Translate this page into:
Experiences of Indian Council of Medical Research with tick-borne zoonotic infections: Kyasanur Forest disease & Crimean-Congo haemorrhagic fever in India with One Health focus
For correspondence: Dr Devendra T. Mourya, ICMR-Chair for Virology and Zoonoses, ICMR-National Institute of Virology, Sus-Pashan Road, Pune 411 021, Maharashtra, India e-mail: dtmourya@gmail.com
-
Received: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Emergence and re-emergence of several pathogens have been witnessed by this century in the form of outbreaks, epidemics and pandemics. In India, the influencing factor that promotes dissemination of emerging and re-emerging viral infections is the biogeographical zones: a megadiverse country, characterized by varied geographical, climatic conditions and ever-changing socio-economical and geopolitical issues. These influence the movement of humans and animals and add layers of complexity for the identification and timely management of infectious diseases. This review focuses on two tick-borne infections: Crimean-Congo haemorrhagic fever (CCHF) and Kyasanur forest disease (KFD). In the last two decades, these viruses have emerged and caused outbreaks in different parts of India. KFD virus was initially identified in 1957 and was known to be endemic in Karnataka State while CCHF virus was first identified during 2010 in Gujarat State, India. These viruses have managed to emerge in new areas within the last decade. With changing epidemiology of these arboviruses, there is a probability of the emergence of these viruses from new areas in future. The investigations on these two diseases under the One Health focus involved early detection, quickly developing diagnostic tools, identifying stakeholders, capacity building by developing collaboration with major stakeholders to understand the epidemiology and geographical spread in domestic animal reservoirs and tick vectors in the affected areas, developing laboratory network, providing diagnostic reagents and biosafety and laboratory diagnosis training to the network laboratories to control these diseases.
Keywords
Crimean-Congo haemorrhagic fever
India
Kyasanur forest disease
one heath
tick-borne
zoonotic disease
Emergence and re-emergence of zoonotic diseases is a major health problem. The latest was SARS-CoV-2 in December 2019, crossing species to infect humans. The concept of One Health deals with the interdependence of human, animal and environmental health. This review is to express experiences dealing with two emerging zoonotic infections viz. Crimean-Congo haemorrhagic fever (CCHF) and Kyasanur forest disease (KFD) in the country. It defines how collaboration, coordination and commitment of relevant principal stakeholders are sought for joint efforts to build laboratory capacity and developing laboratory networks for quick diagnosis to assess the impact of these diseases in the affected areas. The training and coordination has helped to minimize the impact of these diseases on human health. Particularly, various biorisk mitigation trainings helped in prevention of secondary cases and containing the outbreaks of the highly infectious risk group-4 pathogen. This review shares the experiences working with these two emerging zoonotic infectious diseases, focusing on One Health.
Appropriate infrastructure to deal with emerging zoonotic infections
The National Institute of Virology (ICMR-NIV), Pune, is one of the premier institutes of the Indian Council of Medical Research (ICMR), New Delhi. The mission of the institute is to carryout high calibre research in the areas of diagnostics, epidemiology, molecular biology and immunological aspects of the viruses of public health importance. Cutting edge Biosafety level (BSL)-3 and -4 facility is available with the mandate to investigate outbreaks caused by emerging and re-emerging viral infections. The establishment of the state-of-the-art laboratory provided improved zoonotic disease identification, response capacity and prevention. This institute does not only serve the country but also caters to the needs of neighbouring South-East Asian Region (SEAR) countries for laboratory capacity building for preparedness of dealing with unusual outbreaks and epidemic. The ICMR-NIV is recognized as the World Health Organization (WHO) Regional Collaborating Centre for Reference and Research on Arboviruses, Influenza and Measles as well as National Reference Centre for Polio, Hepatitis, Avian Influenza and emerging infectious diseases. This institute is a designated Polio Essential Facility under the Ministry of Health and Family Welfare, Government of India, for storage of the virus isolates of eradicated wild type and attenuated vaccine strains of poliovirus in the country. It is also a resource centre for providing training related to virological diseases for their detection and diagnosis as well as control with the back-up of Virus Research and Diagnostic Laboratories (VRDL) network and State Integrated Disease Surveillance Programme (IDSP) network in the country.
