>C and 14 bp ins/del polymorphisms irrespective of their respective genotypes. No significant association was found between sHLA-G levels and disease activity with respect to genotypes.
Interpretation & conclusions:
Yoga intervention results in improvement and reduced severity of RA in patients irrespective of the HLA-G 14 bp ins/del or +3142G>C polymorphisms. YBLI may be used as an adjunct therapy in RA independent of the genotypes.
Keywords
3’ UTR HLA-G polymorphism
DAS28-ESR
gene environment interaction
randomized controlled trial
rheumatoid arthritis
soluble HLA-G
Rheumatoid arthritis (RA) is the most common autoimmune arthritis1. Various genetic and environmental risk factors are involved in the pathogenesis of this disease2. Genome-wide association studies have demonstrated a strong association with the region of human leucocyte antigen (HLA), which includes the HLA-G gene (6p21.3)3. HLA-G antigens are a type of non-classical major histocompatibility complex class Ib molecules that possess tolerogenic immune properties45. Several polymorphisms of the HLA-G gene might interfere with the expression levels of this gene. The HLA-G gene 3’ untranslated region (UTR) 14 bp ins/del (rs66554220) and +3142G>C (rs1063320) polymorphisms have been shown to influence the HLA-G mRNA transcript size and stability67. There are environmental factors such as drug intervention or yoga-based lifestyle intervention (YBLI), which influence the levels of soulble (s) HLA-G. The previous study from our laboratory indicated a significant elevation in sHLA-G levels after yoga intervention, an active form of mind–body intervention (MBI)8. This Indian-origin MBI is emerging as an alternative and complementary therapy that targets the overall wellbeing, reduces the severity of depression and improves the quality of life9. Yoga targets both mind and body via a well-defined psychoneuroimmune pathway, targets multiple organ systems, improves cardiovagal tone and maintains oxidative eustress which further affects basic metabolism, organ system maintenance, epigenetics, DNA repair, oxidative bioprocesses, blood pressure, subjective well-being and quality of life8910111213.
The current evidence is lacking in the clinical utility of yoga in patients with RA who have 14 bp ins/del (rs66554220) and +3142G>C (rs1063320) polymorphisms and are less likely to respond to disease-modifying anti-rheumatic drugs (DMARDs). Hence, further studies exploring the possible modes of action underlying the therapeutic effect of yoga at a genetic level are required and to establish how regular yoga practice affects the markers of immune modulation like sHLA-G. We hypothesized that therapeutic effect of eight weeks of YBLI in patients with active RA reduces disease activity and upregulates sHLA-G levels irrespective of the presence of disease susceptibility genotypes. The current evidence is limited to establish a link between the multifaceted dimensions of yoga and how it acts on patients with RA with disease susceptibility genotypes. With this background, the primary aim of the present study was to evaluate if yoga is efficacious in cases with susceptibility genotypes, i.e. HLA-G +3142GG and HLA-G 14 bp ins/ins, and to clarify if HLA-G 14 bp ins/del and +3142 G>C polymorphisms have an impact on clinical outcome and disease severity following YBLI.
Material & Methods
Study participants: This single-blinded randomized controlled trial consisted of 140 RA patients fulfilling the 2010 American College of Rheumatology/European League Against Rheumatism 2010 criteria for RA14. RA patients greater than 18 yr of age were recruited from the outpatient clinics of Rheumatology Department, All India Institute of Medical Sciences, New Delhi, India, between June 2017 to July 2018, and assigned to receive either YBLI with conventional drug therapy (yoga group) or routine drug therapy alone (non-yoga group) for eight weeks. All patients with RA enrolled for the trial were on routine medical treatment, including DMARDs for at least six months and whose Disease Activity Score-28–Erythrocyte Sedimentation Rate (DAS28-ESR) was >2.6. Any patients with a history of recent intake of oral/intra-articular steroids in the past six months or taking any other supplements such as antioxidants, herbal–mineral supplements or undertaking any aerobic activities were excluded from the study. Furthermore, patients with any other autoimmune diseases, viral infections, cancer, pregnancy and recurrent spontaneous abortions were excluded from the study. The trial was prospectively registered on the Clinical Trials Registry of India (2017/05/008589) and the study was approved by the Institutional Review Board. All participants provided written informed consent before participating in any study procedures.
Sample size: For the outcome of RA improvement, assuming a 30 per cent therapeutic gain over drug treatment to be clinically significant, the number of participants per group required was 55, in order to achieve approximately 80 per cent power at a two-sided α level of 0.05. Assuming a 20 per cent dropout rate in each groups, so 70 patients were recruited in each group (total 140).
Randomization and blinding: Computer-based randomization using permuted blocks was done by a research assistant who was not involved in the study with the assistance of a web tool, Research Randomizer (https://www.randomizer.org/). The generated random numbers were concealed in sequentially labelled, opaque, and sealed envelopes until group allocation. Participants were not blinded to allocation; only the statistician and investigator were blinded to the group status of the participants.
Interventions: A total of 140 participants were randomized into yoga or non-yoga groups. Baseline characteristics of participants from both the groups were recorded on day 0 before the beginning of the intervention.
Yoga-based lifestyle intervention (YBLI): Participants of the yoga group underwent an eight-week pre-tested YBLI programme along with the routine medications (DMARDs) prescribed by the physicians. Each session in the YBLI included a set of asanas (physical postures), pranayama (breathing exercises) and dhyana (meditation) for approximately 120 min per day15. The sessions were held five times a week for eight weeks and were taught by a registered, specialized yoga instructor at the Laboratory for Molecular Reproduction and Genetics, Department of Anatomy, AIIMS, New Delhi.
