Translate this page into:
Free iron status & insulin resistance in type 2 diabetes mellitus: Analyzing the probable role of a peanut protein
*For correspondence: kamalchem.roy@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution NonCommercial ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
South Asian population is known to have an increased predisposition to type 2 diabetes mellitus (T2DM), which turns out to be an important health concern in this Region1. As per an earlier report about 11.7 per cent people of Kolkata, West Bengal, suffered from T2DM and the prevalence was on a rise2. Anaemia is also present in the Region as a significant public health problem, having a prevalence of greater than 40 per cent in South Asia3. However, the actual status of iron remains unclear because of extensive prevalence of haemoglobinopathies, possible genetic mutations contributing to iron overload, indiscriminate over-the-counter use of iron pills and traditional formulations containing undefined concentrations of iron. Higher heme iron intake and increased body iron stores were found to be significantly associated with a greater risk of T2DM45. Patients suffering from haemoglobinopathies or undergoing repeated blood transfusions also suffer from secondary iron loading disorder6.
Insulin influences the iron uptake and storage in cells by increasing the cell surface transferrin receptors7. Whether a patient with diabetes has excess iron due to increased insulin resistance still remains an unanswered question. Insulin resistance has been shown to have an association with chronic kidney diseases89. Iron accumulation has been reported in the proximal renal tubules in diabetic nephropathy10. Iron in its free form1112 i.e. in non-transferrin bound form is known to induce oxidation of biomolecules and in the formation of reactive oxygen species. We, therefore, studied the free iron status in patients with T2DM and compared with healthy individuals and to find a suitable biocompatible reagent which can bind the free iron.
A cross-sectional, pilot study was conducted on consecutive patients attending the General Medicine outpatients department of M.R. Bangur Hospital, Kolkata, India, between August 2012 and February 2014. Fasting blood and urine samples (10 ml each) were collected from 111 patients with T2DM (53.7 ± 12.4 yr, M:F 60: 51) and 30 healthy controls (75.6 ± 2.5 yr, M:F 8:7). Approval of ethical committee of Institute of Post Graduate Medical Education & Research (IPGMER), Kolkata, was obtained prior to the study.
Those (i) having anaemia, (ii) suffering from any form of haemoglobinopathy, (iii) who were on iron therapy within one year, (iv) having non-diabetic kidney disease, (v) having febrile illness, (vi) having benign prostatic hypertrophy or prostatic cancer, (vii) having urinary tract infection, or (viii) with uncontrolled hypertension, were excluded. The total iron analysis was done by Ferrozine method13 and free iron by HPLC14. Fasting plasma glucose was estimated by glucose oxidase-peroxidase (GOD-POD) method15, serum insulin by ELISA monobind kit and creatinine analysis was done by a kinetic assay15 of Jaffe's involving alkaline solution of sodium picrate16. The plasma creatinine clearance or estimated glomerular filtration rate (eGFR) were estimated as per Cockroft and Gault formulae in ml/min17. Insulin resistance was calculated by homeostatic model assessment - insulin resistance (HOMA-IR) formula18. Urinary microalbumin analysis was done by immunoturbidimetry19.
Conarachin I was extracted from peanut and purified20, and was used as a complexing agent for free iron. Conarachin I was characterized by molecular weight determination and absorption spectrometry20. A 15 per cent resolving sodium dodecyl sulphate polyacrylamide gel electrophoresis (SDS-PAGE) gel was used for molecular weight determination and confirmation of protein purification from crude peanut protein20. Presence of band at about 18 kD (Figure, lane 1) showed the presence of conarachin I in the purified protein fraction as shown earlier19. Conarachin I (0.1 ml) was mixed with 0.4 ml of the diluted serum, injected to HPLC column and analyzed to compare the amount of free Fe2+ and Fe3+ of the same serum samples20.
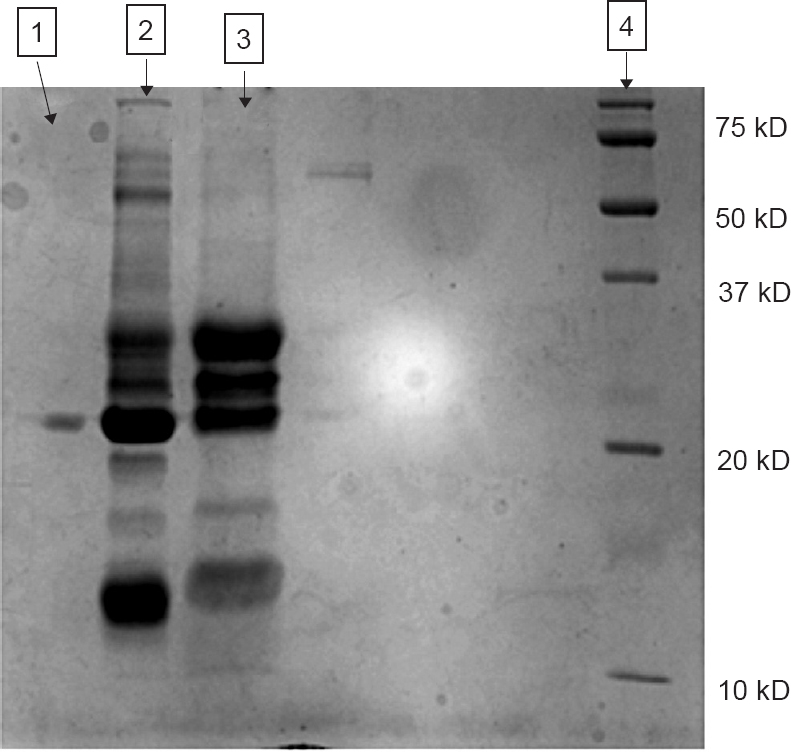
- Purified conarachin I fraction along with its precursors subjected to sodium dodecyl sulphate - polyacrylamide gel electrophoresis (SDS-PAGE). Lane 1, pure conarachin 1; Lanes 2 and 3, protein part before purification; Lane 4, mol.wt.marker.