Kyasanur forest disease
Kyasanur forest disease (KFD) virus was discovered in 19571. It belongs to the tick-borne encephalitis virus sero-complex, genus Flavivirus and family Flaviviridae1. Extensive work was carried out during the 1960s and 1970s to explore the natural cycle, transmission cycle, host-vector biology and disease seasonality. Initial investigations showed the prevalence of this disease only in five districts of Karnataka State (Shimoga, Chikamagalur, Uttara Kannada, Dakshina Kannada and Udupi) with average cases of about 400 to 500/year2. Indigenous KFD vaccine was also developed in the 1960s. The National Institutes of Health/Centers for Disease Control and Prevention, USA, established the biosafety concept in 1960s3. But during 1957-1970, more than 100 researchers got infected while working on KFD in the laboratory and field, hence the work on the KFD virus was completely stopped in ICMR-NIV due to a lack of containment facility and proper and adequate personal protective gears4.
National collaboration with stakeholder on the investigation of KFD
After the establishment of BSL-3 laboratory in ICMR-NIV in 2005, work on this virus was resumed. Quickly the time-sensitive and cost-effective molecular and serological assays were developed for KFD virus (KFDV) identification, including nested RT-PCR, real-time RT-PCR and IgM and IgG ELISA5. The ICMR identified Karnataka Health department as the main stakeholder and provided support for the on-time screening of human, monkey and tick samples. Coordination with health services of various States and public health laboratories with the availability of better laboratory diagnostic tests led to the identification of newer areas affected by KFDV from Western Ghats of India (Kerala, Tamil Nadu, Goa and Maharashtra States)6. With expanding laboratory network from 2012 in southern States, the prevalence of KFD was identified in further new areas (Bandipur National Park), with monkey deaths and human cases from Chamarajanagar district, Karnataka State (2012); Mudumalai Tiger Reserve, Tamil Nadu State (2012)78. In 2014, a massive KFDV outbreak was reported from Thirthahalli taluk, Shimoga District, Karnataka State, India. Monkey and tick pools were also tested positive for KFDV9. Soon after confirmation of this outbreak, necessary preventive measures were taken by the Karnataka State Health authorities10. In May 2014, an outbreak of KFDV was confirmed in the tribal population of Nilambur, Malappuram district, Kerala, bordering the Nilgiri district of Tamil Nadu. The outbreak investigation in the affected areas showed febrile illness and KFD positivity in the tribal population11. In 2015, retrospective screening of the acute febrile illness cases showed the presence of anti-KFD IgG antibody among the human population of Wayanad (7.1%) and Palakkad district (33.9%) (ICMR-NIV unpublished data). In 2016, an outbreak of KFD was jointly investigated by the ICMR-NIV and State Health Department, Dodamarg taluka, Sindhudurg district, Maharashtra State. Higher KFDV positivity (22.8%) with 2.3 per cent case fatality rate (CFR) was recorded during this outbreak12. This was the first report of the KFD outbreak from Maharashtra State. Based on this, the health services, Government of Maharashtra took policy decision regarding KFD vaccination for those who were at high-risk covering health workers and forest workers12. During 2016, outbreak investigations in Belgaum district, Karnataka showed that cashew nut harvesting workers contracted the KFD infections while working in Sattari taluk, Goa. This further confirmed that certain occupations like farming, collecting the dried leaves and wood as well as grazing animals in the forest were the major risk factors for tick-bite and thereby acquiring the infection13. In 2017, the outbreak of KFD was confirmed from the Banda taluka of Sindhudurga district, Maharashtra with the highest recorded CFR of 12.3 per cent (ICMR-NIV unpublished data). With its widespread prevalence along the Western Ghats, KFD emerged as a disease of public health importance in India. Till 2021, human cases, monkey and tick pool positivity have been detected from all the five affected States of the country (ICMR-NIV unpublished data).