Usual care control intervention: Patients of the non-yoga group were advised to continue with their prescribed medicines by the physicians, i.e. DMARDs and also to maintain their day-to-day activities. Further, they were instructed not to enrol themselves in any kind of exercise regime/aerobic activities for the duration of eight weeks.
Outcome measures: The primary endpoint of the trial was to measure the change in disease activity assessed by DAS28-ESR and sHLA-G levels after eight weeks of the intervention. The secondary endpoint was to analyze HLA-G 3'UTR +3142G>C (rs1063320) and 14 bp ins/del (rs66554220) polymorphisms in RA treatment with either yoga group (YBLI and drug therapy) or non-yoga group (drug therapy alone) and to analyze the clinical utility of yoga in those who have risk allele genotypes for RA, i.e. HLA-G +3142GG and 14 bp ins/ins.
Study procedure: The study participants were asked to undergo a clinical evaluation and provide a blood sample at baseline and after eight weeks. DNA was extracted from blood samples, and genotyping was completed at baseline. During the eight-week intervention period, participants were asked to follow the procedures designed for their group. Evaluation of clinical parameters and sHLA-G level detection was repeated after completion of the intervention at eight weeks.
Assessment of clinical parameters: The assessment of clinical parameters included the calculation of DAS28-ESR, which examined 28-joint counts based on tenderness and swelling. In DAS28-ESR, a rating of ≤2.6 represented remission, >2.6 to 3.2 represented low disease activity, >3.2 to 5.1 represented moderate disease activity and >5.1 represented high disease activity.
Assessment of laboratory markers: A total of 5 ml of peripheral blood samples was obtained from all randomized patients in the trial at baseline for genotyping and sHLA-G estimation. At the end of the intervention, only 1 ml of blood sample was taken to repeat the sHLA-G level estimation.
Genotyping: Polymerase chain reaction (PCR)–restriction fragment length polymorphism (RFLP) analysis was done to genotype HLA-G +3142G>C (rs1063320) in the peripheral blood DNA of patients with RA. An HLA-G +3142G>C PCR amplicon of 406 base pair (bp) was subjected to BaeGI (New England Biolabs Inc., Ipswich, MA, USA) restriction enzyme digestion as per the manufacturer’s protocol. The G (wild type) allele was digested by the enzyme resulting in 316 and 90 bp products, whereas the C (mutant type) allele remained undigested (406 bp).
Genotyping of HLA-G 14 bp ins/del (rs66554220) variant in peripheral blood DNA of study subjects was done by PCR. The PCR product sizes were 127 bp for del (wild type) and 141 bp for ins (mutant type) allele.
Estimation of sHLA-G levels: The sHLA-G levels were determined using enzyme-linked immunosorbent assay (ELISA) according to the manufacturer’s protocol (Bioassay Technology Laboratory, USA).
Statistical analysis: The statistical analyses were performed using IBM SPSS Statistics for Macintosh, Version 25.0. (IBM Corp. Armonk, NY, USA). P<0.05 was considered statistically significant. Chi-square test and Fisher’s exact tests were used to compare categorical variables at a baseline level, whereas the Student’s t test and Wilcoxon rank-sum test were used to compare normally distributed continuous variables and non-parametric continuous data, respectively (Table I). For intra-group analysis, paired t tests or Wilcoxon signed-rank tests were used to see the pre- and post-difference for parametric or non-parametric data, respectively. For inter-group analysis, the difference over an eight-week time was made using independent samples t test. Multiple regression analysis was used to determine the variable change associated with a change in DAS28-ESR and change in sHLA-G levels after eight weeks of intervention.
| Variables | Group | χ2 | t | P | |
|---|---|---|---|---|---|
| Yoga (n=70) | Non-yoga (n=70) | ||||
| Demographic characteristics | |||||
| Age (yr) | 44.63±11.9 | 47.01±12.0 | - | 1.180 | 0.2400 |
| Sex* | |||||
| Male | 8 | 14 | 1.941 | - | 0.1635 |
| Female | 62 | 56 | |||
| Age at onset (yr) | 38.53±11.7 | 40.9±11.5 | - | 1.210 | 0.2284 |
| Disease duration (yr) | 6.09±4.2 | 6.1±3.1 | - | 0.015 | 0.9880 |
| Number of patients RF, positive* | 68 | 67 | - | - | - |
| BMI (kg/m2) | 23.60±5.2 | 24.14±3.1 | 0.7632 | 0.4467 | |
| Kuppuswamy’s socioeconomic status scale* | |||||
| Upper | 11 | 14 | 4.178 | 0.3824 | |
| Upper middle | 30 | 37 | |||
| Lower middle | 13 | 7 | |||
| Upper lower | 14 | 9 | |||
| Lower | 2 | 3 | |||
| Presenting symptoms | |||||
| Early morning stiffness (min) | 25.35±23.2 | 26.71±22.4 | - | 0.3518 | 0.7255 |
| TJC | 5.95±4.5 | 6.67±4.01 | - | 0.9912 | 0.3233 |
| SJC | 3.95±4.2 | 3.92±2.6 | - | 0.0480 | 0.9617 |
| Drug therapy | |||||
| Number of patients on MTX monotherapy | 70 | 70 | 1.109 | - | 0.2923 |
| Number of patients on MTX plus other DMARDs | 26 | 18 | |||
| Number of patients on biologic response modifiers | 0 | 0 | |||
| Disease severity | |||||
| Mean DAS28-ESR | 4.68±0.9 | 4.58±1.1 | - | 0.5420 | 0.5887 |
| Stratification by disease severity | |||||
| >2.6-3.2 (low) | 2 | 5 | 1.354 | 0.5081 | |
| >3.2-5.1 (moderate) | 42 | 40 | |||
| >5.1 (high) | 26 | 25 | |||
Data are described as frequency (%) for sex and mean±SD for others; χ2, Chi-square value; t, t test value; TJC, tender joint count; SJC, swollen joint count; MTX, methotrexate; DMARDs, disease-modifying anti-rheumatic drugs; DAS28-ESR, Disease Activity Score-28–Erythrocyte Sedimentation Rate; SD, standard deviation; BMI, body mass index
Results
A total of 140 patients with RA were randomized into the yoga group (n=70) and non-yoga group (n=70) (Fig. 1). The baseline characteristics of the participants in each group are shown in Table I. The group-wise genotype and allele frequency of HLA-G +3142G>C and 14 bp ins/del were found to be non-significant between yoga (n=70) and non-yoga groups (n=70) (Table II).
