Translate this page into:
Evidence of apoptosis in right ventricular dysfunction in rheumatic mitral valve stenosis
Reprint requests: Dr Shantanu Pande, Department of Cardiovascular & Thoracic Surgery, Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow 226 014, Uttar Pradesh, India e-mail: spande@sgpgi.ac.in
-
Received: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Right ventricular (RV) dysfunction is one of the causes of morbidity and mortality in valvular heart disease. The phenomenon of apoptosis, though rare in cardiac muscle may contribute to loss of its function. Role of apoptosis in RV in patients with rheumatic valvular heart disease is investigated in this study.
Methods:
Patients with rheumatic mitral valve stenosis formed two groups based on RV systolic pressure (RVSP) as RVSP <40 mmHg (group I, n=9) and RVSP ≥40 mmHg (group II, n=30). Patients having atrial septal defect (ASD) with RVSP <40 mmHg served as control (group III, n=15). Myocardial performance index was assessed for RV function. Real-time polymerase chain reaction was performed on muscle biopsy procured from RV to assess expression of pro-apoptotic genes (Bax, cytochrome c, caspase 3 and Fas) and anti-apoptotic genes (Bcl-2). Apoptosis was confirmed by histopathology and terminal deoxynucleotide-transferase-mediated dUTP nick end labelling.
Results:
Group II had significant RV dysfunction compared to group I (P=0.05) while caspase 3 (P=0.01) and cytochrome c (P=0.03) were expressed excessively in group I. When group I was compared to group III (control), though there was no difference in RV function, a highly significant expression of pro-apoptotic genes was observed in group I (Bax, P=0.02, cytochrome c=0.001 and caspase 3=0.01). There was a positive correlation between pro-apoptotic genes. Nuclear degeneration was present conforming to apoptosis in valve disease patients (groups I and II) while it was absent in patients with ASD.
Interpretation & conclusion:
Our findings showed evidence of apoptosis in RV of patients with valvular heart disease. Apoptosis was set early in the course of rheumatic valve disease even with lower RVSP, followed by RV dysfunction; however, expression of pro-apoptotic genes regressed.
Keywords
Apoptosis
mitral valve replacement
rheumatic heart disease
right ventricular dysfunction
Right ventricle (RV) functions predominantly as a volume pump that is resilient to adversities in various disease conditions1. Function of RV depends on its own afterload, function of the left ventricle (LV) and contractility of the myocardium. It is established that the systolic function of RV is preserved even in clinically evident RV dysfunction2. RV dysfunction in mitral stenosis is due to increasing afterload3. Dysfunction of RV is a poor prognostic factor in valvular heart disease4. Moreover, the presence of pulmonary arterial hypertension (PAH) is associated with a poor prognosis, with a median survival of 2.8 years5. PAH develops very slowly and over a long period. Thus, most of the studies on PAH and RV are from animal models6. In our previous study, we identified raised pro-brain natriuretic peptide levels in patients having rheumatic valvular heart disease presenting with low RV systolic pressure (RVSP)7. This observation indicates the presence of RV dysfunction in the subset even before rise of afterload. Reason for this is poorly understood as chronic rheumatic heart disease is not known to cause myocardial damage8. Myocardial apoptosis may be one of the reasons though it is not observed in physiological condition9. Apoptosis is known to appear in myocardial cells during various stresses10 and the presence of raised RVSP may be one of them. This study was performed to observe the evidence of apoptosis in RV in patients of rheumatic valvular heart disease and its association with RV dysfunction.