Phylogeography of KFD virus in India
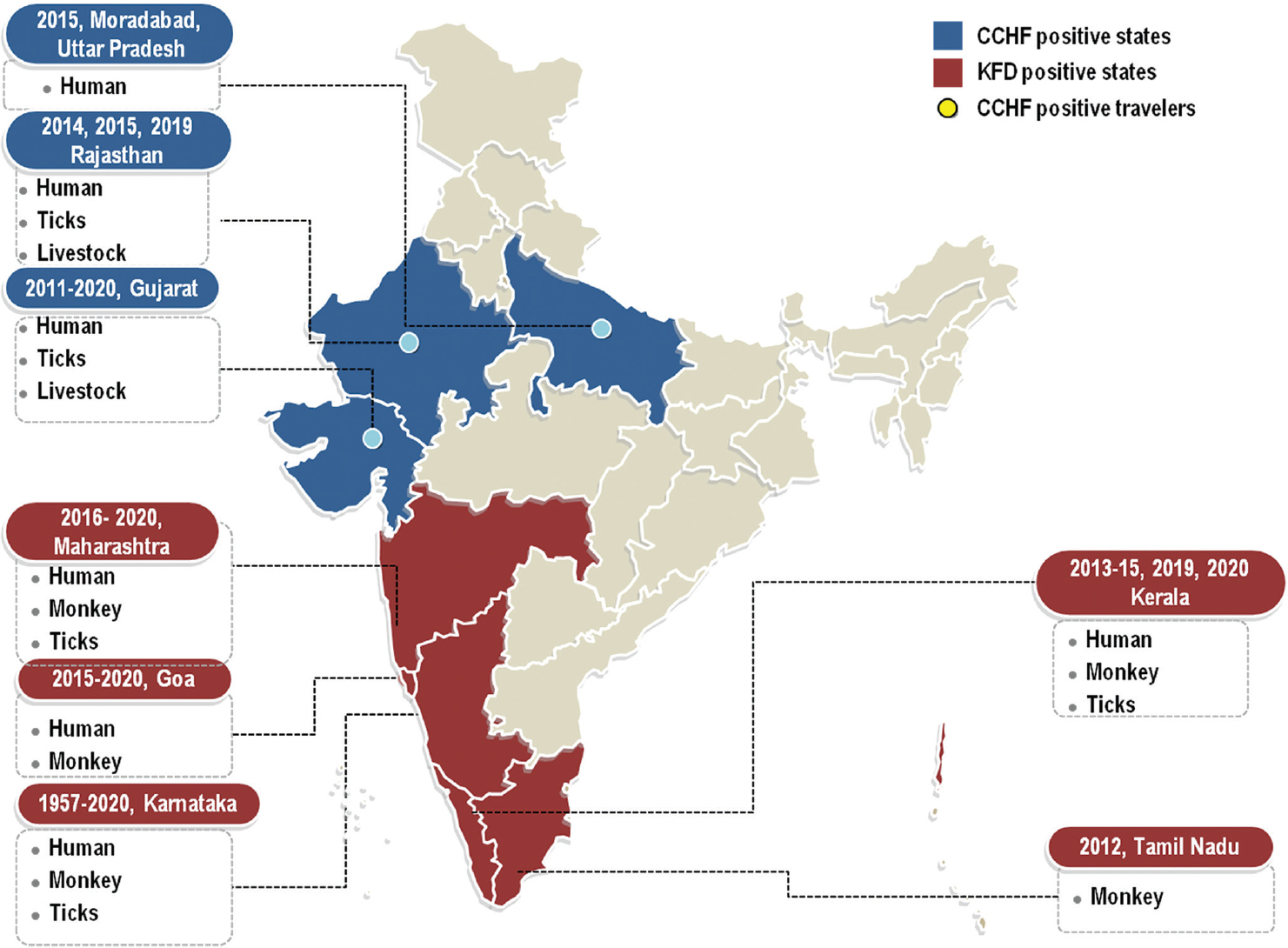
During 1957–2017, several strains of the KFD virus were isolated from humans, ticks and monkeys. The KFD vaccine was prepared in the Virus Research Laboratory, Karnataka, with the collaboration of ICMR-NIV, Pune. The prototype strain isolated in 1957 was used for vaccine preparation. The emergence of KFD in many other States other than Karnataka raised the issue of the possibility of strain variation during the last 5-6 decades14. Therefore, a study was undertaken on phylogeography analysis of 48 whole genomes and additionally 28 E gene sequences of KFDV isolated from different regions spanning the period 1957–2017 that revealed that mean evolutionary rates based on the E gene were marginally higher than that based on the whole genomes14. A subgroup of KFDV strains representing earlier and the recent isolates of duration 2006–2017 differing from the early strains from Karnataka isolated during 1957–1972 by about2.76 per cent at their whole-genome level. This could be the reason for the spread of KFD to different geographical areas that were genetically diverged around 198014. Maximum nucleotide difference between the two groups was noted in the capsid gene (3.27%), followed by the E gene (3.22%) and NS2 gene (2.91%). The highest per cent amino acid differences between the two groups were noted in the capsid protein (3.17%), followed by the prM (1.66%), and NS2 (1.4%) proteins14. The study indicated dispersal of the virus from Karnataka to Goa and Maharashtra while Maharashtra strain represented a new source for transmission of KFDV since 2013. The findings indicated the need to curtail the spread of KFDV by surveillance measures and improved vaccination strategies14 India where the disease was first identified and in Tamil Nadu, Maharashtra, Kerala, and Goa covering the Western Ghats region of India. The incidence of positive cases and distribution of the KFDV. The Fig. 1 depicts the States affected by KFDV.