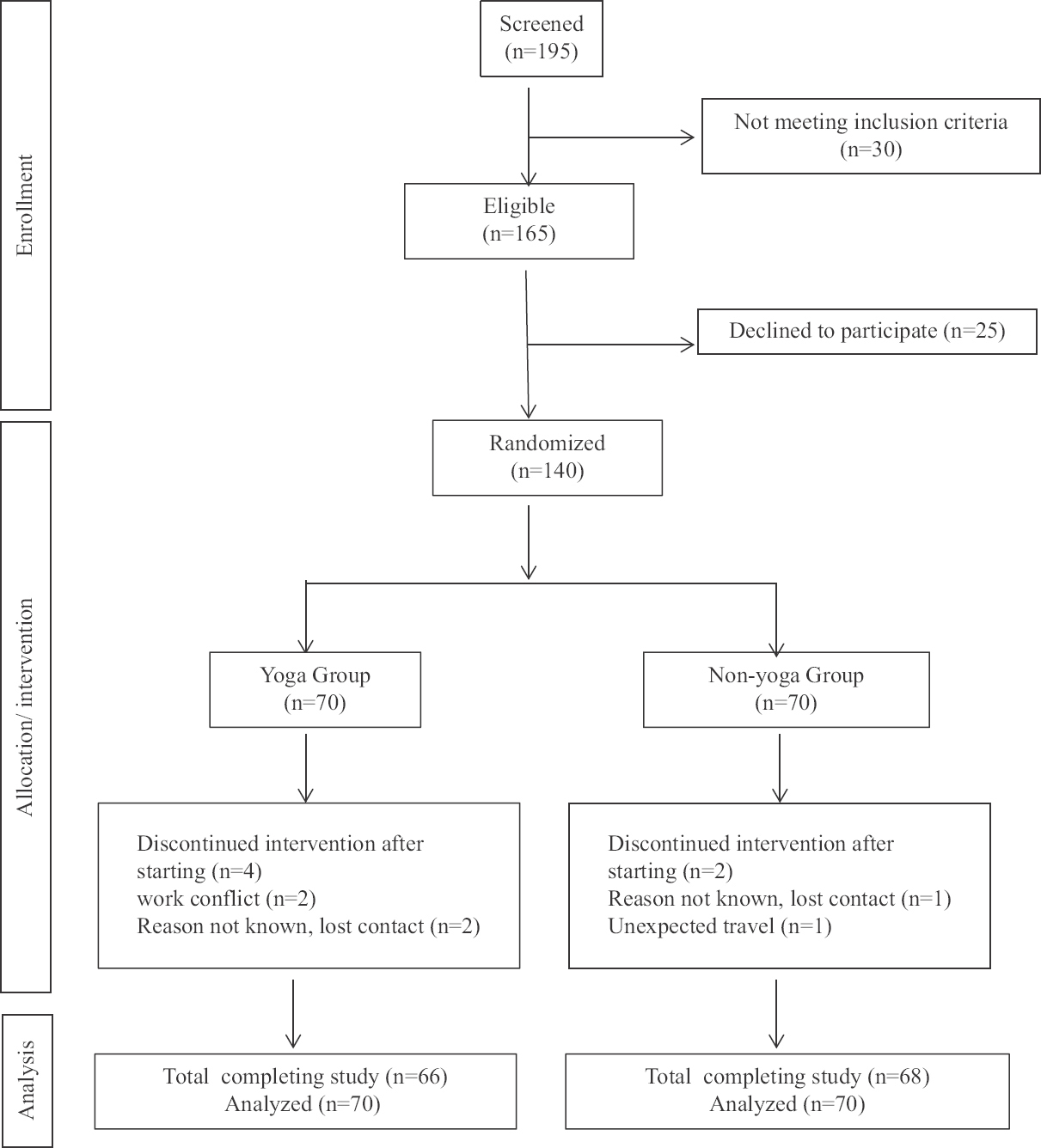
- A CONSORT flow chart.