Material & Methods
The study was conducted in the department of Cardiovascular and Thoracic surgery, Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow, India, between December 2009 and December 2011. The study protocol was approved by the Ethics Committee of the institute, and informed written consent was received from all the patients participating in this study. Consecutive patients with rheumatic valvular heart disease undergoing mitral valve replacement fulfilling inclusion criteria were included. Inclusion criteria required patients to have all the mentioned criteria such as chronic rheumatic heart disease, severe mitral stenosis, normal left ventricular function and normal sinus rhythm with age between 18 and 60 years. Patients were excluded from the study if valve other than mitral was operated, concomitant coronary revascularization was required, atrial fibrillation was present or LV was dilated with ejection fraction (EF) less than 50 per cent. The patients were categorized in two groups based on RVSP: group I with RVSP<40 mmHg (n=9) and group II with RVSP≥40 mmHg (n=30). Patients undergoing operation for correction of atrial septal defect (ASD) with RVSP<40 mmHg (n=15, group III) formed the third group. ASD was included as the RV in this condition involutes to normal geometry and function during adulthood11. RVSP of <40 mmHg in these patients put the similar afterload to RV as observed in valve group with RVSP <40mmHg and without rheumatic valvular heart disease. ASD patients thus served as a control for group I. This was the only available group of patients requiring open-heart surgery with RV closest to normal population. Patients with ASD and RVSP>40 mmHg cannot be used as a control group for rheumatic valve disease with RVSP>40 mmHg as the reason for load on RV will be different in both these situations.
Echocardiography: All measurements were made on transthoracic echocardiography utilizing Philips Envisor HD echo system and a 3.2-MHz transthoracic transducer (Philips Medical Systems, USA) by a single operator to eliminate the bias. Routine echocardiography was performed using prescribed protocol and left ventricular end dimensions in systole and diastole (LVESD and LVEDD), EF of LV and mitral valve morphology were assessed utilizing two-dimensional imaging and Doppler measurements. RVSP was calculated in apical four-chamber view and was considered as representative of pulmonary artery systolic pressure12. RV function was further assessed with the Doppler index of myocardial performance index (MPI) expressed by formula (isovolumic contraction time + isovolumic relaxation time/RV ejection time). It is established that MPI is not affected by the loading condition of RV, but it was ensured that there was no change in heart rate during both measurements as these were done in two different echocardiographic views13. MPI value of >0.40 was considered as RV dysfunction14.
History of medical treatment: Patients with ASD were not on any preoperative medications. However, valve heart disease patients were on tablet digitalis 0.25 mg orally once daily for five days a week and tablet furosemide 40 mg orally once a day. Patients in valve group were of chronic rheumatic heart disease and hence were not on steroids or immunosuppression. There was no medication that could influence appearance of apoptosis.
Procedure of RV biopsy: Patients were operated under general anaesthesia through median sternotomy using cardiopulmonary bypass with aortic and bi-caval canulation. In valve cases, the right atrium was opened obliquely after snaring the vena cavae and RV was entered through tricuspid valve after retracting it. Partial thickness of 1 cm × 1 cm of RV free wall muscle was removed from endocardial surface. During cardiopulmonary bypass, active warming was performed to achieve the temperature between 35 and 36°C and tepid blood antegrade cardioplegia was used after ascending aortic cross-clamp. Mitral valve replacement was done through left atrium using bi-leaflet mechanical prosthesis. In patients operated for ASD repair, aortic cross-clamp was applied and heart was arrested with cold blood cardioplegia delivered through the aortic root. Right atrium was opened and RV biopsy taken as described for valve cases. The operation was completed in standard fashion. RV muscle biopsy was stored in liquid nitrogen at -270°C to be analyzed at a later date. A part of this was preserved for histopathology.