Crimean-Congo haemorrhagic fever (CCHF)
Identification of major stakeholders and national collaboration on outbreak investigation
In 2011, the presence of CCHF virus was confirmed for the first time during a nosocomial outbreak in a tertiary care hospital in Ahmadabad, Gujarat15. With evidence-based surveillance and collaboration with Gujarat State Health Authorities, the investigations revealed the circulation of Tajikistan strain of CCHF virus in this outbreak15. After the first outbreak, the Department of Animal Husbandry, Gujarat government was identified as the main stakeholder and screening of livestock and tick pools was initiated. The team of Integrated Disease Surveillance Programme (IDSP), Gujarat, worked in collaboration with ICMR-NIV, Pune to confirm the epidemiological linking of the CCHF cases. This set-up led to the investigation of another dreadful outbreak of CCHF in 2013, in Karyana village, Amreli district, Gujarat16. This outbreak investigation showed the cause of secondary cases among the close contacts who were performing the last rituals of the CCHF case. This outbreak made a huge impact on public health, hence, the State government in consultation with ICMR decided for the procedure for safe last rituals of the suspected and confirmed cases by the health authorities. The CCHF clinical management guidelines 2013 were formulated in collaboration with IDSP, Emergency Medical Relief (EMR), National Centre for Disease Control (NCDC) and ICMR-NIV, Pune (guidelines not available in public domain).
The establishment of state-of-the-art containment BSL-4 facility at ICMR-NIV, Pune in 2012 made it possible to develop indigenous serological assays for diagnosis of IgM and IgG for humans and IgG for the livestock17. Before this, the source of reagents supplied was only the Centers for Disease Control and Prevention, USA. These indigenous technologies not only helped in the timely diagnosis of suspected CCHF cases; but also rendered a help in surveillance of CCHF in human, livestock, and ticks in the country.
The Gujarat State and Central Health Authorities initiated a survey of antibodies in domestic animals (bovine, sheep, and goat), which revealed a high proportion of animal population positive for anti-CCHF IgG antibodies from 15 districts of Gujarat17. The high prevalence of this virus in Gujarat during 2011-2014 caused almost 34 CCHF cases and 16 deaths1516. In 2014, samples from a suspected viral haemorrhagic fever (VHF) case from Veravilapur village, Sirohi District, Rajasthan was confirmed to be CCHF positive. This was the first outbreak of CCHF in Rajasthan, which raised the question of whether the CCHF virus has spread to Rajasthan State or it already existed but was not detected before18.
Following the first confirmed CCHF case from Rajasthan, a nosocomial outbreak was reported from Jodhpur in January 201519. After this episode, a three-member medical team from the State ministry visited the hospital and on their recommendations, contact tracing was initiated, and a total of five cases were confirmed. Data on the genetic analysis suggested the CCHF viral strain responsible for this outbreak to be new which could be a recent introduction from the neighbouring countries19.
To understand its prevalence in the rest of the country, the main stakeholder, Indian Council of Agricultural Research (ICAR) was identified and with their help the countrywide survey of CCHF antibodies was carried out with samples from bovine, sheep and goats from 22 States and one Union Territory of India within two years. The results showed the prevalence of this antibody in all these areas20. Many sporadic CCHF cases and focal outbreaks were reported from Gujarat during 2015-2018 (ICMR-NIV unpublished data). In 2016, an Indian migrant worker who returned from Muskat, Oman to Kutch, Gujarat was confirmed as an imported CCHF case21. Phylogenetic analysis revealed that this imported strain belonged to the Asia-1 IV group, along with strains of CCHFV from Oman, Afghanistan, Pakistan and Iran20.
Another imported CCHF case with a travel history from Dubai, the United Arab Emirates to Thrissur, Kerala, was confirmed in December 2019. The high vigilance of the airport authority and public health system in India with the strengthened laboratory network helped in identifying, isolating and management of this case (ICMR-NIV unpublished data). During 2019, maximum numbers of CCHF cases were detected in India from Gujarat and Rajasthan States with a 50 per cent CFR (ICMR-NIV unpublished data). Considering the higher number of secondary cases in this outbreak, the CCHF clinical management guidelines 2013 were modified. The enhanced network of the surveillance system under IDSP helped in the detection of CCHF cases in the country. From 2011 to 2020, a total of 125 CCHF cases were confirmed with 53 deaths (CFR-42.40%) (ICMR-NIV unpublished data).