| HLA-G polymorphism | Yoga group (n=70) | Non-yoga group (n=70) | P |
|---|---|---|---|
| +3142G>C (rs1063320) | |||
| Genotype, n (%) | |||
| GG | 29 (41.4) | 37 (52.9) | 0.3328 |
| GC | 30 (42.9) | 22 (31.4) | |
| CC | 11 (15.7) | 11 (15.7) | |
| Allele frequency, n (%) | |||
| G | 62.9 | 68.6 | 0.4544 |
| C | 37.1 | 31.4 | |
| 14 bp ins/del (rs66554220) | |||
| Genotype, n (%) | |||
| del/del | 36 (51.4) | 26 (37.1) | 0.1198 |
| ins/del | 14 (20) | 24 (34.3) | |
| ins/ins | 20 (28.6) | 20 (28.6) | |
| Allele frequency, n (%) | |||
| del | 61.4 | 54.3 | 0.3876 |
| ins | 38.6 | 45.7 | |
HLA-G, human leucocyte antigen-G; RA, rheumatoid arthritis
Treatment efficacy: Interaction between disease severity, genotypes and sHLA-G levels: The changes in DAS28-ESR scores and sHLA-G levels from baseline to eight weeks based on disease activity and polymorphism stratifications are summarized in Tables III and IV. Analysis of the association of HLA-G +3142G>C (P=0.3564) and 14 bp ins/del (P=0.6154) polymorphisms and treatments for RA showed no significant differential treatment remission in the yoga group and non-yoga group. The percentage improvement was greater in the yoga group as compared to the non-yoga group in both the HLA-G +3142G>C and 14 bp ins/del polymorphisms irrespective of their genotypes (Fig. 2).
| Group | Baseline measurement, mean±SD | Post eight-week measurement, mean±SD |
P Within groups |
Change from baseline to eight weeks, mean (95% CI) |
P Between the groups |
|---|---|---|---|---|---|
| Total for all participants in a group – DAS28-ESR | |||||
| Yoga | 4.7±0.9 | 4.1±0.9 | <0.001 | 0.5 (0.4-0.7) | <0.001 |
| Non-yoga | 4.6±1.1 | 4.5±1.3 | 0.720 | 0.1 (−0.1-0.3) | |
| Stratified based on severity – DAS28-ESR | |||||
| Low | |||||
| Yoga | 2.8±0.04 | 3.8±0.5 | 0.228 | −0.9 (−5.6-3.6) | 0.042 |
| Non-yoga | 2.6±0.02 | 4.2±1.3 | 0.041 | −1.7 (−3.3-−0.1) | |
| Moderate | |||||
| Yoga | 4.1±0.5 | 4.1±1.0 | 0.975 | −0.005 (−0.3-0.3) | 0.324 |
| Non-yoga | 4.1±1.1 | 4.3±1.4 | 0.264 | −0.3 (−0.8-0.2) | |
| High | |||||
| Yoga | 5.6±0.6 | 4.1±0.9 | <0.001 | 1.5 (1.1-1.9) | <0.001 |
| Non-yoga | 5.7±0.5 | 4.7±1.1 | <0.001 | 1.0 (0.5-1.5) | |
| Stratified based on+3142 G>C genotypes – DAS28-ESR | |||||
| GG | |||||
| Yoga | 4.5±1.0 | 4.0±1.1 | 0.149 | 0.4 (−0.2-1.1) | 0.025 |
| Non-yoga | 4.7±1.1 | 4.3±1.2 | 0.087 | 0.4 (−0.1-0.8) | |
| GC | |||||
| Yoga | 4.9±0.9 | 4.1±0.8 | <0.001 | 0.7 (0.3-1.1) | 0.008 |
| Non-yoga | 4.3±1.2 | 4.7±1.5 | 0.337 | −0.4 (−1.2-0.5) | |
| CC | |||||
| Yoga | 4.6±0.9 | 4.4±0.7 | 0.569 | 0.2 (−0.5-0.9) | 0.414 |
| Non-yoga | 4.6±0.9 | 4.7±1.2 | 0.837 | −0.1 (−1.3-1.1) | |
| Stratified based on 14 bp ins/del genotypes – DAS28-ESR | |||||
| del/del | |||||
| Yoga | 4.8±0.8 | 4.1±1.1 | 0.002 | 0.5 (0.2-0.9) | 0.038 |
| Non-yoga | 4.7±0.8 | 4.6±1.2 | 0.713 | 0.1 (−0.4-0.7) | |
| ins/del | |||||
| Yoga | 4.5±1.0 | 4.0±1.0 | 0.126 | 0.5 (−0.1-1.3) | 0.993 |