Quantitative reverse transcription-polymerase chain reaction (qRT-PCR): Total RNA was isolated from myocardial tissues using RNeasy Mini kit (Qiagen, Germany) according to the manufacturer's protocol. The RNA was subsequently reverse-transcribed using an oligo(dT) primer and reverse transcriptase (Applied Biosystems, USA). RT-PCR reactions were performed using SYBR Green PCR Master Mix (Applied Biosystems) and 100nM of gene-specific forward and reverse primers. Primers used for the amplification of Human Bax, Bcl2, Cyt c, Fas, caspase-3 and an internal loading control, glyceraldehyde-3-phosphate dehydrogenase (GAPDH) were as follows: Bax, sense 5’-GATGCGTCCACCAAGAAGC-3’ (forward) and 5’-CCAGTTGAAGTTGCCGTCAG-3’ (reverse); Bcl-2, 5’-GATGCGTCCACCAAGAAGC-3’ (forward) and 5’-CCAGTTGAAGTTGCCGTCAG-3’ (reverse); CYC, 5’-TGGGTGATGTTGAGAAAGG-3’(forward) and 5’-CGGCTGTGTAAGAGTATCC-3’(reverse); Fas, 5’-CGTCTGTTGCTAGATTATCG-3’(forward) and 5’-TTGTCTGTGTACTCCTTCC-3’(reverse); Caspase 3, 5’-CTGGACTGTGGCATTGAGAC- 3’(forward) and 5’-ACAAAGCGACTGGATGAACC-3’ (reverse); GAPDH, 5’-GTCTCCTCTGACTTCAACAGCG-3’ (forward) and 5’-ACCACCTGTTGCTGTAGCCAA-3’ (reverse). The PCR reaction conditions were 95°C for 10 min, 95°C for 30 sec, 58°C for one minute and 72°C for 30 sec (40 cycles). Amplification was performed according to the manufacturer's cycling protocol and done in duplicate (Applied Biosystems 7300). Gene expression was calculated as 2-Δ(CT), where CT is cycle threshold, where DCT=(CT gene of interest - CT internal control).
Histopathology: The myocardial tissue was fixed in formalin and paraffin-embedded; 2-4 μm thick sections were stained with haematoxylin and eosin. The sections were evaluated under a light microscope for features of myofibril disarray, myofibril atrophy or hypertrophy, myocytolysis, features of nuclear degeneration, presence and extent of interstitial fibrosis, adipose tissue and inflammatory cells and vascular changes. Masson's trichrome stain was performed wherever indicated to look for the extent of fibrosis.
TUNEL (terminal deoxynucleotide-transferase- mediated dUTP nick end labelling) assay: Apoptosis was identified with in situ detection of TUNEL using a DNA fragmentation detection kit (Roche, USA). After de-paraffinization and rehydration, paraffin-embedded sections of P8 stage were incubated in freshly prepared permeabilization solution (0.1% Triton X-100, 0.1% sodium citrate) for two minutes on ice. After washing with PBS, the area around section was dried and 50 μl of TUNEL reaction mixture (5 μl deoxynucleotide-transferase enzyme in 45 μl labelled thymidine solution) was added on each section. The slides were incubated in a humidified atmosphere for 60 min at 37°C in the dark. The slides were rinsed three times with PBS and counterstained with Hoechst 33,258 (molecular probes, USA) nuclear stain and mounted in antifade mountant. The stained cells were visualized under a fluorescent microscope (Nikon Eclipse 80i; Nikon Instech Co. Ltd., Kawasaki, Kanagawa, Japan). For quantitative analysis, the apoptotic index was expressed as number of TUNEL-positive cells/100 nuclei (Hoechst stained) in 5μ heart section. Image Pro Plus 5.1 software (Media Cybernetics Inc, Silver Spring, USA) was used for image capturing and cell counting.
Statistical analysis: Non-parametric tests were utilized to obtain significance while comparing variables between the groups. Mann-Whitney U-test was applied to calculate significance in two values of a variable in two different groups. Fischer's exact test was used to analyze the categorical data between groups. Pearson's correlation between desired and relevant variables was performed. All analyses were carried out using SPSS 10 version for Windows (SPSS Inc., Chicago, IL, USA).
