Translate this page into:
Female genital tuberculosis: Revisited
For correspondence: Dr Jai Bhagwan Sharma, Department of Obstetrics & Gynaecology, All India Institute of Medical Sciences, Ansari Nagar, New Delhi 110 029, India e-mail: jbsharma2000@gmail.com
-
Received: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Female genital tuberculosis (FGTB) is caused by Mycobacterium tuberculosis (rarely Mycobacterium bovis and/or atypical mycobacteria) being usually secondary to TB of the lungs or other organs with infection reaching through haematogenous, lymphatic route or direct spread from abdominal TB. In FGTB, fallopian tubes are affected in 90 per cent women, whereas uterine endometrium is affected in 70 per cent and ovaries in about 25 per cent women. It causes menstrual dysfunction and infertility through the damage of genital organs. Some cases may be asymptomatic. Diagnosis is often made from proper history taking, meticulous clinical examination and judicious use of investigations, especially endometrial aspirate (or biopsy) and endoscopy. Treatment is through multi-drug antitubercular treatment for adequate time period (rifampicin, isoniazid, pyrazinamide, ethambutol daily for 60 days followed by rifampicin, isoniazid, ethambutol daily for 120 days). Treatment is given for 18-24 months using the second-line drugs for drug-resistant (DR) cases. With the advent of increased access to rapid diagnostics and newer drugs, the management protocol is moving towards achieving universal drug sensitivity testing and treatment with injection-free regimens containing newer drugs, especially for new and previously treated DR cases.
Keywords
Fallopian tubes
female genital tuberculosis
GeneXpert
infertility
Mycobacterium tuberculosis
Introduction
Tuberculosis (TB) remains a major public health problem globally with 10 million persons developing active TB each year with 1.33 million deaths1. Most (85%) TB deaths occur in developing countries, especially Asia (55%) and Africa (30%) with most (75%) cases being from 15-45 yr age group1. Multi-drug resistant (MDR) and extensively drug-resistant (XDR) TB, which have high morbidity and mortality are matters of real concern1.
The World Health Organization (WHO) declared TB, a global emergency in 1993 and recommended the Directly Observed Treatment Short-course (DOTS) strategy to tackle the disease globally, especially in developing countries2. The Revised National TB Control Programme (RNTCP) of India has incorporated the DOTS strategy all over India by the end of 2005 diagnosing about 71 per cent cases and curing above 87 per cent cases with a seven-fold reduction in mortality3.
Female genital TB (FGTB) was first reported by Morgagni in 1744 on the autopsy of a young woman who died of TB peritonitis4. The incidence of FGTB, a type of extrapulmonary TB (EPTB) is increasing in young women globally567. The FGTB causes menstrual dysfunction and infertility in women6891011. Early detection and suitable combination treatment regimens with adequate dosages of drugs can reduce damage and future infertility in these women891011.
Epidemiology of female genital tuberculosis
Genitourinary TB is responsible for 27.1 per cent cases of EPTB with genital TB being seen in nine per cent cases7. The exact incidence of FGTB is not known due to underreporting of cases, asymptomatic cases, vague symptomatology and the lack of reliable diagnostics with high sensitivity891011. The reported incidence is different in different nations being one per cent in infertility clinics of the USA12, one per cent in the Scandinavian countries13, 4-8 per cent in Pakistan1415, 15-21.1 per cent in South Africa16, 1-19 per cent in different areas of India1718. High incidence (26%) has been reported from tertiary centres due to referred cases19, as also (up to 48%) in women registering for assisted reproduction20.
HIV infection has increased the incidence of EPTB and FGTB both in India and Africa2122 due to poor immunity. The mean age of developing FGTB is 40 yr in developed nations913. However, the disease presents in younger age group (20-30 yr) in Asia due to early marriage and child-bearing in them891011.
Pathogenesis
Mycobacterium tuberculosis (rarely Mycobacterium bovis and/or atypical mycobacteria) is the aetiological agent. High-risk factors for TB are poverty, overcrowding, lack of healthcare facilities, poor ventilation, diabetes, illicit drug use, kidney ailment and HIV infection6891011122122. Genital TB mostly spreads from the lungs or other organs with transmission being usually by haematogenous or lymphatic route or sometimes direct spread from adjacent organs (bowel or lymph node). It may be sexually-transmitted through infected semen from active genitourinary TB in the male partner12.
Fallopian tubes
Both fallopian tubes are involved in most (>90%) women in FGTB and the involvement can be TB endosalpingitis, exosalpingitis, interstitial TB salpingitis and Salpingitis isthmica nodosa8910111219. In tuberculous endosalpingitis, with the haematogenous route of spread, the infection starts from endosalpinx making tubes swollen, oedematous and irregular with the formation of hydrosalpinx, pyosalpinx, tubo-ovarian masses and dense adhesions8910111219. Endosalpinx may be hyperplastic or oedematous or totally destroyed by disease making women more susceptible to ectopic pregnancy and infertility681223. In tuberculous exosalpingitis, infection starts in the muscularis mucosa of oviducts with hyperaemia, flimsy adhesions and miliary tubercles on the surface of the tubes689101112. Later beading, closed tubes, tubo-ovarian masses, hydrosalpinx, pyosalpinx and the development of synechiae formation occurs89101112.
Hydrosalpinx and the tubal condition can be graded on laparoscopy and laparotomy as per the type of adhesions, patency of tubes, morphology of tubes and fimbrial stricture for prognostication of fertility2425.
Uterus
The endometrium is affected in 50-80 per cent (average 70%) patients through haematogenous, lymphatic or contagious route. Initially, there are no obvious lesions, later ulcers are formed and in advanced stages, distortion of the uterus occurs due to synechiae. The lesions can be focal or multiple ulcers, necrosis or haemorrhagic areas. Destruction of the endometrium may occur with Asherman's syndrome manifesting as secondary amenorrhoea and infertility26. On microscopy, typical caseative epithelioid granulomas, epithelioid cells and specialized Langerhans giant cells may not form due to the shedding of the endometrium during menstruation. The presence of a focal collection of lymphocytes on endometrial biopsies may also indicate FGTB18.
Ovaries
Ovaries are affected in 20-30 per cent patients with adhesions, caseation, adnexal cyst or mass formation with defective ovarian function and reserve and sometimes complete destruction of ovary2728. Sometimes tubo-ovarian cyst can manifest as acute abdomen simulating acute appendicitis and may be diagnosed on laparoscopy or laparotomy29.
Peritoneum
Pelvic and abdominal peritoneum is often involved in abdomino-pelvic TB with multiple tubercles, ascites and abdominal masses simulating ovarian cancer30. Various types of adhesions are formed in the pelvis and abdomen such as perihepatic synechiae (Fitz-Hugh-Curtis syndrome), hanging gall bladder sign and ascending colonic synechiae and frozen pelvis in the abdomino-pelvic TB313233. Ascitic fluid sampling for biochemical analysis (increased adenosine deaminase levels) and peritoneal biopsy may confirm the diagnosis of TB and thus can avoid laparotomy. FGTB and endometriosis may present together in some cases34.
Cervix
The cervix may be involved in about five per cent cases of genital TB usually secondary to tubal or endometrial TB, but may rarely be primary disease transmitted by the partner through infected semen. It manifests as polypoidal growth or ulceration simulating cervical cancer necessitating biopsy and histopathological demonstration of granulomatous inflammation35.
Vagina and vulva
The involvement of vagina and vulva is rare and is usually an extension from endometrium or cervix, or rarely primary due to transmission from an infected semen of the partner. There may be a hypertrophic ulcer or growth on the vulva or vagina requiring biopsy and histopathological demonstration of granuloma and to rule out cancer and other diseases such as syphilis and lymphogranuloma venereum89101136. Rarely, a giant vulval tumour may be formed in FGTB37. Even vesicovaginal and rectovaginal fistulas can rarely occur in FGTB38.