Figure 1 depicts the States affected by CCHF virus including the imported cases, and Figure 2 emphasizes the concept of the One Health approach needed for zoonotic diseases control and prevention in India.
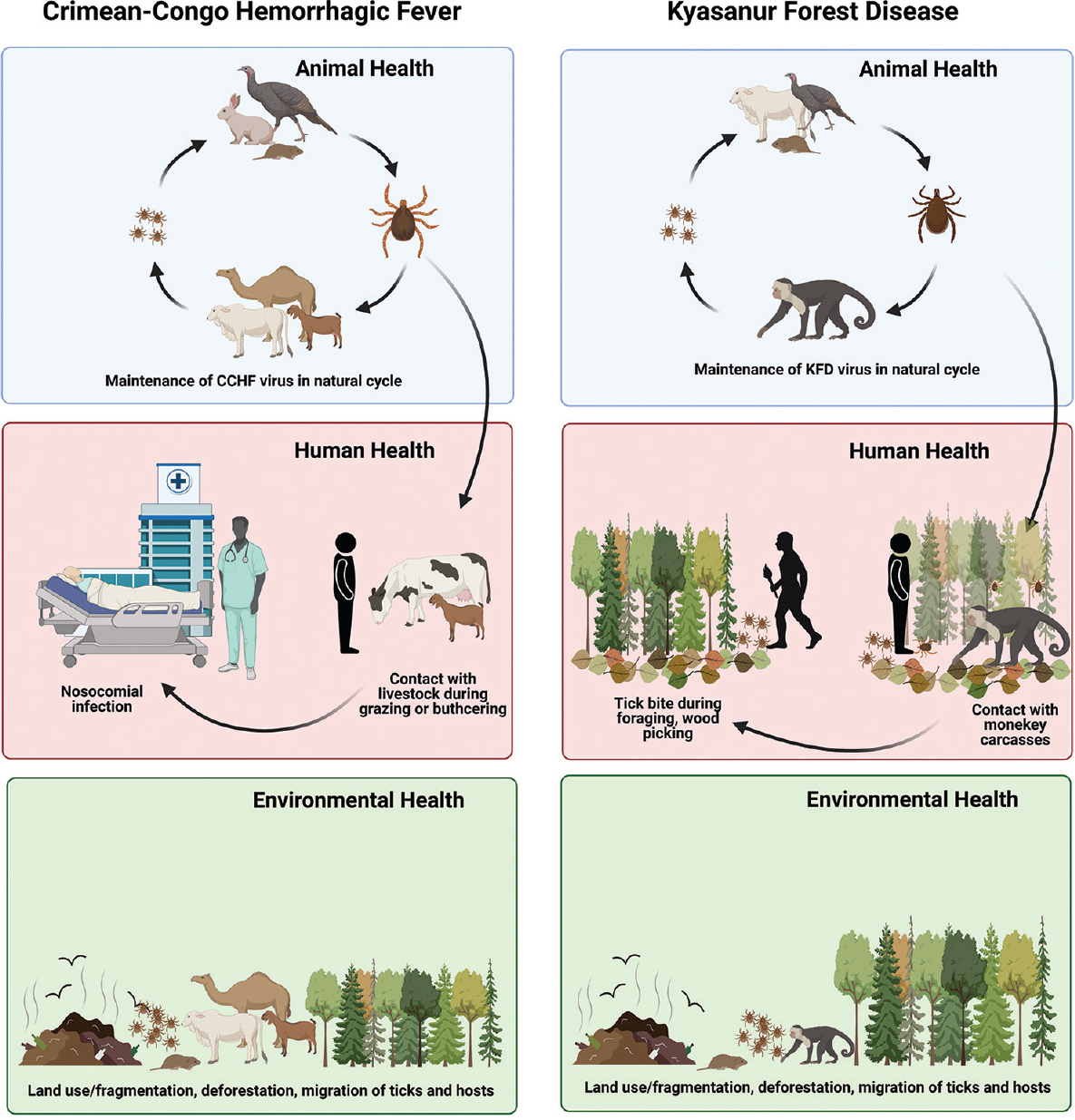
- Concept of One Health: Prevention and control of CCHF and KFD based on a multidimensional approach including human, animal and environmental factors. Source: Created by BioRender.com.
International cooperation and human resource development
With the help of the Ministry of Health and Family Welfare, Government of India, international collaboration with CDC, USA was established under Global Health Security Agenda, USA, for enhancing laboratory capacity for quick detection and identification of newly emerging infections22. This programme also helped in establishing a specific network for Viral Haemorrhagic Fever (VHF) laboratories in India22.