Results
There was no significant difference in the demographic and clinical profile of the patients with valve replacement and ASD (Table I). The effect of different chronic pressure loading condition was compared on the RV of patients with mitral stenosis. RVSP was significantly different in group I compared to group II [median (range): 37.5 mmHg (31-40) vs. 59.5 mmHg (42-122)]. RV dysfunction was significantly (P<0.05) more in groups II patients (21 of 30 patients) versus four of nine patients in group I. Caspase 3 and cytochrome c genes were expressed more in patients with valve disease with RVSP<40 mmHg (Table II). However, LV function in valve with higher RVSP was similar to patients with RVSP<40 mmHg though LV size was marginally smaller in high RVSP patients with LVES of 29.5 mm (16-48) in group II versus 30 mm (30-52) in group I (P=0.03) and LVED of 47.5 mm (32-76) in group II versus 55 mm (42-76) in group I, and LVEF of 60 per cent (59-60) in group II versus 56.5 per cent (50-65) in group I.
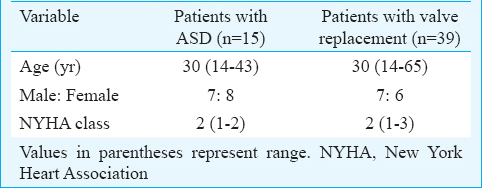
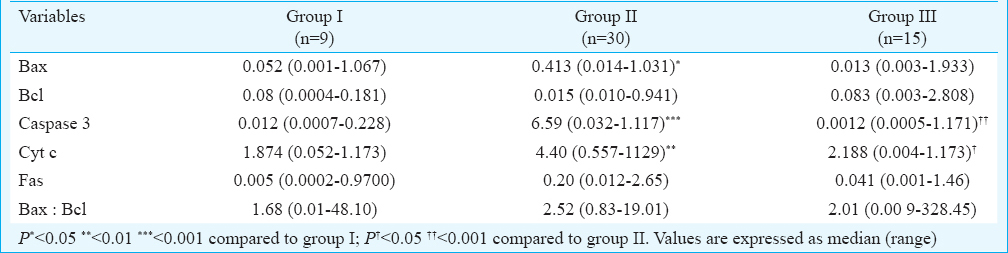
ASD and valve disease groups having comparable RVSP were compared; only difference between them was the cause for which they underwent open-heart surgery. RVSP (loading condition) was similar in both the groups, 37.5 mmHg (31-40) in group I versus 37 mmHg (28-40) in group III. RV function was similar in the two groups (RV dysfunction was present in 6 of 15 patients in ASD group and 4 of 9 patients in valve disease group). There was significantly higher expression of BAX, caspase 3 and cytochrome c genes in valve group (Table II). The patients in group III (ASD) presenting with the evidence of RV dysfunction (6/15 patients) expressed excess of cytochrome c (0.0226 in patients with no RV dysfunction vs. 0.0538 in patients with RV dysfunction, P=0.03). Valve disease patients had a larger LV size and marginally reduced LV functions with LVES 32 mm (30-52) in group I versus 23 mm (14-35) in group III (P=0.0001) and LVED of 55 mm (42-56) in group I versus 38 mm (31-46) in group III (P=0.0001) and LVEF of 56.5 per cent (50-65) in group I versus 60 per cent in group II (P=0.05).
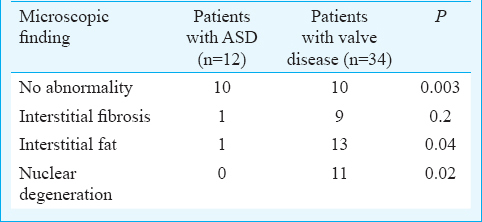
Comparison of microscopic findings in patients of groups I and II did not reveal any significant difference relating to the presence of interstitial fibrosis, interstitial fat deposition and nuclear degeneration. The microscopic findings in combined valve disease and ASD groups were compared. This comparison was done to observe if there were any difference in patients with valve disease that has inflammatory process as causative factor against simple volume overload condition that is devoid of inflammation (Table III, Fig. 1). Comparison revealed significant (P=0.04) amount of interstitial fat deposition (Fig. 1C) and nuclear degeneration (Fig. 1B) in the valve disease group. Nuclear degeneration was confirmed by TUNEL test in all the patients and was found to be confirmative of degeneration (Fig. 2). Interstitial fibrosis (Fig. 1D) was present in fair number of samples in higher amount in valve disease patients though it did not reach statistical significance. Significant number of sample in ASD group had normal myocardial histology (Fig. 1A). This difference of microscopic findings persisted while comparing valve disease with RVSP of <40 mmHg (group I) and ASD (group III) (Table IV).