Infertility in genital tuberculosis
Both primary and secondary infertility can occur in FGTB (40-80% among FGTB cases) due to various causes as given below:
Tubal factors
Tubal factors include unilateral and bilateral tubal blockage, loss of tubal function due to ciliary damage in FGTB, perisalpingitis causing adhesions and tubo-ovarian mass formation, and unilateral or bilateral hydrosalpinx with or without obstruction affecting fertilization and embryonic implantation3940.
Defective ovarian function
Endocrine dysfunction, chronic anovulation, antigonadotropic effect of M. tuberculosis even on an in vitro fertilization (IVF) cycle, poor quality of embryo due to intrinsic oocyte factor defect and decreased production of progesterone (luteal phase defect), implantation failure, lower pregnancy rates and higher abortion rates are observed in FGTB2728.
Uterine (endometrial) factors
Genital TB affects endometrial receptivity leading to defective endometrial markers and vascularization of the endometrium, and endometrial atrophy and synechiae formation26. Defective or failed implantation has also been reported in FGTB41. In FGTB, there is T-helper-1 cell (Th-1) response that leads to implantation failure instead of Th-2 cell response needed for successful implantation of fertilized ovum. Hence, FGTB shifts Th-2 response to Th-I response in endometrium leading to implantation failure. In fact, Dam et al41 observed latent FGTB to be an important cause of repeat IVF failure in Indian setting through poor implantation.
Clinical signs and symptoms of FGTB are depicted in Table I.
| Symptoms | Signs |
|---|---|
| No symptoms (10%) | No sign (10%) |
| General systemic symptoms | Raised temperature |
| Pyrexia | Lymphadenopathy |
| Anorexia | (in lymph nodes TB) |
| Weight loss Feeling unwell, Malaise |
Crackles on chest auscultation (PTB) |
| Menstrual symptoms | Abdominal examination |
| Puberty menorrhagia Heavy menstrual bleeding (in early stage) |
Vague or definite abdominal or pelvic lump |
| Postmenopausal bleeding | Ascites |
| OligomenorrhoeaHypomenorrhoea | Doughy feel of abdomen |
| Amenorrhoea | Vaginal examination |
| (primary and secondary) Dysmenorrhoea |
Soft tender enlarged uterus (pyometra) Tenderness and induration in the fornices |
| Infertility (primary and secondary) | |
| Lump in adnexa | |
| Abdominal or pelvic mass | Fullness and tenderness in the pouch of Douglas |
| Abdominal and pelvic pain | |
| Acute abdomen | |
| Vaginal discharge | Unusual findings |
| Douglas ulcers or growth | Solid lesions on external genitalia |
| Urinary incontinence or feacal incontinence | Ulcers on external genitalia Genital fistula |
Diagnosis
Differential diagnosis varies as per organ involvement and symptoms (Table II). Due to paucibacillary nature of FGTB, microbiological diagnosis of M. tuberculosis is usually difficult. One should think of TB in women with chronic pelvic inflammatory disease, chronic vaginal discharge, unexplained infertility not responding to standard treatment6891011. Combination of various methods is used to make a diagnosis of FGTB689101142, which include history taking, general physical examination [inclusive of evidence of TB elsewhere in the body like lymphadenopathy (lymph node TB), bones and joints (skeletal TB), chest auscultation (pulmonary TB), abdominal examination (abdominal TB) and ascites], and gynaecological examination.
| In patients with tubo-ovarian mass |
| Ectopic gestation |
| Appendicitis |
| Endometriosis |
| Pelvic inflammatory disease (acute and chronic) |
| Tuberculosis of endometrium |
| Abnormal uterine bleeding |
| Endometrial hyperplasia |
| Endometrial polyp |
| Endometrial cancer |
| Ovarian tuberculosis |
| Ovarian cyst |
| Ovarian cancer |
| Ovarian ectopic pregnancy |
| In patients with granulomas |
| Treponema pallidum infection |
| Antinomycosis |
| Leprosy |
| Lymphogranuloma venereum |
| Regional ileitis |
| Histoplasmosis |
| Brucellosis |
| Schistosomiasis |
| Filariasis |
| Cervical tuberculosis |
| Cervical cancer |
| Cervical hypertrophy |
| Cervical ectopic |
| Vaginal tuberculosis |
| Vaginal cancer |
| Vaginal cyst |
| Vaginal warts |
| Vulval TB |
| Vulval cancer |
| Bartholin abscess |
| Condyloma acuminata |
| Condyloma lata |
| Vulval and vaginal warts |
Investigations
-
(i)
-
(ii)
X-ray chest (postero-anterior view) may show active pulmonary TB (fibrocavitory disease, infiltrations, mediastinal or hilar lymphadenopathy, miliary TB) or old healed lesions of past TB.
-
(iii)
Mantoux/(Tuberculin) test and interferon gamma release assay (IGRA)43: These have sensitivity of 55 per cent and specificity of 80 per cent and alone cannot be used for diagnosis of FGTB. Positive tests just indicate infection but not disease and negative tests do not rule out infection.
-
(iv)
Blood markers: Cancer antigen 125 (CA 125) is a good tumour marker for ovarian malignancies (normal levels <35 U/ml). However, its levels can be significantly raised in advanced abdominal tuberculosis. Thakur et al44 reported a very high (1255 U/ml) levels of CA 125 in their case of advanced abdominal tuberculosis, which came down to 42 U/ml after one month of ATT (antitubercular treatment). Its levels are only moderately raised usually <200 U/ml in FGTB (as compared to the higher rise in thousands in cancer ovary)1130. However, CA 125 is not a very reliable marker for the diagnosis of FGTB8.
-
(v)
Imaging methods: These are of use only in tubo-ovarian masses. Ultrasonography (USG) may show tubo-ovarain masses with calcification and fluid in the pouch of Douglas5845. It may show thin endometrium, the heterogenous appearance of the endometrium, endometrial fluid, calcification or bands and intrauterine synechiae45. It can demonstrate hydrosalpinges with cog wheel sign and inhomogenous enlarged ovaries with free peritoneal fluid and fixed adnexal masses45.
Computerized axial tomography (CAT) scan (Fig. 1) may show masses in abdomen and pelvis with ascites, thickened and enhanced peritoneum, with lesions in the abdominal viscera and lymph node46. Magnetic resonance imaging (MRI) has a higher resolution and may show tubo-ovarian masses. Unilateral or bilateral tubo-ovarian masses, hydrosalpinx, adnexal cysts or tuberculous deposits on peritoneum or liver have been reported in our study47. Positron-emission tomography (PET) scan shows unilateral or bilateral tubo-ovarian masses with increased fluorodeoxy glucose (FDG) uptake by TB lesion4849. We observed increased FDG uptake by TB lesions in our study on 17 women of tubercular tubo-ovarian masses (Fig. 2). It also helps in differentiating between carcinoma ovary and abdomino-pelvic TB. Hysterosalpingography (HSG) is contraindicated in FGTB as it can result in flare-up of subclinical infection. However, it is often performed as part of infertility workup in unsuspected cases. It shows the internal architecture of the uterus and tubes and thus helps in the diagnosis of FGTB (Figs 3 and 4). Various HSG findnigs like tobacco pouch, golfclub and maltese cross appearance of tubes and shruken uterine cavity with tubal block have been reported by different authors in FGTB505152.
-
(vi)
Microbiological tests: Endometrial biopsy, curettage or aspirate performed in the luteal phase (day 21) are the most important tests for the diagnosis of genital TB6891011. All efforts should be made to achieve microbiological confirmation. Demonstration of typical caseous granuloma with or without Langerhans giant cells on histopathology is diagnostic of genital TB. Multiple biopsies may increase pick up rate53. WHO approved rapid diagnostic tests (WRDT) are cartridge based nucleic acid amplification test (CBNAAT/ GeneXpert MTB/RIF) and liquid culture by mycobacterial growth indicator tube (MGIT) with phenotypic drug sensitivity testing (DST) or genotypic DST by line probe assay (LPA) are done on endometrial sample sent in saline545556. Polymerase chain reaction (PCR) is a fast, sensitive and specific test to diagnose mycobacterial DNA in endometrial sample by targeting 65 kDa and the mpt 64 gene5758. It has a high sensitivity and can detect 1-10 bacilli per ml5758. However, the false-positive rate of PCR is high. Many researchers have advised against PCR for the rapid detection of TB59. Rana et al60 observed better results of reverse transcriptase-PCR in the detection of FGTB. In our experience, there is high false positivity of PCR and it is recommended not to start antitubercular treatment (ATT) only on positive PCR unless there is evidence of FGTB clinically on examination, or on radiology or endoscopy81161.
