Translate this page into:
Fanconi's anaemia & Laron syndrome: An enigma
*For correspondence: rajkashyapmd@gmail.com
-
Received: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
A 12 yr old female child† presented to the Hematology outpatient department, Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow, India, in September 2018 with anaemia requiring frequent blood transfusions. Haemogram showed pancytopaenia. Bone marrow biopsy and aspiration were performed which revealed a hypoplastic marrow (Figure A). Chromosomal breakage analysis was negative. Next-generation sequencing for Fanconi's anaemia (FA) genetic mutations showed a heterozygous 3' splice site variation in intron 13 of FANCA gene.
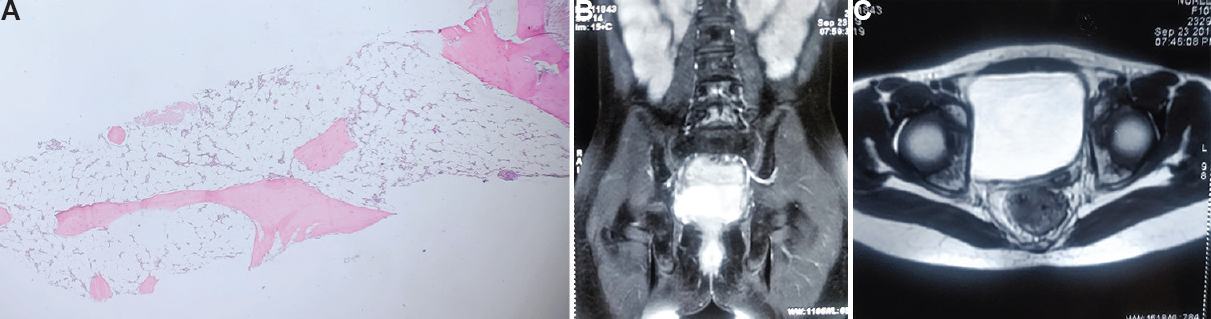
- (A) Photomicrograph of the bone marrow biopsy (H and E stain, ×10) showing hypocelluar marrow with empty marrow spaces and overall cellularity of less than 5 per cent. (B) Bone marrow biopsy showing marked hypocellularity and marrow spaces replaced by fatty tissue. (C) Magnetic resonance images showing marked hypoplasia of the uterus in the transverse and cross sections.
Ultrasonogram and magnetic resonance imaging of the abdomen and pelvis (Figure B and C) revealed a hypoplastic uterus for her age measuring 2.9 × 0.8 cm. In view of her short stature with delayed organ growth, tests for endocrine function were performed. The growth hormone (GH) levels were elevated while insulin-like growth factor-1 levels were low suggestive of primary GH insensitivity. A diagnosis of Fanconi's anaemia (FA) with Laron syndrome was made. She was managed with androgen therapy for the FA and was being followed by paediatric endocrinologists for further management. On one year follow up, she was off transfusions and maintained a haemoglobin level of more than 8 g/dl.
Co-existence of these two conditions is a rare phenomena because while FA is associated with a marked increase in risk of malignancies, Laron syndrome is associated with a reduced risk. In All patients of FA, GH levels should be estimated at baseline and a thorough endocrine workup must be done.
Acknowledgments:
Authors acknowledge Dr Muniba Alim, department of Hematology, SGPGIMS for assisting in clinical workup and diagnosis of this case.
Conflicts of Interest: None.