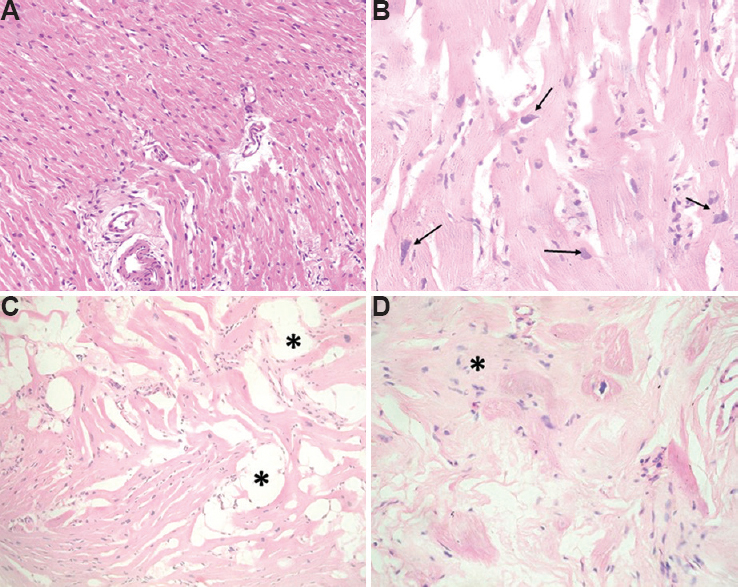
- Sections from myocardial biopsy (hematoxylin and eosin) showing (A) normal myocardium, (B) myofibrils with features of nuclear degeneration (arrows) with presence of nuclear enlargement, irregular nuclear contours and granular chromatin (×400), (C) interstitial deposition (asterisks) of mature adipose tissue (×200), (D) myofibril disarray (asterisk), fibre atrophy and marked interstitial fibrosis (×400).
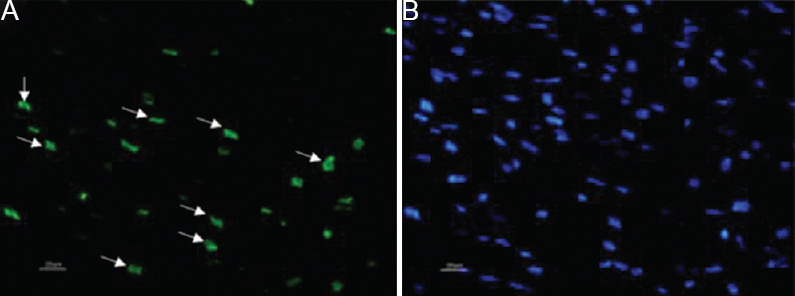
- (A) The cells showing green fluorescence are TUNEL positive and (B) Hoechst (blue) shows nuclear stain, i.e., total number of cells.
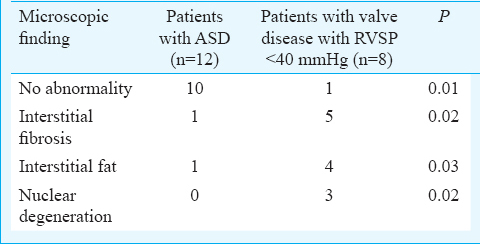
Expression of Bax had significant positive correlation with normal myocardium on histology (r=0.334, P=0.04). Nuclear degeneration observed on microscopy had strongly positive correlation with expression of Bcl (r=0.513, P=0.001), caspase 3 (r=0.506, P=0.001), FAS (r=0.479, P=0.002) and Bax (r=0.629, P=0.0001).