| Non-yoga | 4.2±1.2 | 4.7±1.4 | 0.166 | −0.5 (−1.4-0.2) | |
| ins/ins | |||||
| Yoga | 4.6±1.2 | 4.2±0.8 | 0.266 | 0.4 (−0.3-1.2) | 0.014 |
| Non-yoga | 4.8±1.1 | 4.0±1.1 | 0.012 | 0.8 (0.2-1.4) | |
DAS28-ESR, Disease Activity Score-28–Erythrocyte Sedimentation Rate; CI, confidence interval; SD, standard deviation
| Group | Baseline measurement, mean±SD | Post eight-week measurement, mean±SD |
P Within groups |
Change from baseline to eight weeks, mean (95% CI) |
P Between the groups |
|---|---|---|---|---|---|
| Total for all participants in a group – soluble HLA-G (U/ml) | |||||
| Yoga | 7.9±4.1 | 9.1±5.2 | <0.001 | −1.2 (−1.8-−0.5) | 0.018 |
| Non-yoga | 8.3±3.2 | 8.5±3.5 | 0.364 | −0.2 (−0.7-0.3) | |
| Stratified based on disease severity – soluble HLA-G (U/ml) | |||||
| Low | |||||
| Yoga | 8.7±1.5 | 10.4±4.5 | 0.559 | −1.7 (−28.2-24.7) | 0.250 |
| Non-yoga | 7.5±1.4 | 7.7±1.5 | 0.748 | −0.2 (−1.8-1.4) | |
| Moderate | |||||
| Yoga | 7.9±4.5 | 8.9±5.5 | 0.007 | −1.1 (−1.8-−0.3) | 0.003 |
| Non-yoga | 7.9±3.2 | 8.3±3.8 | 0.189 | −0.4 (−1.0-0.2) | |
| High | |||||
| Yoga | 7.8±3.5 | 9.1±4.7 | 0.033 | −1.2 (−2.3-−0.1) | 0.112 |
| Non-yoga | 9.1±3.5 | 8.9±3.2 | 0.777 | 0.1 (−0.7-0.9) | |
| Stratified based on+3142 G>C genotypes – soluble HLA-G (U/ml) | |||||
| GG | |||||
| Yoga | 6.6±4 | 8.4±5.3 | 0.003 | −1.7 (−2.9-−0.6) | 0.025 |
| Non-yoga | 8.2±3.4 | 7.7±3.4 | 0.130 | 0.4 (−0.1-0.9) | |
| GC | |||||
| Yoga | 9.2±4 | 10.1±5.2 | 0.060 | −0.8 (−1.7-0.04) | 0.044 |
| Non-yoga | 8.4±3.3 | 8.9±3.7 | 0.309 | −0.4 (−1.4-0.4) | |
| CC | |||||
| Yoga | 7.6±3.8 | 8.0±4.3 | 0.380 | −0.3 (−1.2-0.5) | 0.002 |
| Non-Yoga | 8.7±2.2 | 10.6±2.4 | 0.004 | −1.8 (−3.0-−0.7) | |
| Stratified based on 14 bp ins/del genotypes – soluble HLA-G (U/ml) | |||||
| del/del | |||||
| Yoga | 8.5±3.6 | 9.1±4.2 | 0.115 | −0.5 (−2.2-−0.7) | <0.001 |
| Non-yoga | 8.1±2.8 | 9.6±3.6 | 0.001 | −1.5 (−2.3-−0.7) | |
| ins/del | |||||
| Yoga | 8.4±5.2 | 9.1±6.6 | 0.357 | −0.7 (−2.3-0.8) | 0.769 |
| Non-yoga | 9.0±3.3 | 8.1±2.9 | 0.003 | 0.9 (0.3-1.4) | |
| ins/ins | |||||
| Yoga | 6.4±3.8 | 9.0±5.7 | 0.001 | −2.6 (−4-−1.2) | 0.004 |
| Non-yoga | 7.7±3.6 | 7.6±3.8 | 0.783 | 0.1 (−0.7-1.02) | |
CI, confidence interval; SD, standard deviation; HLA-G, human leucocyte antigen-G
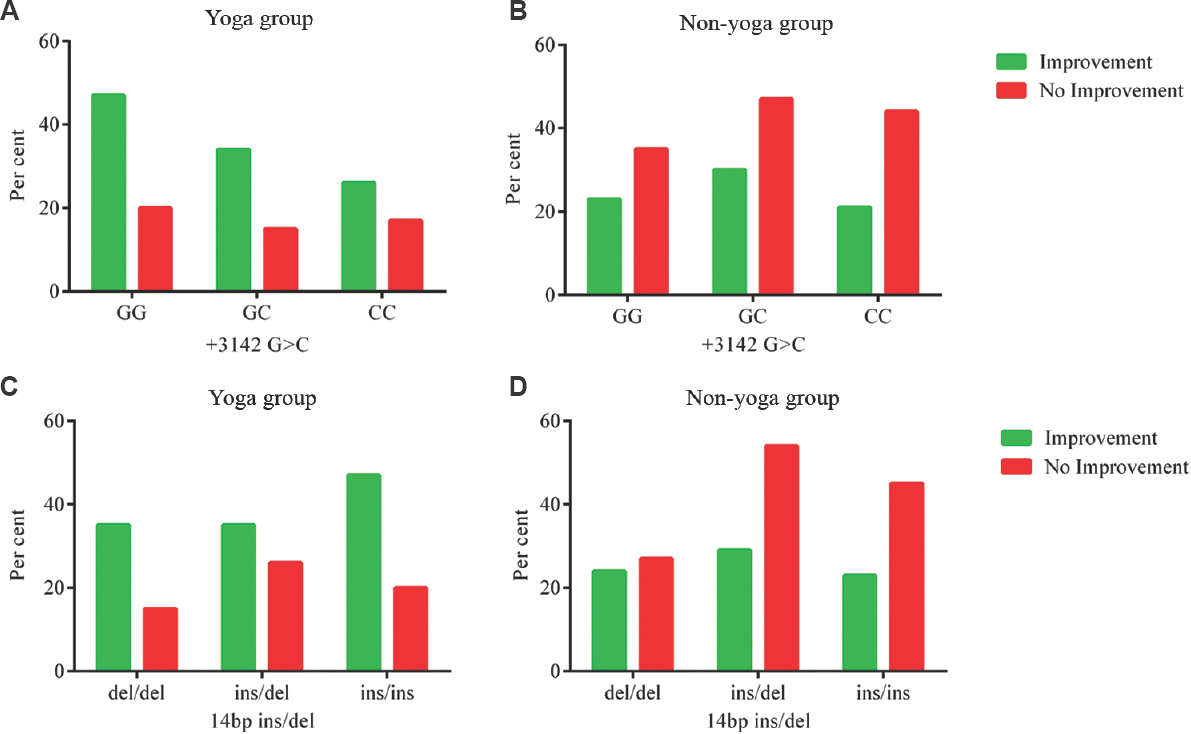
- Improvement by genotype: (A and B) Percentage improvement by HLA-G +3142G>C genotypes and treatment arm; (C and D) percentage improvement by HLA-G 14 bp ins/del genotypes and intervention group.
Association of sHLA-G levels and disease severity based on genotypes: The results of the linear regression model were derived using pre- and post-intervention change (Δ) DAS28-ESR as a dependent variable and ΔsHLA-G level as a predictor. The variance amongst the regression lines of three genotypes of HLA-G +3142G>C and 14 bp ins/del polymorphism with respect to ΔDAS28-ESR and ΔsHLA-G levels is shown in Fig. 3A-D.