Qualitative data were grouped and compared by chi square test. Yates correction was done when the cell frequency was below five21. Quantitative data were subjected to comparison by their differences in mean by unpaired t test. A HOMA value of 2.4 was taken as comparator as the value exhibited evidence of diabetic kidney disease in an Indian study22. Serum iron value of 150 µg/dl was taken as upper reference limit for both sexes considering 145 and 160 as upper reference limit (URL) for females and males, respectively as per the kit insert.
Insulin resistance was not found to be significantly associated with total iron. Serum total iron values <150 and >150 µg/dl were compared with HOMA values <2.4 and >2.4 for both sexes. No association was seen when the means of total free iron were compared with HOMA<2.4 and HOMA>2.4 (15.7±1.64 vs16.02±2.56 ppm); insulin resistance was not related to Fe3+/Fe2+ ratio either in males or in females. Obesity, as body mass index (BMI in kg/m2) >2523 was compared with HOMA, the association was significant at (P<0.01). Free iron has been known to cause damage by generation of free radicals. As obesity with raised amount of adipose tissue contributes to more serum iron and serum iron is known to contribute to insulin resistance, we decided to multiply the BMI with the ferric-ferrous ratio, and took the product (BMI×Fe3+/Fe2+) as the index value. The median value of the distribution was around 0.37, the mode was 0.3, and HOMA was compared with values above and below 0.3 in females and males.
Iron contributes to insulin resistance (IR) by hindering its action on liver. It also retards the catabolism of insulin leading to hyperinsulinaemia. Insulin contributes to iron overload by generating more transferrin receptors, more ferritin and entry of iron into the fat cells24. So with more number of fat cells, more iron will be present in the body. This will contribute to insulin resistance. A significant difference was obtained in females (P<0.001) but not in males when the index was compared to HOMA of 2.4. Also, concordance of our index values between females and males showed significance (P<0.001) (Table I). Thus, one can assume that the product of free iron ratios and BMI bears a stronger association with IR in females than in males or BMI alone. A mean free iron value of 15.82±1.38 ppm (n=111) was found in patients with diabetes, whereas it was 9.28±1.21 ppm in healthy controls (n=30) (P<0.001).

The stronger relationship with the index in females may be due to lesser amount of iron stores in them25. Ferric form contributes more to IR possibly as the origin of free iron is supposed to be from transferrin which contains iron in its ferric form. Ferric form may represent the initial active redox state of iron before being reduced to ferrous form. This led us to hypothesize that with more iron in ferric form, there would be more free iron turnover and hence more damage. Though higher amounts of both free and total iron were found amongst patients with microalbuminuria and lower eGFR, the results were not significant in our population which may be due to the presence of lesser amount of nephropathy in patients.
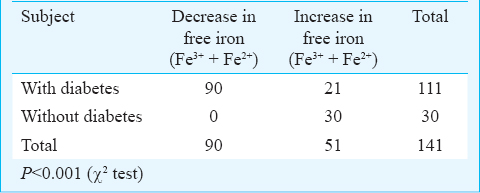
Free iron was considerably reduced in the serum of most patients with diabetes upon addition of conarachin I with a few showing increase whereas serum samples of healthy subjects showed increase in the free iron concentration upon addition of conarachin I. The difference between the two groups was significant (P<0.001) (Table II). Patients with diabetes (mean fasting plasma glucose = 164.77±16.84 mg/dl) had a higher level of free iron than healthy individuals possibly due to more generation of non-transferrin bound iron (NTBI) by glycation of apotransferrin which does not bind iron avidly26. It was interesting to observe that the higher plasma glucose level in patients with diabetes renders the medium reducing so as the initial Fe3+/Fe2+ equilibrium in plasma is maintained even after being exposed to aerial oxidation for up to 72 h27. The serum of patients with diabetes having higher mean fasting plasma glucose levels might enhance the complexing ability of conarachin I and reduce the free iron level. In healthy controls with normal glucose levels, addition of the protein conarachin I from outside probably disturbs the equilibrium of transferrin bound iron and releases some bound iron free thus increasing the free iron level. The results indicate that peanut proteins may serve to design therapeutics to reduce excess free iron in patients with diabetes and hence control sugar levels especially in insulin resistant female patients.