Discussion
In all patients, the left ventricular function was well preserved. All the valve disease patients had predominantly mitral stenosis. This eliminated the possibility of LV affecting the RV function. It was observed that LV was under filled in valve disease cases with high RVSP15. In the present study, we added a third group of ASD with RVSP<40 mmHg for comparison with the valve disease group having similar RVSP. RV dysfunction was significantly higher in patients of mitral stenosis with RVSP of ≥40 mm Hg when compared with valve disease group with RVSP<40 mm Hg, but there was no difference in RV function of group I and group III. Bogaard et al16 have reported that an elevated pulmonary artery pressure may not be the only reason for RV remodelling and failure. They opined that apoptosis might also play a role in RV remodelling and in the subsequent development of heart failure.
It was observed that the RV function, though similar in ASD and valve disease patients with RVSP<40 mmHg but the valve disease group had significantly higher expression of pro-apoptotic genes. This finding suggested the presence of milieu for apoptosis in valve disease. It was also noticed that the rise in BAX expression was significant and observed in both the valve disease groups when compared to ASD group. In animal study, the apoptosis was observed early and then declined when clinically manifested RV failure occurred17. This may be the possible explanation of reduction in caspase 3 and cytochrome c activity in patients with high RVSP. A positive correlation between pro-apoptotic gene expression favours mitochondrial pathway of cell apoptosis18.
BAX expression in valve disease groups is the starting point for stimulation of intrinsic pathway of apoptosis16. This is balanced by the expression of BCL2 gene, which is an anti-apoptotic gene19. This interplay between the two genes favours apoptosis in valve disease group. This triggers the cytochrome c that is mitochondrial pathway of stimulating the final pathway of apoptosis by activating caspase 320. This mitochondrial pathway is highly expressed in valve disease patients with RVSP<40 mmHg and thus sets the stage for RV dysfunction because of apoptosis in the later course of the disease. It is interesting to observe that the external pathway involving Fas which stimulates caspase 9 and finally caspase 3 is not expressed in this group of patients21. Fas have been shown to play a role in cardiac apoptosis in response to stretch in the muscle22.
An association has been shown between LV dysfunction and apoptosis23. Although RV may follow similar principle, there is no investigation of apoptosis and its role in dysfunction of RV. Abbate et al24 first reported the presence of apoptosis in RV after left ventricular infarction. Our study showed the evidence of favourable apoptotic environment persisting in the rheumatic valvular heart disease even before clinical and echocardiographic evidence of RV dysfunction.
Cardiac myosin has been shown to share resemblance with streptococcal M protein in rheumatic heart disease. This has been postulated as the cause of fibrosis in myocardial tissue25. Saikia et al26 demonstrated myocardial fibrosis on microscopy in samples from patients suffering with rheumatic heart disease. Absence of fibrosis in ASD group that has similar RVSP (<40 mmHg) as compared to one of the valve disease group indicates the presence of fibrosis as a result of rheumatic disease rather than haemodynamic consequence of RV strain27. Apoptosis, as evidenced by nuclear degeneration on microscopy and confirmed by TUNEL was absent in all the samples of ASD while present in 11 of 34 samples of valve disease groups. The positive correlation between expression of pro-apoptotic genes and apoptosis was shown to be significant in this study.
This study had certain limitations: (i) since this study was conducted with a small number of patients and the data was scattered within a large range, it is difficult to precisely comment on the significance achieved with respect to different variables compared, (ii)histological abnormality of fibrosis, fat and nuclear degeneration in this study was largely qualitative. Since this study was investigating the presence of these factors in the rheumatic patients, the quantitation was not planned, (iii)the patients with ASD served as controls. This was not the best control group, but probably the most appropriate control of person requiring cardiac surgery, (iv) TUNEL assay alone was considered for confirming the apoptosis in this study. Further study must be planned after removing these limitations to generate better understanding of the role of apoptosis and its mechanism in RV dysfunction.
In conclusion, apoptosis may be a possible mechanism of RV dysfunction in rheumatic mitral stenosis as shown by overexpression of pro-apoptotic genes and presence of nuclear degeneration that was confirmed by TUNEL assay. This process starts early in the course of valve disease when clinically evident RV dysfunction has not ensued. Later in the course, with chronically increased afterload expression of these genes, however, RV function continues to deteriorate.