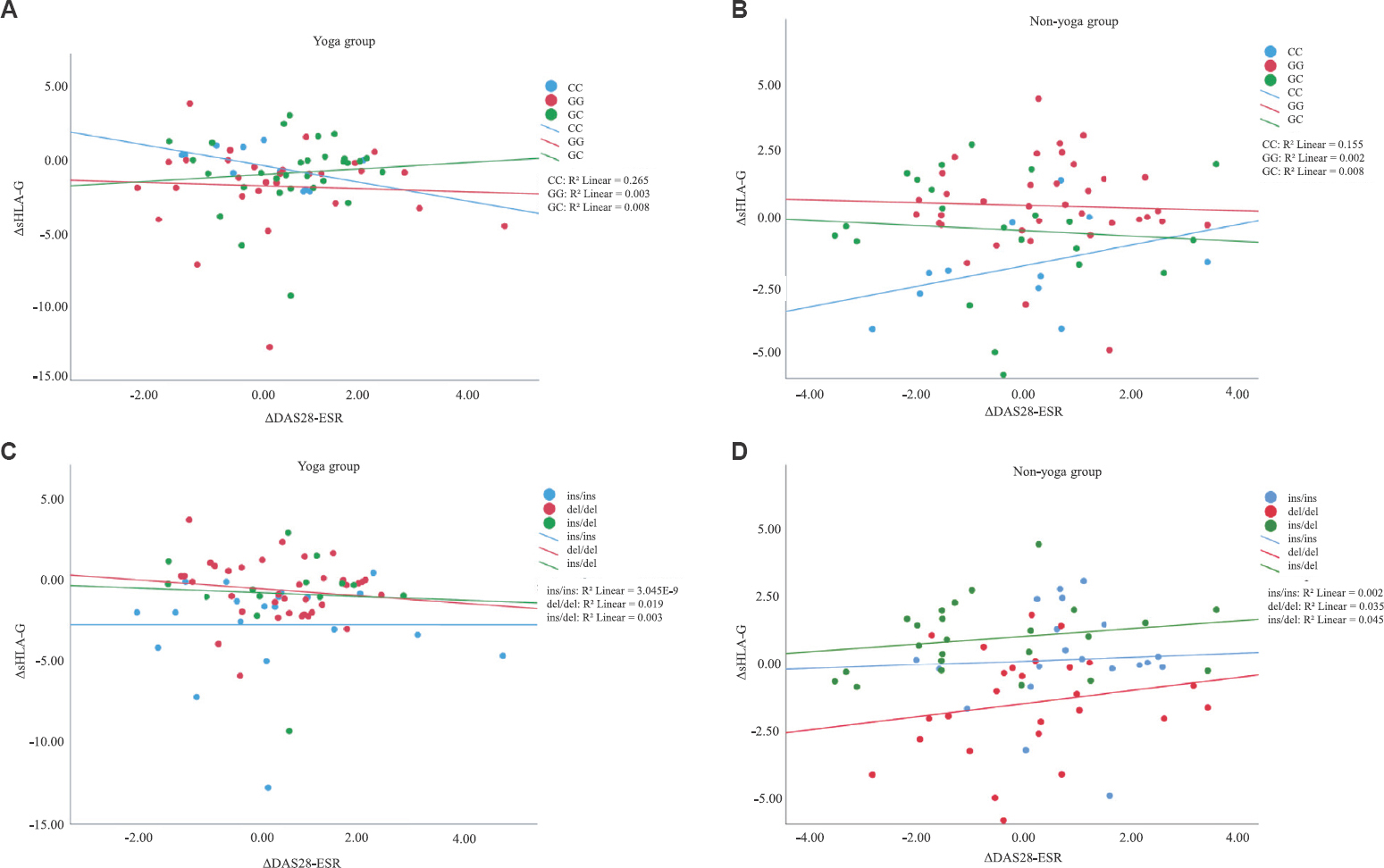
- Association of change in disease activity scores (ΔDAS28-ESR) and sHLA-G levels based on genotypes: (A and B) Association of change in disease activity scores (ΔDAS28-ESR) and disease severity from baseline by HLA-G +3142G>C genotypes in both intervention groups; (C and D) association of change in disease activity scores (ΔDAS28-ESR) and disease severity from baseline by HLA-G 14 bp ins/del genotypes in both intervention groups.
Discussion
In this study, HLA-G 14 bp ins/del and HLA-G+3142G>C polymorphisms showed no significant association on therapy response to eight weeks of YBLI in RA. To the best of our knowledge, this is the first study aiming to investigate the influence of these polymorphisms in response to YBLI in RA and if yoga is efficacious in patients with RA with susceptibility genotypes.
In 14 bp ins/del HLA-G polymorphism, the homozygous deletion of 14 bp confers a more stable mRNA as compared to the homozygous insertion genotype16. The ins allele is associated with lower levels of membrane-bound and sHLA-G levels17. In +3142 G>C HLA-G polymorphism, the +3142G allele possesses a binding site with a higher affinity for miR-148a, miR-148b and miR-152 which downregulate the expression of HLA-G1617. Various studies have investigated the impact of +3142G>C and 14 bp ins/del polymorphism of HLA-G with susceptibility to RA in various populations16171819. It is also reported that patients with RA have lower soluble (s) HLA-G levels as compared to healthy controls, which may lead to a chronic activation of inflammatory cells and contribute to increased severity of RA20. In the present study, low-producing sHLA-G susceptibility genotypes, i.e. +3142GG and 14 bp ins/ins, showed a significant increase in sHLA-G levels after YBLI. High-producing sHLA-G-protective genotypes, i.e. +3142CC and 14 bp del/del, showed a significant increase of sHLA-G levels in the non-yoga group. The percentage of improvement was higher in the yoga group as compared to the non-yoga group in both the HLA-G +3142G>C and 14 bp ins/del polymorphisms irrespective of their genotypes.