The ICMR has also extended its training support to SEAR countries including Bhutan, Sri Lanka, Myanmar, Bangladesh, Indonesia, Nepal, Maldives and Thailand in many bilateral programmes. The training and sensitization workshops included in-depth details on biosafety, biosecurity, and management of the biorisk programmes while working in the BSL-2 and BSL-3 laboratory. Similarly, with the support of WHO, various trainings were conducted for the network of laboratories for a regulatory framework for sample collection, packaging and transportation as per International Air Transport Association (IATA) along with biomedical waste management dealing with a high-risk group of pathogens. This also included simulation exercises to provide glimpses and real scenarios of the outbreak containment and response for these laboratories network (NIV unpublished data).
The ICMR-NIV, Pune, provided the expertise for the establishment of the BSL-3 level laboratories in the country. In-depth trainings on the validation of the facility and laboratory equipment, risk assessment while working with high-risk pathogens were also undertaken. Hands-on trainings included biosafety aspects while handling suspected zoonotic infection samples, working with biosafety cabinets, management of spills, handling sharps, etc.
Quality assurance in laboratory testing for better surveillance & preparedness
The ICMR-NIV, Pune, established laboratory quality system for the CCHF and KFD diagnosis and National Accreditation Board for Testing and Calibration Laboratories (NABL) (ISO/IEC 17025:2005) was implemented to provide the quality and technical competence of CCHF and KFD molecular and serological diagnostic tests. Strict adherence to internal quality assurance, surveillance audit and assessment is followed. The diagnostic algorithms for KFD and CCHF are provided in Fig. 3. The Department of Health Research (DHR), Ministry of Health and Family Welfare, Government of India established a network of VRDL laboratories across the country to create infrastructure for timely identification of viruses causing outbreaks or related to significant morbidity/mortality, which are significant at a public health level. This has also helped IDSP, India in surveillance data23.
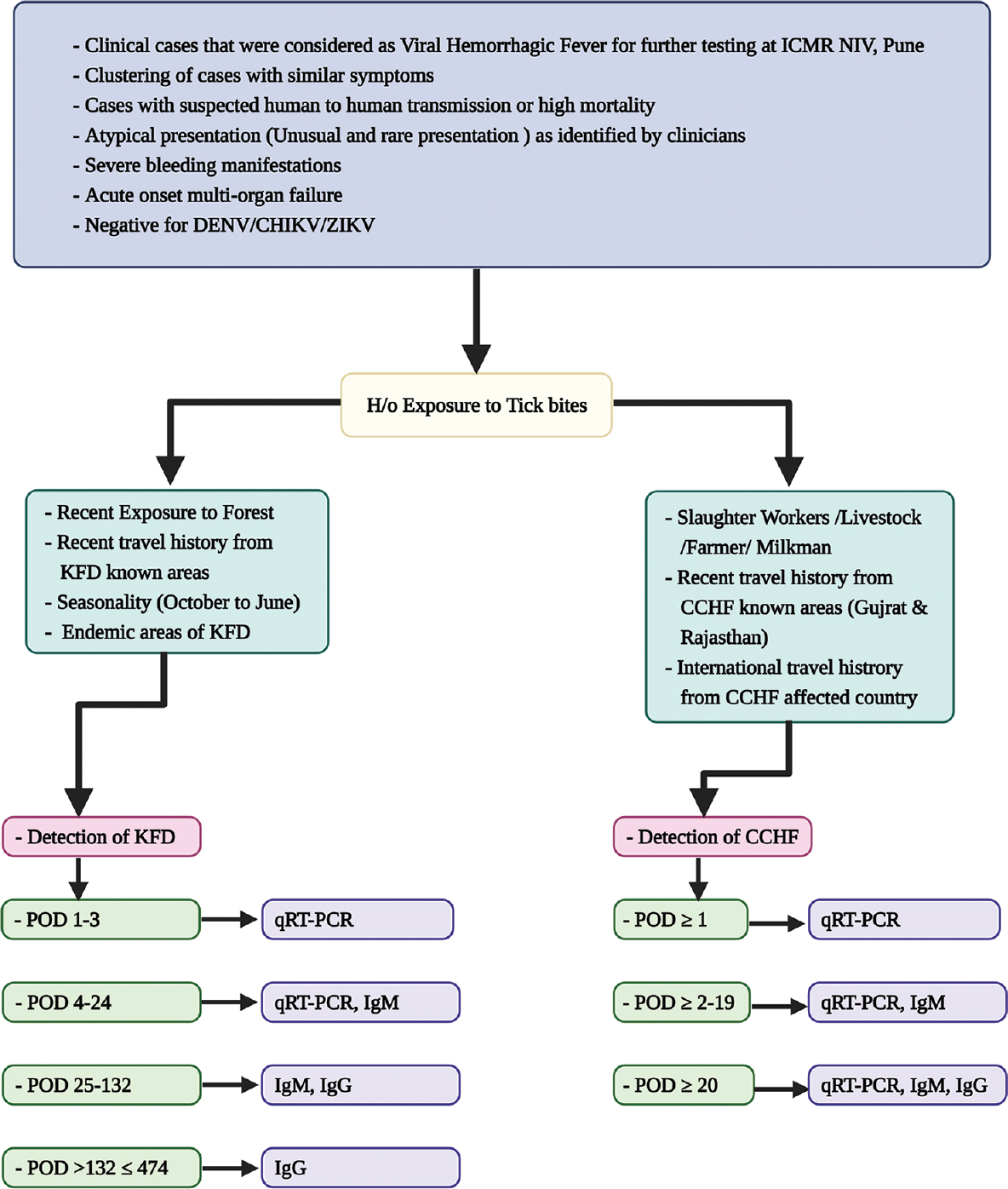
- Diagnostic algorithm for the detection and screening of CCHF and KFDV cases. Source: Refs 16, 21 and NIV unpublished data; figure created by BioRender.com.
Policy and collaborative programme development
The ICMR-NIV, Pune, has signed a Memorandum of Understanding (MoU) in 2012 with Karnataka State Government to help them in setting up the diagnosis of KFD in the State. Not only the hands-on training for KFDV diagnosis was conducted for Virus Diagnostic Laboratory (VDL), Shimoga, but also technical support was provided to build a diagnostic facility.