A positive CBNAAT (cartridge based nucleic acid amplification test) result is a useful confirmation, but a negative test does not always rule out TB. The Xpert MTB/RIF is an automated test which can detect purified DNA of M. tuberculosis on the endometrial sample. It can also detect rifampicin resistance and can give report within two hours. Sharma et al62 observed GeneXpert) to have a 33-50 per cent sensitivity, 100 per cent specificity for the diagnosis of FGTB. We also observed 35 per cent sensitivity and 100 per cent specificity in the detection of FGTB with GeneXpert63.
Loop-mediated isothermal amplification (LAMP) assay has been used on endometrial biopsy64 Sethi et al64 observed high sensitivity of 66.18 per cent for LAMP in contrast to 29.4 per cent for AFB smear, 10.29 per cent for AFB culture, 8.82 per cent for histopathology and 95 per cent for PCR. They also observed a high concordance of 63 per cent between PCR and LAMP.
-
(vii)
Hysteroscopy: It is endoscopic visualization of endometrial cavity and may be normal in the absence of endometrial TB (as the uterus is involved in only about 70% of cases of TB) and in early disease. Usually, there is a pale looking cavity, the presence of tubercles, small white caseous nodules, varying grades of intrauterine synechaie (Fig. 5) and Asherman's syndrome2665. Kumar and Kumar66 observed white caseous nodules as stars shining against the blue background of methylene blue dye in their study of endometrial TB on hysteroscopy at higher magnification. As there is a high-risk of complications and difficulties in performing hysteroscopy in FGTB cases due to the small shrunken cavity, the procedure needs to be performed by expert gynaecologists preferably under laparoscopic guidance67.
-
(viii)
Laparoscopy: A laparoscopy or dye test performed under general anaesthesia is the most reliable modality for the detection of FGTB and abdomino-pelvic TB, particularly affection of oviducts, ovaries and peritoneum. It is often done with hysteroscopy for better results. While performing laparoscopy one has to carefully visualize the whole of the peritoneal cavity (and not only pelvis) by rotating the laparoscope by 360° systematically [ first pelvis for genital organs, then ileocecal region, ascending colon, hepatic flexure, liver, gallbladder, stomach, whole of small bowel, descending colon, omentum (Fig. 6) and whole of peritoneum] to observe various lesions and adhesions of TB and any other coincidental findings8116869.
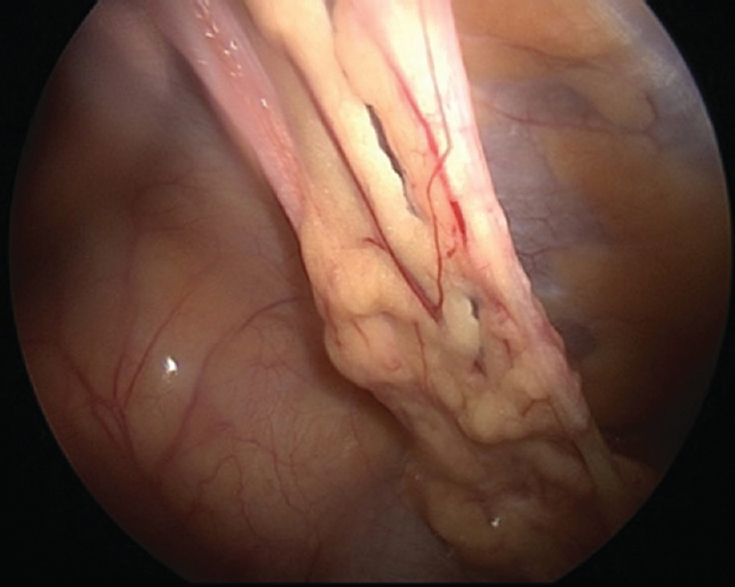
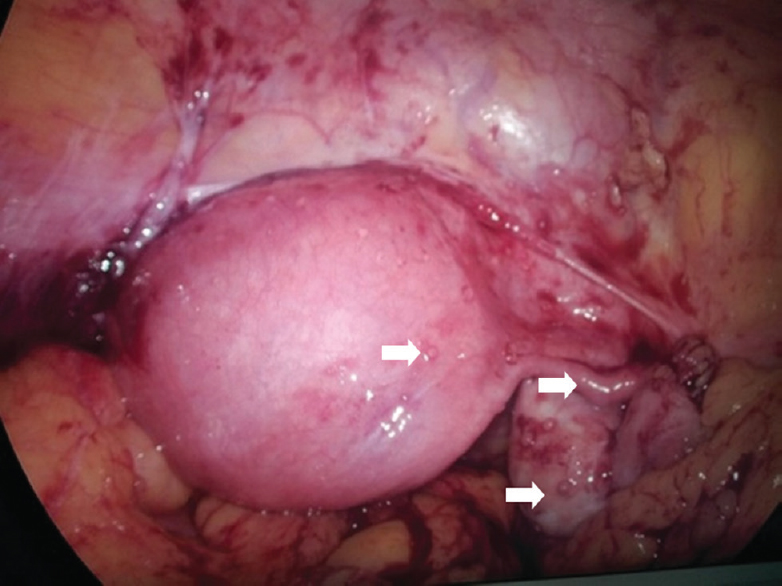
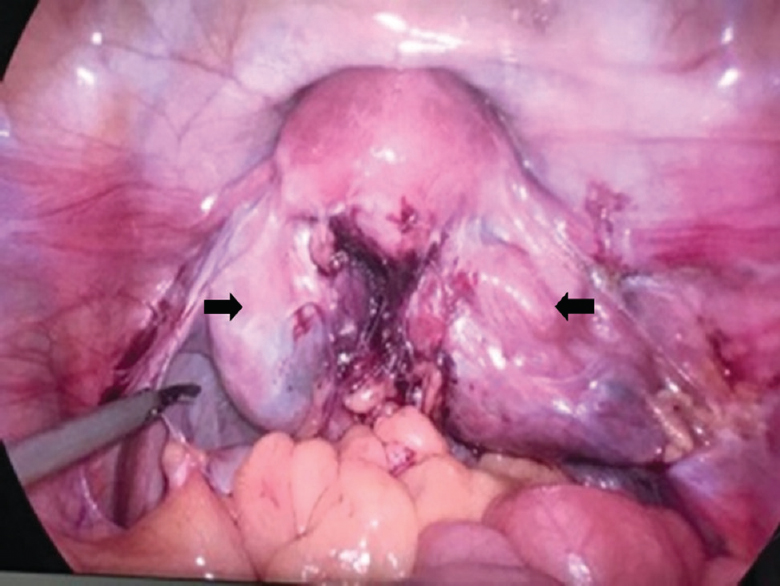
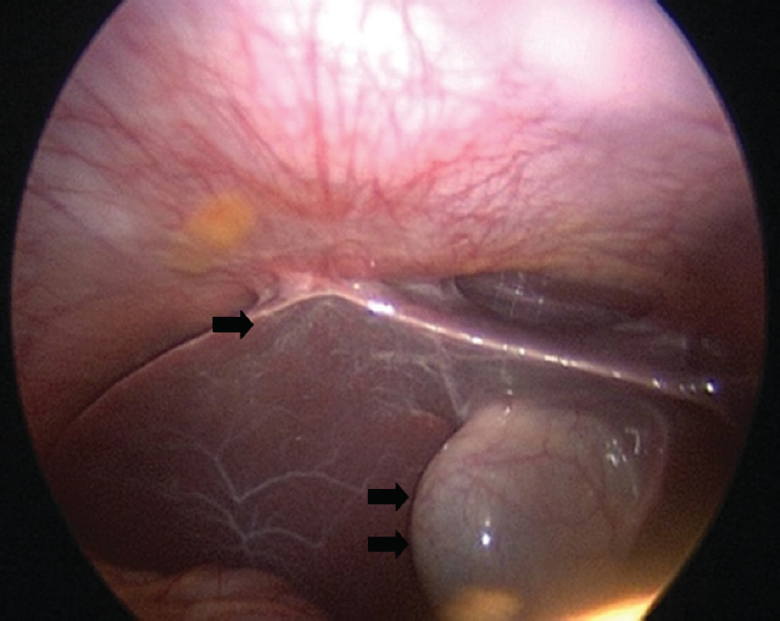
Various laparoscopic findings can be as follows: (a) In subacute stage, the findings are congestion, oedema, fluid-filled pockets, miliary tubercles (Fig. 7), white yellow and opaque patches on the uterus, tubes, ovaries and peritoneum; (b) In chronic stages, there may be small swollen tubes with agglutinated fimbriae (nodular salpingitis), varying types of tubal block (fimbrial, mid tubal or cornual block), beading of tubes, hydrosalpinx (Fig. 8) and pyosalpinx caseous nodules can be seen in utero vesical pouch (Fig. 9); (c) We observed alternate constrictions and dilatations of fallopian tubes on injection of methylene blue in FGTB cases (Sharma's blue python sign)70. Fusion of fimbrial ends due to caseous material in a case of FGTB (Sharma's Kissing fallopian tube sign)71 and calcified tubes like a dried tree branch (Sharma's Dried tree branch sign)72 were also observed in FGTB cases; and (d) Varying grades of abdominal and pelvic adhesions (Fig. 6) are common in FGTB. The adhesions are thick and vascular. We have observed a high incidence (48%) of perihepatic synechiae (Fitz-Hugh-Curtis Syndrome) in FGTB cases31. Hanging gall bladder sign due to perihepatic adhesions was also observed in FGTB (Fig. 10)32. Another observation was ascending colonic adhesions at the junction of lower 2/3rd and upper 1/3rd of ascending colon in abdomino-pelvic TB33.