The previous studies from our laboratory investigated the impact of yoga intervention on systemic inflammatory markers; mitochondrial integrity and biogenesis; levels of critical molecules such as nicotinamide adenine dinucleotide (NAD+), sirtuins and melatonin and severity of comorbid depression in patients with RA, and it was found that after eight weeks of yoga therapy, there was a significant elevation of sHLA-G levels and reduction in DAS28-ESR levels891521. The observations from the present study suggested that there was a significant elevation of sHLA-G levels in +3142GG and 14 bp ins/ins genotypes after YBLI (Table IV). Previous studies have suggested that 14 bp ins/ins and +3142GG genotypes are associated with a lower HLA-G level than 14 bp del/ins, 14 bp del/del, and +3142GC, +3142CC genotypes, respectively616. This association of low-producing 14 bp ins and +3142G alleles with sHLA-G levels can be attributed to mRNA instability, resulting in reduced production of its protein, and thus, the elevation of sHLA-G in these two genotypes. This is of clinical significance as it is directly associated with increased disease severity. Furthermore, the 14 bp del allele confers a more stable mRNA as compared to 14 bp ins allele and is associated with a higher sHLA-G levels16.
In the present study, +3142GC and 14 bp del/del genotypes showed a significant decline in DAS28-ESR after eight weeks of YBLI. In contrast, the 14 bp ins/ins showed a significant decline in DAS28-ESR in the non-yoga group (Table III). Yoga reportedly acts via the psycho-neuro-immune axis, which creates a homeostatic balance between sympathetic and parasympathetic limbs of the autonomic nervous system during the aggressive symptomatic phase and helps normalize the flare and achieve remission inturn by achieving parasympathetic dominance22. Yoga helps improve the overall quality of life by reducing pain perception, disability quotient and disease activity in cases with active RA, which is seen by a significant reduction in the Visual Analogue Scale, Health Assessment Questionnaire–Disability Index and DAS28-ESR scores, respectively8. Yoga is a cost-effective mind–body therapy, which, unlike drugs, has no side effects and aids in prolonging the periods of remissions with fewer relapses. Yoga has tremendous transformative power and causes dynamic changes in gene expression, and promotes health. It can prevent the onset of complex lifestyle diseases, has rehabilitative potential and can be used as an adjunct therapy in the management of complex lifestyle diseases.
Methotrexate, a DMARD, is the most commonly used drug for the management of RA. Various studies have documented the association of methotrexate treatment response with HLA-G polymorphisms2324. Rizzo et al, 2006, documented that methotrexate leads to increased production of the anti-inflammatory sHLA-G molecules, which were significantly associated with 14 bp del/del genotype23. In the present study, the levels of sHLA-G showed a significant elevation in the non-yoga group in +3142CC and 14 bp del/del genotypes who were only on routine DMARDs without yoga intervention. The genotypes +3142CC and 14 bp del/del were associated with high levels of sHLA-G. Baricordi et al24 reported an association between HLA-G 14 bp ins/del polymorphism and clinical response to methotrexate treatment in RA, and the majority of patients who responded to methotrexate belonged to HLA-G 14 bp ins/ins genotype. A meta-analysis by Lee et al18 did not show any significant association between methotrexate response, HLA-G 14 bp ins/del and +3142G/C polymorphism and disease risk.
The present study demonstrated that the percentage of improvement was higher in the yoga group as compared to the non-yoga group in both the HLA-G +3142G>C and 14 bp ins/del polymorphisms irrespective of their genotypes (Fig. 2). Yoga regulates the deranged molecular networks in RA, and its mechanism could act via various pathways such as reduction of reactive oxygen species, improvement in mitochondrial integrity, upregulation of mitochondrial copy number, increase in mitochondrial membrane potential, increase in NAD+ levels which helps in maintaining the calcium signalling, nuclear and mitochondrial crosstalk, cytochrome c oxidase-II activity, harmonization of circadian rhythm markers, reduction of adhesion molecules, alteration of cytokine profiles, epigenetic modifications, etc.89152125. Yoga overall increases muscular strength, range of motion, flexibility and improves balance and co-ordination89. It reduces anxiety, depression, chronic pain and promotes wellness, hence improves the quality of life8925262728. No significant association was found between change in the sHLA-G levels and disease activity post-intervention based on genotypes in either of the groups (Fig. 3). Our findings suggest that RA improvement and response with yoga is independent of HLA-G +3142G>C and 14 bp ins/del genotype.
The main limitation in the present study was the sample size. Also, there was a lack of an active control group as the non-yoga group was not exposed to any equal attention control intervention and was only on drug therapy as compared to the active yoga intervention group. Furthermore, since there was no follow up period after eight weeks, it was difficult to predict how quickly participants returned to baseline levels of sHLA-G levels and DAS28-ESR. Hence, in future, long-term follow up studies should be carried out to study the effects of yoga on the disease parameters.
In conclusion, yoga intervention results in an improvement in RA health outcomes irrespective of the presence of HLA-G 14 bp ins/del or +3142G>C polymorphisms. YBLI may be used as an adjunct therapy for this chronic debilitating autoimmune inflammatory arthritis independent of the genotype by reducing disease activity and upregulation of levels of sHLA-G. RA, a highly heterogeneous condition, is likely to yield the most optimal outcomes through customized treatment approaches based on patient-specific genetic and environmental features. Hence, there is a need for identifying other genes that may modulate the treatment response in RA, including the beneficial outcome to YBLI.