In conclusion, free iron was significantly raised in serum of patients with T2DM when compared with healthy subjects. The calculated index of the product of BMI with the ferric-ferrous ratio may be important in assessing insulin resistance, particularly in females or BMI at any level of glycaemia. A peanut protein, conarachin I binds with the free iron in the serum of patients with diabetes and may contribute to the reduction of insulin resistance. The limitation of the study was that serum ferritin and total iron binding capacity (TIBC) were not measured. As serum ferritin is falsely raised in inflammatory states, thus may contribute as a confounding factor. The use of peanut protein to bind serum free iron is a subject of further investigations in animal models.
Acknowledgment
Authors acknowledge the assistance of Ms Pamela Chowdhury, NEERI, Kolkata, India, during analysis of plasma-iron and Dr Mrityunjoy Sarkar, M.R.Bangur Hospital for his help in collection of serum samples. The second author (SKG) acknowledges Council of Scientific & Industrial Research, India [Sanc. No. 09/028(0929)/2014-EMR-I dated 11/08/2014] for providing SRF.
References
- Prevalence and trends of the diabetes epidemic in South Asia: a systematic review and meta-analysis. BMC Public Health. 2012;12:380.
- [Google Scholar]
- Prevalence of undernutrition and anemia among the child beneficiaries of mid-day meal program. Int J Adv Nutr Health Sci. 2014;2:52-8.
- [Google Scholar]
- Body iron stores and heme-iron intake in relation to risk of type 2 diabetes: A systematic review and meta-analysis. PLoS One. 2012;7:e41641.
- [Google Scholar]
- Dietary iron intake, body iron stores, and the risk of type 2 diabetes: a systematic review and meta analysis. BMC Med. 2012;10:119.
- [Google Scholar]
- The insulin resistance epidemic in India: fetal origins, later lifestyle, or both? Nutr Rev. 2001;59:1-9.
- [Google Scholar]
- Insulin resistance, inflammatory biomarkers, and adipokines in patients with chronic kidney disease: effects of angiotensin II blockade. J Am Soc Nephrol. 2006;17(12 Suppl 3):S206-S12.
- [Google Scholar]
- Clinically overt hereditary hemochromatosis in Denmark 1948-1985: epidemiology, factors of significance for long-term survival, and causes of death in 179 patients. Ann Hematol. 2001;80:737-44.
- [Google Scholar]
- Noninvasive prediction of fibrosis in C282Y homozygous hemochromatosis. Gastroenterology. 1998;115:929-36.
- [Google Scholar]
- The molecular and cellular basis of iron toxicity in iron overload (IO) disorders. Diagnostic and therapeutic approaches. Thalassemia Rep. 2013;3(s1):e3.
- [Google Scholar]
- Serum free iron concentration in patients with type 2 diabetes mellitus with good and poor control and its correlation with glycemic control. Int J Diab Res. 2013;2:33-8.
- [Google Scholar]
- The determination of ferric iron in plants by HPLC using the microbial iron chelator desferrioxamine E. Biometals. 2005;18:53-62.
- [Google Scholar]
- Clinical diagnosis and management by laboratory methods. (16th ed). Philadelphia: WB Saunders; 1974. p. :263.
- [Google Scholar]
- Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412-9.
- [Google Scholar]
- Deficiency in the detection of microalbuminuria by urinary dipstick in diabetic patients. Diabetes Care. 2003;26:3195-6.
- [Google Scholar]
- Evaluation of a new immunoturbidimetry technique for measuring microalbuminuria. Boll Soc Ital Biol Sper. 1991;67:273-8.
- [Google Scholar]
- Peanut protein sensitivity towards trace iron: a novel mode to ebb allergic response. Food Chem. 2015;176:308-13.
- [Google Scholar]
- Methods in biostatistics: for medical students and research workers. New Delhi: Jaypee Brothers Medical Publishers; 1997.
- [Google Scholar]
- Insulin resistance at different stages of diabetic kidney disease in India. J Assoc Physicians India. 2010;58:612-5.
- [Google Scholar]
- Implications of the revised Consensus body mass indices for Asian Indians on clinical obstetric practice. J Clin Diagn Res. 2014;8:OC01-3.
- [Google Scholar]
- Body iron stores are increased in overweight and obese women with polycystic ovary syndrome. Diabetes Care. 2005;28:2042-4.
- [Google Scholar]
- Harrison's principles of internal medicine. (18th ed). New York: McGraw Hill; 2012. p. :847-8.
- [Google Scholar]
- Study of nonenzymatic glycation of transferrin and its effect on iron - binding antioxidant capacity. Iran J Basic Med Sci. 2010;13:194-9.
- [Google Scholar]
- Essential biochemistry. (3rd ed). New Jersey, USA: John Wiley & Sons, Inc; 2013. p. :626-7.
- [Google Scholar]