It has been observed that performing laparoscopy in FGTB is difficult and associated with risk such as the inability to see pelvis (10.3%), excessive bleeding (2.3%), and peritonitis (8%), and should be performed by experienced gynaecologists73.
-
(ix)
Combination of tests and diagnostic algorithm: Ultimately, the diagnosis of FGTB is made by meticulous examination and suitable investigations like endometrial sampling, radiology (in tubo-ovarian masses) and the use of hysteroscopy and laparoscopy. An algorithm has been developed for FGTB in INDEX-TB Guidelines, an initiative of Central TB Division, Ministry of Health and Family Welfare, Government of India and the WHO in 2016 for the diagnosis and management of FGTB74. Another Indian team is also working to develop an algorithm suitable for the detection and management of FGTB75. It is mandatory to notify every case diagnosed and treated under NIKSHAY, a web-based notification system maintained by the Ministry of Health and Family Welfare, Government of India (http://nikshay.in).
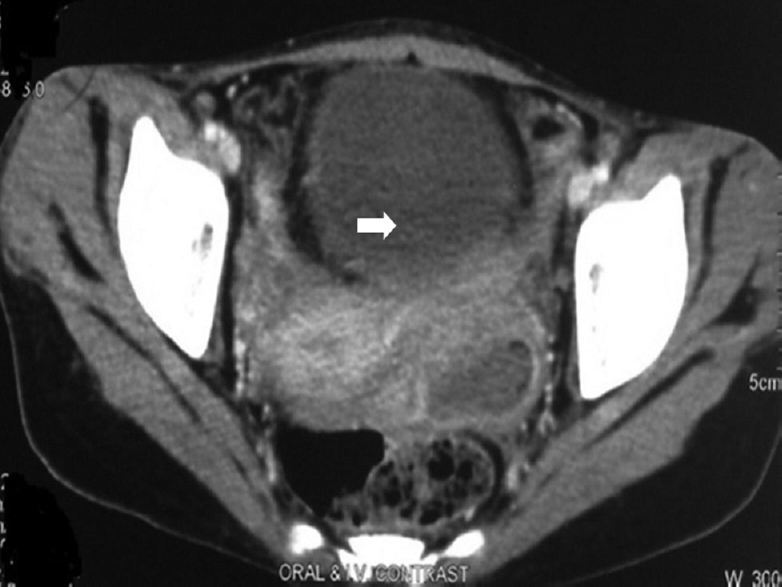
- Computed tomography with unilateral tubo-ovarianmass in female genital tuberculosis.
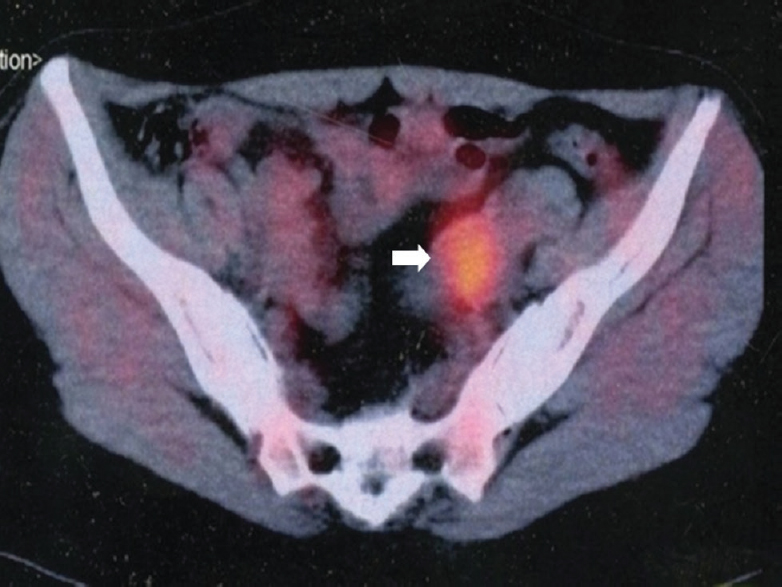
- Positron emission tomography and computed tomography scan showing unilateral increased FDG uptake in tubo-ovarian masses (arrow).
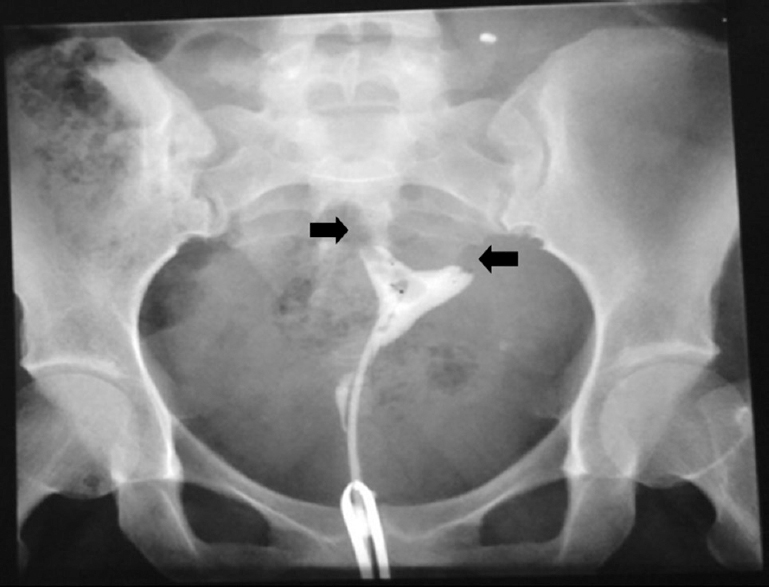
- Hysterosalpingography showing bilateral tubal block (arrows).