Acknowledgment:
The authors acknowledge the yoga instructor, Ms Shalini Jha, Central Council for Research in Yoga and Naturopathy, Ministry of AYUSH, New Delhi, for providing the yoga instructions and the patients with RA for participating in the yoga programme.
Financial support & sponsorship: This study received financial support from the Department of Science and Technology, India, (SR/SATYAM/55/2016). The first author (SG) received Senior Research Fellowship (45/2/2019-ANA/BMS) from the Indian Council of Medical Research, New Delhi, India.
Conflicts of Interest: None.
References
- Rheumatoid arthritis:Pathological mechanisms and modern pharmacologic therapies. Bone Res. 2018;6:15.
- [Google Scholar]
- The genetics of rheumatoid arthritis:Risk and protection in different stages of the evolution of RA. Rheumatology (Oxford). 2016;55:199-209.
- [Google Scholar]
- Contribution of a non-classical HLA gene, HLA-DOA, to the risk of rheumatoid arthritis. Am J Hum Genet. 2016;99:366-74.
- [Google Scholar]
- Association of HLA-A and non-classical HLA class I alleles. PLoS One. 2016;11:e0163570.
- [Google Scholar]
- HLA-G +3142 polymorphism as a susceptibility marker in two rheumatoid arthritis populations in Brazil. Tissue Antigens. 2014;83:260-6.
- [Google Scholar]
- Human leukocyte antigen-G polymorphism influences the age of onset and autoantibody status in rheumatoid arthritis. Tissue Antigens. 2015;85:182-9.
- [Google Scholar]
- Impact of yoga based mind-body intervention on systemic inflammatory markers and co-morbid depression in active Rheumatoid arthritis patients:A randomized controlled trial. Restor Neurol Neurosci. 2019;37:41-59.
- [Google Scholar]
- Yoga and its impact on chronic inflammatory autoimmune arthritis. Front Biosci (Elite Ed). 2021;13:77-116.
- [Google Scholar]
- Erratum to “impact of yoga and meditation on cellular aging in apparently healthy individuals:A prospective, open-label single-arm exploratory study”. Oxid Med Cell Longev. 2017;2017:2784153.
- [Google Scholar]
- Yoga- and meditation-based lifestyle intervention increases neuroplasticity and reduces severity of major depressive disorder:A randomized controlled trial. Restor Neurol Neurosci. 2018;36:423-42.
- [Google Scholar]
- Relaxation response induces temporal transcriptome changes in energy metabolism, insulin secretion and inflammatory pathways. PLoS One. 2013;8:e62817.
- [Google Scholar]
- Mind-body medicine and immune system outcomes:A systematic review. Open Complement Med J. 2009;1:25-34.
- [Google Scholar]
- The 2010 American College of Rheumatology/European League Against Rheumatism classification criteria for rheumatoid arthritis:methodological report phase I. Ann Rheum Dis. 2010;69:1589-95.
- [Google Scholar]
- Effect of an 8-week yoga-based lifestyle intervention on psycho-neuro-immune axis, disease activity, and perceived quality of life in rheumatoid arthritis patients:A randomized controlled trial. Front Psychol. 20202259;11
- [Google Scholar]
- Evaluation of HLA-G 14bp Ins/Del and +|y3142G>C polymorphism with susceptibility and early disease activity in rheumatoid arthritis. Adv Med. 2016;2016:4985745.
- [Google Scholar]
- The 14 bp deletion-insertion polymorphism in the 3'UT region of the HLA-G gene influences HLA-G mRNA stability. Hum Immunol. 2003;64:1005-10.
- [Google Scholar]
- Meta-analysis of associations between functional HLA-G polymorphisms and susceptibility to systemic lupus erythematosus and rheumatoid arthritis. Rheumatol Int. 2015;35:953-61.
- [Google Scholar]
- Association of HLA-G 3'UTR polymorphisms with soluble HLA-G levels and disease activity in patients with rheumatoid arthritis:A case-control study. Immunol Invest. 2020;49:88-105.
- [Google Scholar]
- Linkage disequilibrium between human leukocyte antigen (HLA) class II and HLA-G--possible implications for human reproduction and autoimmune disease. Hum Immunol. 2005;66:688-99.
- [Google Scholar]
- Yoga improves mitochondrial health and reduces severity of autoimmune inflammatory arthritis:A randomized controlled trial. Mitochondrion. 2021;58:147-59.
- [Google Scholar]
- HLA-G 14-bp polymorphism regulates the methotrexate response in rheumatoid arthritis. Pharmacogenet Genomics. 2006;16:615-23.
- [Google Scholar]
- In rheumatoid arthritis, a polymorphism in the HLA-G gene concurs in the clinical response to methotrexate treatment. Ann Rheum Dis. 2007;66:1125-6.
- [Google Scholar]
- Yoga-Impact on mitochondrial health:Clinical consequences. Ann Neurosci. 2021;28:114-6.
- [Google Scholar]
- Is yoga a suitable treatment for rheumatoid arthritis:Current opinion. Open Access J Sports Med. 2012;3:81-7.
- [Google Scholar]
- Effect of mindfulness meditation on intraocular pressure and trabecular meshwork gene expression:A randomized controlled trial. Am J Ophthalmol. 2021;223:308-21.
- [Google Scholar]
- Potential role of yoga intervention in the management of chronic non-malignant pain. Evid Based Complement Alternat Med. 2022;2022:5448671.
- [Google Scholar]