The morbidity and mortality caused by KFDV (monkey fever) disease in the country had made the policymakers and researchers to realize the importance of the establishment of the containment facility and appropriate biosafety measures for handling such high-risk pathogens. The advent of these technologies has helped in applying control and preventive measures for this disease. Considering the potential risk of CCHF in India and the threat of imports via international travellers and animal trading, different guidelines were prepared for case identification, diagnosis, quarantine policies, and contact tracing24.
Conclusions
Since there are no vaccines or effective antiviral drugs available for the treatment of CCHF, the treatment is solely supportive and current prevention strategies focus on creating awareness in affected areas25. CCHF is also listed in the WHO Research & Development (R&D) Blueprint list of epidemic threats needing urgent R&D action26. Though the vaccine for KFD is available, there are questions related to its immunogenicity6. With the unavailability of antiviral drugs, KFD cases are managed with supportive therapy6. Strategic vaccination drive in KFD affected areas and adjoining regions is a requirement for restricting the spread of this disease6.
There is a need to increase awareness of emerging zoonotic infections, enhancing laboratory capacities and organizing various levels of training programmes under the One Health programme from a public health point of view. Being adequately prepared to detect, manage and respond to emerging outbreaks of infectious diseases is important. The active surveillance of vector, reservoir and human population can provide significant information about the virus activity in affected and adjoining areas. This will be useful both for measuring the need for interventions and for assessing the effects of interventions. This will also help in efficiently developing emergency preparedness of the public health system in India to tackle emerging infections. Different approaches of Next Generation Sequencing have been established for an in-depth understanding of emerging infections27. This will provide the backbone for preparedness for prediction, detection and mitigation of emerging zoonotic infections.
Acknowledgment:
Authors acknowledge the encouragement and support extended by Prof. (Dr.) Balram Bhargava, Secretary to the Government of India, Department of Health Research, Ministry of Health & Family Welfare & Director-General, ICMR, New Delhi. Authors also express the gratitude towards Drs N. K. Ganguli, V. M. Katoch, and Soumya Swaminathan, Former Director Generals, ICMR for promoting and taking further One Health concept. The authors also express gratitude to all the earlier Directors of ICMR-NIV, Pune and dedicated scientists and technical staff for their support and dedicated services during these investigations of emerging viral diseases.
Financial support & sponsorship: None.
Conflicts of Interest: None.
References
- Emerging/re-emerging viral diseases & new viruses on the Indian horizon. Indian J Med Res. 2019;149:447-67.
- [Google Scholar]
- Kyasanur forest disease: an epidemiological view in India. Rev Med Virol. 2006;16:151-65.
- [Google Scholar]
- A new approach to clean room design. Technical Report No. SC-4673 (RR). Albuquerque, New Mexico: Sandia Corp; 1962.