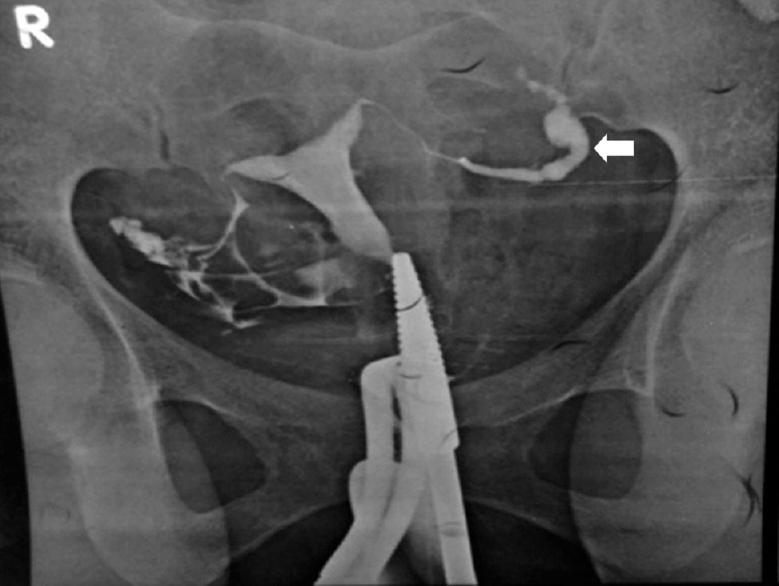
- Hysterosalpingography showing left hydrosalpinx with fimbrial block (arrow).
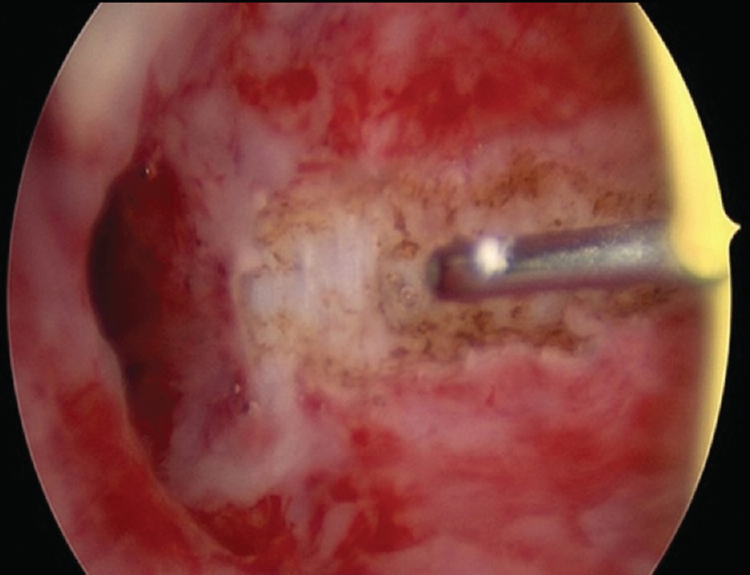
- Hysteroscopy showing grade II adhesions in female genital tuberculosis being resected.
- Laparoscopy showing omental adhesions.
- Laparoscopy showing tubercles on uterus, fallopian tubes and ovaries (arrows).
- Laparoscopy showing bilateral hydrosalpinxs, tubo-ovarian masses, adhesions and frozen pelvis (arrows).
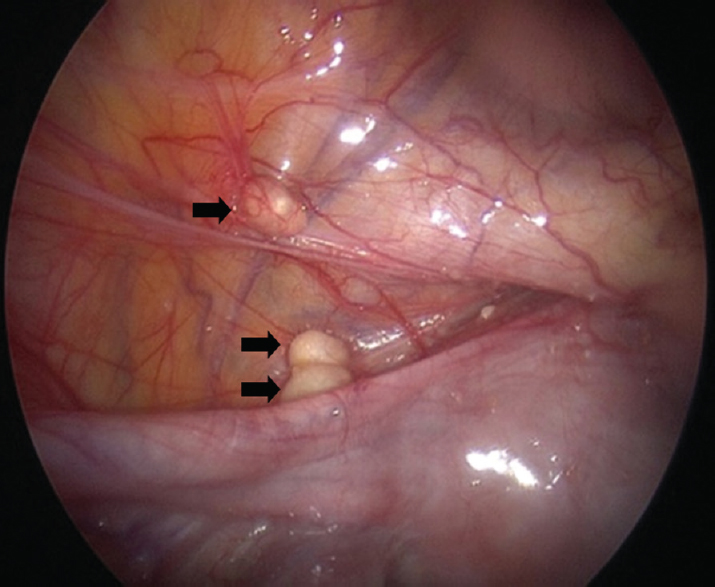
- Laparoscopy showing caseous nodules in uterovesical pouch (single arrow) and on anterior abdominal wall (double arrow).
- Laparoscopy showing Fitz-Hugh-Curtis syndrome (single arrow) and hanging gall bladder sign (double arrow).
Treatment
All new cases, whether microbiologically confirmed or clinically diagnosed and drug sensitive previously treated patients (non-responders, failures, recurrent TB, lost to follow up for one month after receiving one month of ATT) are given combination therapy. Medical therapy with anti-tubercular drugs for 6-9 months is effective for these FGTB cases76. In a randomized controlled trial, six months ATT was found to be equally effective as nine months therapy77.
Directly observed treatment short course strategy (DOTS)
The treatment of FGTB is shown in Fig. 11. DOTS is favoured and recommended by the WHO1. Daily treatment is given under direct supervision of a treatment supporter. Four drugs isoniazid (H), rifampicin (R), pyrazinamide (Z) and ethambutol (E) is given for two months (HRZE), followed by H, R and E (HRE) daily for four months (Fig. 11). Thrice-weekly regimen is no longer used.
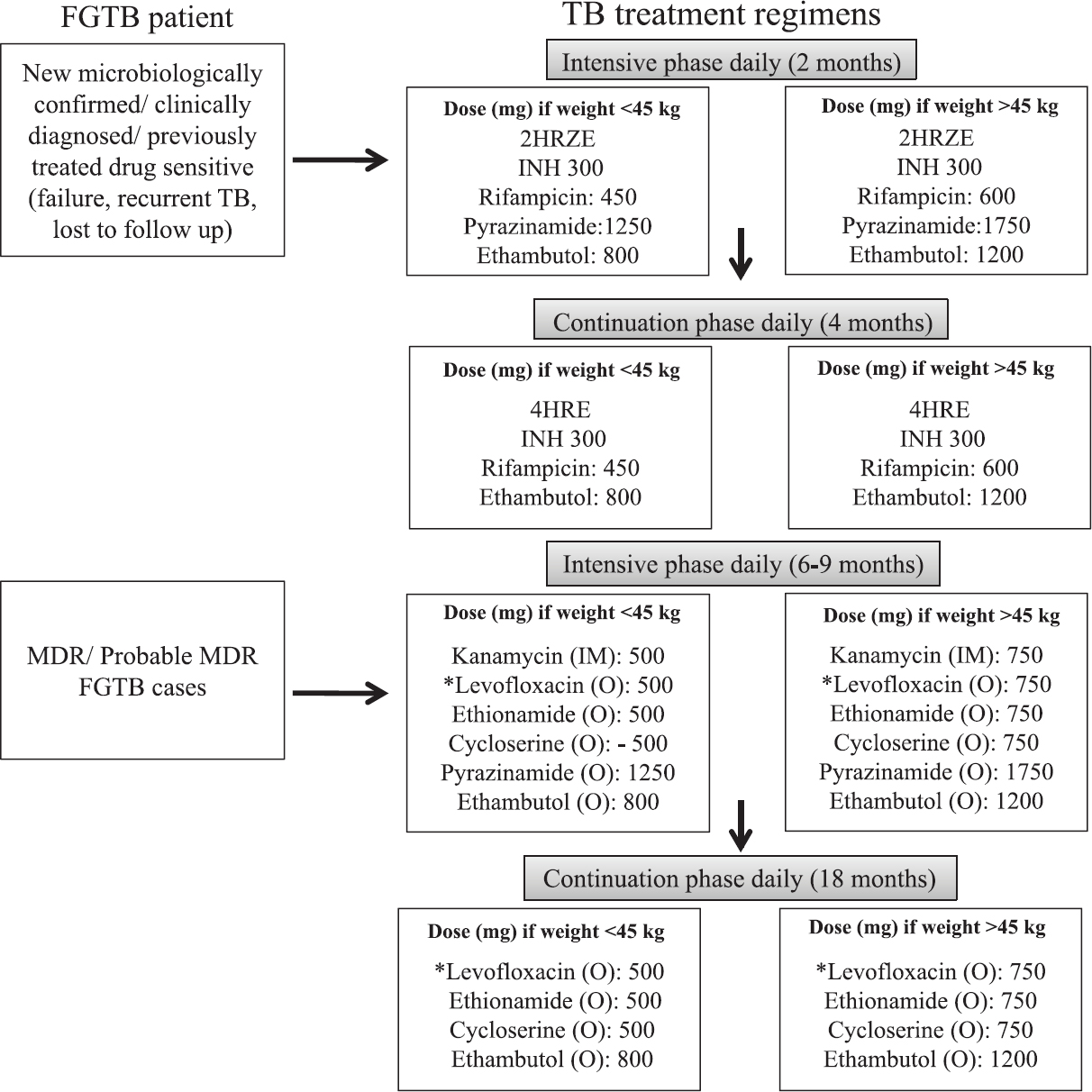
- Treatment regimens for female genital tuberculosis (FGTB). *Moxifloxacin to be given, if resistance to levofloxacin. Recently, 4 drug fixed dose combination (FDC) HRZE (75, 150, 400, 275) has been introduced. HRZE, isoniazid, rifampicin, pyrazinamide and ethambutol; INH, isoniazid; MDR, multi-drug resistant resistant; IM, intramuscular; O, oral. Source: Refs 13811.
Non DOTS treatment
Self administered therapy for women not willing to take medicines from the DOTS centre can buy combination kits containing four drugs (HRZE) for two months followed by kit containing three drugs (HRE) for four months.
Treatment of HIV-TB and DRTB
If the patient is both HIV and TB positive, both need to be treated. ATT is started to all patients with drug-sensitive or DR TB and HIV irrespective of CD4 cell count, as early as possible, usually by two weeks of initiation of ATT. In drug-sensitive TB patient on the second-line ART, rifampicin is replaced by rifabutin (150 mg daily)13. Any patient who fails to respond clinically and/ or radiologically despite 2 months of supervised adequate ATT is a presumptive DRTB case and should be offered WRDTs to confirm drug sensitivity. The diagnosis of drug resistant TB is based on the results of WRDT. Drug-resistant [RR/ MDR/ XDR (extensively DR)]. FGTB is treated with reserve drugs for 18-24 months like for pulmonary MDR (Fig. 11).
Adverse effects of drugs
First-line drugs are safe and may have minor side effects but rarely serious side effects like hepatitis. However, reserve drugs are toxic and are to be given for longer duration. Various adverse effects of ATT are shown in Table III.
| First line drugs | Side effects |
|---|---|
| Isoniazid | Peripheral neuropathy, seizures Erythema and skin rash Hepatitis Lethargy |
| Rifampicin | Gastrointestinal irritation, hepatitis, skin reaction, flu-like syndrome, anaemia, Thrombocytopenic purpura |
| Pyrazinamde | Hepatitis, gastrointestinal irritation (nausea, vomiting), hyperuricaemia |
| Ethambutol | Optic neuritis |
| Reserve drugs | Side effects |
| Injectable streptomycin, kanamycin and amikacin | Ototoxicity, renal toxicity, vertigo, electrolyte imbalance |
| Quinolones | Gastrointestinal irritation, abdominal pain, nausea vomiting, hepatitis, seizures, dizziness, skin rash, joint pains, photosensitivity QTc prolongation |
| Ethionamide | Gastrointestinal irritation, abdominal pain, nausea, vomiting, hepatitis, hypothyroidism and goiter Hallucination and depression, neuropathy |
| Cycloserine | Neurological effects (dizziness, seizures, headache, tremors, insomnia), hypersensitivity, suicidal tendency, depression |
| Para-amino salicyclic acid | Gastrointestinal irritation, abdominal pain, nausea, vomiting, skin rash, hypothyroidism, hypokalaemia |
Surgical treatment
Schaefer12 had advised surgical treatment by removal of the uterus, both tubes and ovaries for persistent disease, tubercles, pyosalpinx, tubo-ovarian mass, non-healing ulcers in MDR TB despite medical treatment12. Besides, surgical treatment in TB is difficult and hazardous with more complications as observed by us in hysteroscopy and laparoscopy, laparotomy and vaginal hysterectomy performed in women with genital tuberculosis67737879. However, limited surgery in the form of drainage of persistent pelvic or tubo-ovarian abscess despite medical treatment can be performed as recommended by the American Thoracic Society80.
Repeat laparoscopy and hysteroscopy after anti-tubercular treatment
Repeat laparoscopy and hysteroscopy can be performed after completion of a full course of ATT for the disappearance of disease. This also helps in prognostication for treatment of infertility. It was observed that after ATT, minor TB lesions disappeared, but major adhesions, frozen pelvis, blocked tubes (advanced disease) persisted with poor prognosis for fertility81. Bahadur et al82 observed significant improvement in grades I and II adhesions only on repeat hysteroscopy after completion of ATT in FGTB patients, but major adhesions (grade III onwards) persisted. We observed the persistence of advanced Asherman's syndrome and adhesions on repeat hysteroscopy in FGTB patients83. Tuboplasty should be avoided in case of FGTB as it does not improve the prognosis for fertility but there is risk of flare-up of TB and further ectopic gestation after ATT101123.
Assisted reproduction in female genital tuberculosis
Despite ATT, results for fertility is low in FGTB patients with conception rate being only 19.2 per cent1742. In vitro fertilization and embryo transfer (IVF-ET) has been found to be useful modality in treating FGTB with blocked tubes but normal endometrium42848586. Parikh et al84 observed 16.6 per cent pregnancy rate per embryo transfer (ET) with in vitro fertilization (IVF) after completion of ATT in patients with normal endometrium. Jindal et al85 found IVF-ET to be the most effective modality in FGTB with pregnancy rate of 17.3 per cent as compared to only 4.3 per cent with tubal surgery. Malik86 observed a pregnancy rate of 38.2 per cent with IVF-ET in 120 women with FGTB after completion of ATT. Another study observed IVF to be a successful modality in FGTB patients87. Chimote et al88 also recommended IVF-ET as a treatment for FGTB cases with blocked tubes but normal endometrium. If the endometrium is destroyed despite ATT but ovaries are normal, gestational surrogacy can be a successful modality in such patients89. Samantha et al89 observed a viable delivery rate of 50 per cent with gestational surrogacy. If ovaries are destroyed, then adoption is advised to the couple891011.
Tuberculosis (TB) and pregnancy
A patient of pulmonary tuberculosis during pregnancy must take full treatment even in the first trimester as all four primary drugs (isoniazid, rifampicin, pyrazinamide and ethambutol) are safe in pregnancy9. Jana et al90 observed increased maternal and perinatal morbidity in pregnancies complicated of pulmonary TB. The same group observed increased maternal and perinatal morbidity in EPTB cases91. However, with adequate treatment and nutrition and care during pregnancy there is no adverse maternal and perinatal outcome in PTB or EPTB92.
Recent advances and future direction
Research is being conducted to develop newer drugs1142. Recently injection free regimen using bedaquiline and delamanid have been recommended by WHO in their rapid advise and update 201893 and WHO Consolidated Guidelines on Drug Resistant Tuberculosis Treatment (2019)94 against resistant strains of M. tuberculosis and to shorten therapy period. Stem cells, nanotechnology and colostrum are being tested to regenerate fallopian tubes, endometrium and ovaries to treat permanent damage11. The WHO rapid communication93 has stressed upon injection free regimens for all types of TB, including MDR and rifampicin-resistant (RR) TB94. It has also advised discontinuation of category II regimen. For new or all previously treated patients if rifampicin or isoniazid sensitive after ensuring strict clinical, radiological and bacteriological follow up (if available) (2HRZE/4HRE) is given13. For isoniazid-resistant TB patients the uniphasic regimen (6LfxRZE) is given. For MDR, pre-XDR, XDR TB patients the recommended regimen is bedaquiline, levofloxacin (or moxifloxacin), linezolid, cycloserine, clofazimine. Streptomycin, amikacin instead of kanamycin and capreomycin9394 is given if injectable drugs are to be used.