- Highly infectious tick-borne viral diseases: Kyasanur forest disease and Crimean–Congo haemorrhagic fever in India. WHO South East Asia J Public Health. 2014;3:8-21.
- [Google Scholar]
- Diagnosis of Kyasanur forest disease by nested RT-PCR, real-time RT-PCR and IgM capture ELISA. J Virol Methods. 2012;186:49-54.
- [Google Scholar]
- Clinical & epidemiological significance of Kyasanur forest disease. Indian J Med Res. 2018;148:145-50.
- [Google Scholar]
- On the transmission pattern of Kyasanur Forest disease (KFD) in India. Infect Dis Poverty. 2015;4:37.
- [Google Scholar]
- Spread of Kyasanur Forest Disease, Bandipur Tiger Reserve, India, 2012–2013. Emerg Infect Dis. 2013;19:1540-1.
- [Google Scholar]
- Outbreak of Kyasanur Forest disease in Thirthahalli, Karnataka, India, 2014. Int J Infect Dis. 2014;26:132-4.
- [Google Scholar]
- Kyasanur Forest disease outbreak and vaccination strategy, Shimoga District, India, 2013-2014. Emerg Infect Dis. 2015;21:146-9.
- [Google Scholar]
- New focus of Kyasanur Forest disease virus activity in a tribal area in Kerala, India, 2014. Infect Dis Poverty. 2015;4:12.
- [Google Scholar]
- Kyasanur Forest disease prevalence in Western Ghats proven and confirmed by recent outbreak in Maharashtra, India, 2016. Vector Borne Zoonotic Dis. 2018;18:164-72.
- [Google Scholar]
- Occupational exposure of cashew nut workers to Kyasanur Forest disease in Goa, India. Int J Infect Dis. 2017;61:67-9.
- [Google Scholar]
- Phylogeography of Kyasanur forest disease virus in India (1957-2017) reveals evolution and spread in the Western Ghats region. Sci Rep. 2020;10:1966.
- [Google Scholar]
- Detection, isolation and confirmation of Crimean-Congo hemorrhagic fever virus in human, ticks and animals in Ahmadabad, India, 2010-2011. PLoS Negl Trop Dis. 2012;6:e1653.
- [Google Scholar]
- Emergence of Crimean-Congo hemorrhagic fever in Amreli District of Gujarat State, India, June to July 2013. Int J Infect Dis. 2014;18:97-100.
- [Google Scholar]
- Serosurvey of Crimean-Congo hemorrhagic fever virus in domestic animals, Gujarat, India, 2013. Vector Borne Zoonotic Dis. 2014;14:690-2.
- [Google Scholar]
- First confirmed case of Crimean-Congo haemorrhagic fever from Sirohi district in Rajasthan State, India. Indian J Med Res. 2015;142:489-91.
- [Google Scholar]
- Nosocomial infection of CCHF among health care workers in Rajasthan, India. BMC Infect Dis. 2016;16:624.
- [Google Scholar]
- Cross-sectional serosurvey of Crimean-Congo hemorrhagic fever virus IgG in livestock, India, 2013–2014. Emerg Infect Dis. 2015;21:1837.
- [Google Scholar]
- Crimean-Congo Hemorrhagic Fever in migrant worker returning from Oman to India, 2016. Emerg Infect Dis. 2017;23:1005-8.
- [Google Scholar]
- Centers for Disease Control and Prevention. Division of Global Health Protection: Global health protection and security. Available from https://www.cdc.gov/globalhealth/healthprotection/ghs/index.html
- Department of Health Research, MoHFW, Government of India, New Delhi. Establishment of a network of Laboratories for managing epidemics and Natural Calamities (VRDL). Available from: https://dhr.gov.in/schemes/establishmentnetwork-laboratories-managing-epidemics-and-naturalcalamities
- Second international conference on Crimean-Congo hemorrhagic fever. Antiviral Res. 2018;150:137-47.
- [Google Scholar]
- Identification of the crucial parameters regarding the efficacy of ribavirin therapy in Crimean-Congo haemorrhagic fever (CCHF) patients: a systematic review and meta-analysis. J Antimicrob Chemother. 2019;74:3432-9.
- [Google Scholar]
- Prioritizing diseases for research and development in emergency contexts. Available from: https://www.who.int/activities/prioritizing-diseases-for-research-and-development-in-emergency-contexts
- Complete genome sequencing of Kaisodi virus isolated from ticks in India belonging to Phlebovirus genus, family Phenuiviridae. Ticks Tick-Borne Dis. 2019;10:23-33.
- [Google Scholar]