Conclusion
FGTB causes gynecological symptoms such as infertility, menstrual dysfunction and chronic pelvic pain. Diagnosis is made by meticulous history thorough clinical examination and proper use of investigations, particularly endometrial aspirate for AFB culture, PCR and histopathology aided by endoscopy. Treatment is through the first-line drugs in combination (HRZE for two months followed by HRE for four months). Fertility outcome is poor in FGTB, but IVF-ET can be performed for tubal blockage with normal endometrium with a good outcome. Surrogacy can be advised in case of damaged endometrium and adoption if ovaries are damaged. Newer vaccines, diagnostics and medicines (like bedaquiline, delamanid) and stem cell therapy are being developed and tried.
Financial support & sponsorship:
None.
Conflicts of Interest:
None.
Acknowledgment
Authors acknowledge Dr K.S. Sachdeva, Central TB Division, Ministry of Health and Family Welfare, Government of India, New Delhi for his help.
References
- WHO global tuberculosis report 2018. Geneva: WHO; 2018.
- WHO report on the TB epidemic. TB a global emergency. WHO/ TB/ 94.177. Geneva: WHO; 1994.
- Central TB Division, Directorate General of Health Services. India TB. Report: Revised National Tuberculosis Control Programme: Annual status report. New Delhi: Ministry of Health and Family Welfare; 2018.
- [Google Scholar]
- Female genital tuberculosis - a disease seen again in Europe. Vojnosanit Pregl. 2007;64:855-8.
- [Google Scholar]
- Female genital tuberculosis. In: Sharma SK, Mohan A, eds. Tuberculosis (3rd ed). Delhi: Jaypee; 2015. p. :362-71.
- [Google Scholar]
- Tuberculosis and obstetric and gynecological practice. In: Studd J, Tan SL, Chervenak FA, eds. Progress in obstetrics and gynaecology. Vol 18. Philadelphia: Elsevier; 2008. p. :395-427.
- [Google Scholar]
- Current diagnosis and management of female genital tuberculosis. J Obstet Gynaecol India. 2015;65:362-71.
- [Google Scholar]
- Genital tuberculosis in women. Analysis of 187 newly diagnosed cases from 47 Swedish hospitals during the ten-year period 1968 to 1977. Am J Obstet Gynecol. 1980;138:974-7.
- [Google Scholar]
- Incidence of genital tuberculosis in infertile women. J Pak Med Assoc. 1985;35:280-1.
- [Google Scholar]
- Investigation of the prevalence of female genital tract tuberculosis and its relation to female infertility: An observational analytical study. Iran J Reprod Med. 2012;10:581-8.
- [Google Scholar]
- Genital tuberculosis at Tygerberg hospital - prevalence, clinical presentation and diagnosis. S Afr Med J. 1992;81:12-5.
- [Google Scholar]
- Infertility and pregnancy outcome in female genital tuberculosis. Int J Gynaecol Obstet. 2002;76:159-63.
- [Google Scholar]
- Tuberculous endometritis: A clinicopathological study of 1000 cases. Br J Obstet Gynaecol. 1983;90:84-6.
- [Google Scholar]
- Genital tuberculosis in Indian infertility patients. Int J Gynaecol Obstet. 2007;97:135-8.
- [Google Scholar]
- Genital tuberculosis: A leading cause for infertility in women seeking assisted conception in North India. Arch Gynecol Obstet. 2008;278:325-7.
- [Google Scholar]
- Clinical presentation and epidemiology of female genital tuberculosis in Eastern Sudan. Int J Gynaecol Obstet. 2012;118:236-8.
- [Google Scholar]
- Genital tuberculosis: An important cause of ectopic pregnancy in India. Indian J Tuberc. 2014;61:312-7.
- [Google Scholar]
- A new classification system for pregnancy prognosis of tubal factor infertility. Int J Clin Exp Med. 2014;7:1410-6.
- [Google Scholar]
- Genital tuberculosis is common among females with tubal factor infertility: Observational study. Alex J Med. 2015;51:321-4.
- [Google Scholar]
- Genital tuberculosis: An important cause of Asherman's syndrome in India. Arch Gynecol Obstet. 2008;277:37-41.
- [Google Scholar]
- The effect of tuberculosis on ovarian reserve among women undergoing IVF in India. Int J Gynaecol Obstet. 2012;117:40-4.
- [Google Scholar]
- Effect of antitubercular treatment on ovarian function in female genital tuberculosis with infertility. J Hum Reprod Sci. 2016;9:145-50.
- [Google Scholar]
- Tubercular tubo-ovarian cystic mass mimicking acute appendicitis: A case report. J Med Case Rep. 2011;5:363.
- [Google Scholar]
- Abdomino-peritoneal tuberculosis masquerading as ovarian cancer: A retrospective study of 26 cases. Arch Gynecol Obstet. 2010;282:643-8.
- [Google Scholar]
- Fitz-Hugh-Curtis syndrome associated with tuberculous salpingitis and peritonitis: A case presentation and review of literature. BMC Gastroenterol. 2018;18:42.
- [Google Scholar]
- Sharma's hanging gall bladder sign: A new sign for abdomino-pelvic tuberculosis: An observational study. IVF Lite. 2015;2:94-8.
- [Google Scholar]
- Sharma's ascending colonic adhesion: A new sign in abdomino-pelvic tuberculosis with infertility. IVF Lite. 2016;3:18-22.
- [Google Scholar]
- Concomitant female genital tuberculosis and endometriosis. Indian J Tuberc. 2017;64:173-7.
- [Google Scholar]
- Cervical tuberculosis masquerading as cervical carcinoma: A rare case. J Obstet Gynaecol India. 2001;51:184.
- [Google Scholar]
- Hypertrophic tuberculosis of vulva-a rare presentation of tuberculosis. Indian J Tuberc. 2010;57:95-7.
- [Google Scholar]
- Tuberculosis: A rare cause of rectovaginal fistula in a young girl. J Obstet Gynaecol India. 2001;51:176.
- [Google Scholar]
- Genital tuberculosis-ovarian function and endometrial receptivity. In: Mukherjee GG, Tripathy SN, Tripathy SN, eds. Genital tuberculosis (1st ed). New Delhi: Jaypee Brothers Medical Publishers (P) Ltd; 2010. p. :27-42.
- [Google Scholar]
- The significance of cytokines, chemical composition, and murine embryo development in hydrosalpinx fluid for predicting the IVF outcome in women with hydrosalpinx. Hum Reprod. 2002;17:128-33.
- [Google Scholar]
- Role of latent genital tuberculosis in repeated IVF failure in the Indian clinical setting. Gynecol Obstet Invest. 2006;61:223-7.
- [Google Scholar]
- Tuberculosis: Manual for obstetrics and gynaecologists (1st ed). Delhi: Jaypee Brothers Medical Publisher (P) Ltd; 2015. p. :155-275.
- Serial interferon-gamma release assays during treatment of active tuberculosis in young adults. BMC Infect Dis. 2010;10:300.
- [Google Scholar]
- Elevated serum cancer antigen 125 levels in advanced abdominal tuberculosis. Med Oncol. 2001;18:289-91.
- [Google Scholar]
- OC14.04: Ultrasound in female genital tuberculosis: A retrospective series. Ultrasound Obstet Gynecol. 2013;42:28.
- [Google Scholar]
- Update: Abdominal tuberculosis - unusual findings on CT. Clin Radiol. 1995;50:223-8.
- [Google Scholar]
- Magnetic resonance imaging findings among women with tubercular tubo-ovarian masses. Int J Gynaecol Obstet. 2011;113:76-80.
- [Google Scholar]
- Comparison of PET/CT with other imaging modalities in women with genital tuberculosis. Int J Gynaecol Obstet. 2012;118:123-8.
- [Google Scholar]
- Peritoneal tuberculosis revealed by carcinomatosis on CT scan and uptake at FDG-PET. BJOG. 2003;110:1129-31.
- [Google Scholar]
- Hysterosalpingographic findings in infertile women with genital tuberculosis. Int J Gynaecol Obstet. 2008;101:150-5.
- [Google Scholar]
- Hysterosalpingography and ultrasonography findings of female genital tuberculosis. Diagn Interv Radiol. 2015;21:10-5.
- [Google Scholar]
- Hysterosalpingographic appearances of female genital tract tuberculosis: Part II: Uterus. Int J Fertil Steril. 2014;8:13-20.
- [Google Scholar]
- Histopathologic analysis of female genital tuberculosis: A fifteen-year retrospective study of 110 cases in Eastern India. Turk J Pathol. 2013;29:41-5.
- [Google Scholar]
- Evaluating PCR, culture & histopathology in the diagnosis of female genital tuberculosis. Indian J Med Res. 2011;134:40-6.
- [Google Scholar]
- Role of newer methods of diagnosing genital tuberculosis in infertile women. Indian J Pathol Microbiol. 2013;56:155-7.
- [Google Scholar]
- Improved diagnostic value of PCR in the diagnosis of female genital tuberculosis leading to infertility. J Med Microbiol. 2005;54:927-31.
- [Google Scholar]
- Endometrial tuberculosis among patients undergoing endometrial biopsy at Tikur Anbesa specialized hospital, Addis Ababa, Ethiopia. BMC Infect Dis. 2018;18:304.
- [Google Scholar]
- Is PCR a useful tool for the diagnosis of tuberculosis in 1995? Tubercl Lung Dis. 1995;76:183-4.
- [Google Scholar]
- Utility of reverse transcriptase PCR and DNA-PCR in the diagnosis of female genital tuberculosis. J Med Microbiol. 2011;60:486-91.
- [Google Scholar]
- Female genital tuberculosis – a diagnostic and therapeutic challenge. Indian J Tuberc. 2014;61:98-102.
- [Google Scholar]
- Evaluation of xpert MTB/RIF assay performance in diagnosing extrapulmonary tuberculosis among adults in a tertiary care centre in India. Eur Respir J. 2014;44:1090-3.
- [Google Scholar]
- Role of geneXpert in diagnosis of female genital tuberculosis: A preliminary report. Eur J Obstet Gynecol Reprod Biol. 2016;207:237-8.
- [Google Scholar]
- Loop-mediated isothermal amplification assay for detection of Mycobacterium tuberculosis complex in infertile women. Indian J Med Microbiol. 2016;34:322-7.
- [Google Scholar]
- Hysteroscopic findings in women with primary and secondary infertility due to genital tuberculosis. Int J Gynaecol Obstet. 2009;104:49-52.
- [Google Scholar]
- Unusual appearing tubercular deposits at hysteroscopy. J Minim Invasive Gynecol. 2007;14:144.
- [Google Scholar]
- Increased difficulties and complications encountered during hysteroscopy in women with genital tuberculosis. J Minim Invasive Gynecol. 2011;18:660-5.
- [Google Scholar]
- Laparoscopic findings in female genital tuberculosis. Arch Gynecol Obstet. 2008;278:359-64.
- [Google Scholar]
- Genital tuberculosis in infertile women: Assessment of endometrial TB PCR results with laparoscopic and hysteroscopic features. J Obstet Gynaecol India. 2011;61:301-6.
- [Google Scholar]
- Sharma's python sign: A new tubal sign in female genital tuberculosis. J Lab Physicians. 2016;8:120-2.
- [Google Scholar]
- Sharma's kissing fallopian tubes sign: A new tubal sign in female genital tuberculosis. J Obstet Gynaecol India. 2017;67:227-9.
- [Google Scholar]
- Sharma's dried tree branch fallopian tubes sign: A new laparoscopic sign in female genital tuberculosis with infertility. IVF Lite. 2016;3:98-103.
- [Google Scholar]
- Increased complication rates associated with laparoscopic surgery among patients with genital tuberculosis. Int J Gynaecol Obstet. 2010;109:242-4.
- [Google Scholar]
- Ministry of Health and Family Welfare, Government of India and World Health Organization. In: INDEX TB guidelines: Guidelines on extra-pulmonary tuberculosis for India. New Delhi: MoHFW; 2016.
- [Google Scholar]
- Indian Scientists Developing Diagnostic Algorithm for Female Genital TB. The Hans India. Available from: http:// www.thehansindia.com/posts/index/2014-09-21/Indianscientists- developing-diagnostic-algorithm-for-female-genital- TB-108475
- [Google Scholar]
- Prospective analysis of short course chemotherapy in female genital tuberculosis. Int J Gynaecol Obstet. 1992;38:311-4.
- [Google Scholar]
- Six months versus nine months anti-tuberculous therapy for female genital tuberculosis: A randomized controlled trial. Eur J Obstet Gynecol Reprod Biol. 2016;203:264-73.
- [Google Scholar]
- Surgical complications during laparotomy in patients with abdominopelvic tuberculosis. Int J Gynaecol Obstet. 2010;110:157-8.
- [Google Scholar]
- Increased complication rates in vaginal hysterectomy in genital tuberculosis. Arch Gynecol Obstet. 2011;283:831-5.
- [Google Scholar]
- American Thoracic Society, Centers for Disease Control and Prevention, Infectious Diseases Society of America. American Thoracic Society/Centers for Disease Control and Prevention/ Infectious Diseases Society of America: Controlling tuberculosis in the United States. Am J Respir Crit Care Med. 2005;172:1169-227.
- [Google Scholar]
- Comparative study of laparoscopic abdominopelvic and fallopian tube findings before and after antitubercular therapy in female genital tuberculosis with infertility. J Minim Invasive Gynecol. 2016;23:215-22.
- [Google Scholar]
- Second-look hysteroscopy after antitubercular treatment in infertile women with genital tuberculosis undergoing in vitro fertilization. Int J Gynaecol Obstet. 2010;108:128-31.
- [Google Scholar]
- Effect of antitubercular therapy on endometrial function in infertile women with female genital tuberculosis. Infect Disord Drug Targets. 2016;16:101-8.
- [Google Scholar]
- Genital tuberculosis - A major pelvic factor causing infertility in Indian women. Fertil Steril. 1997;67:497-500.
- [Google Scholar]
- Favorable infertility outcomes following anti-tubercular treatment prescribed on the sole basis of a positive polymerase chain reaction test for endometrial tuberculosis. Hum Reprod. 2012;27:1368-74.
- [Google Scholar]
- IVF and tuberculosis. In: Mukherjee GG, Tripathy SN, Tripathy SN, eds. Genital tuberculosis (1st ed). Delhi: Jaypee Brothers Medical Publishers (P) Ltd; 2010. p. :135-40.
- [Google Scholar]
- Current progress in obstetrics and gynaecology. Vol 4. (1st ed). True-Life India: Mumbai; 2017. p. :205-28. Genital tuberculosis and infertility in Indian population
- [Google Scholar]
- Gestational surrogacy in gential tuberculosis. In: Mukherjee GG, Tripathy SN, Tripathy SN, eds. Gential tuberculosis (1st ed). Delhi: Jaypee Brothers Medical Publishers (P) Ltd; 2010. p. :141-54.
- [Google Scholar]
- Perinatal outcome in pregnancies complicated by pulmonary tuberculosis. Int J Gynaecol Obstet. 1994;44:119-24.
- [Google Scholar]
- Obstetrical outcomes among women with extrapulmonary tuberculosis. N Engl J Med. 1999;341:645-9.
- [Google Scholar]
- Tuberculosis and pregnancy - results of a study in a high prevalence area in London. Eur J Obstet Gynecol Reprod Biol. 2006;126:48-55.
- [Google Scholar]
- World Health Organization. Rapid Communication: Key Changes to Treatment of Multidrug-and Rifampicin - Resistant Tuberculosis (MDR/RR-TB), WHO/CDS/TB/2018.18. Geneva: WHO; 2018.
- [Google Scholar]
- World Health Organization. WHO Consolidated Guidelines on Drug-resistant Tuberculosis Treatment. Geneva: WHO; 2019.