Acknowledgment
This study was funded by research grant from Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow, India.
Conflicts of Interest: None.
References
- Pathophysiology and management of right heart ischemia. J Am Coll Cardiol. 2002;40:841-53.
- [Google Scholar]
- Importance of the right ventricle in valvular heart disease. Eur Heart J. 1996;17:829-36.
- [Google Scholar]
- Right ventricular ejection fraction is an independent predictor of survival in patients with moderate heart failure. J Am Coll Cardiol. 1998;32:948-54.
- [Google Scholar]
- Survival in patients with primary pulmonary hypertension. Results from a national prospective registry. Ann Intern Med. 1991;115:343-9.
- [Google Scholar]
- Longitudinal in vivo SPECT/CT imaging reveals morphological changes and cardiopulmonary apoptosis in a rodent model of pulmonary arterial hypertension. PLoS One. 2012;7:e40910.
- [Google Scholar]
- Pulmonary arterial hypertension in rheumatic mitral stenosis: does it affect right ventricular function and outcome after mitral valve replacement? Interact Cardiovasc Thorac Surg. 2009;9:421-5.
- [Google Scholar]
- Does endomyocardial biopsy aid in the diagnosis of active rheumatic carditis? Circulation. 1993;88:2198-205.
- [Google Scholar]
- Clinical characteristics relevant to myocardial cell apoptosis: analysis of pericardial fluid. Interact Cardiovasc Thorac Surg. 2004;3:359-62.
- [Google Scholar]
- Apoptosis in pressure overload-induced heart hypertrophy in the rat. J Clin Invest. 1996;97:2891-7.
- [Google Scholar]
- The remarkable right ventricle of patients with Eisenmenger syndrome. Coron Artery Dis. 2005;16:19-25.
- [Google Scholar]
- Quantitative assessment of pulmonary hypertension in patients with tricuspid regurgitation using continuous wave Doppler ultrasound. J Am Coll Cardiol. 1985;6:359-65.
- [Google Scholar]
- Doppler echocardiographic index for assessment of global right ventricular function. J Am Soc Echocardiogr. 1996;9:838-47.
- [Google Scholar]
- The relation between quantitative right ventricular ejection fraction and indices of tricuspid annular motion and myocardial performance. J Am Soc Echocardiogr. 2004;17:443-7.
- [Google Scholar]
- Long-term intravenous epoprostenol infusion in primary pulmonary hypertension: prognostic factors and survival. J Am Coll Cardiol. 2002;40:780-8.
- [Google Scholar]
- Chronic pulmonary artery pressure elevation is insufficient to explain right heart failure. Circulation. 2009;120:1951-60.
- [Google Scholar]
- Nicorandil prevents right ventricular remodeling by inhibiting apoptosis and lowering pressure overload in rats with pulmonary arterial hypertension. PLoS One. 2012;7:e44485.
- [Google Scholar]
- Effects of left ventricular volume overload on mitochondrial and death-receptor-mediated apoptotic pathways in the transition to heart failure. Am J Cardiol. 2009;103:1261-8.
- [Google Scholar]
- Cytochrome c and dATP-dependent formation of Apaf-1/caspase-9 complex initiates an apoptotic protease cascade. Cell. 1997;91:479-89.
- [Google Scholar]
- Stretch-mediated release of angiotensin II induces myocyte apoptosis by activating p53 that enhances the local renin-angiotensin system and decreases the Bcl-2-to-Bax protein ratio in the cell. J Clin Invest. 1998;101:1326-42.
- [Google Scholar]
- Right ventricular cardiomyocyte apoptosis in patients with acute myocardial infarction of the left ventricular wall. Am J Cardiol. 2008;102:658-62.
- [Google Scholar]
- Induction of myocarditis and valvulitis in lewis rats by different epitopes of cardiac myosin and its implications in rheumatic carditis. Am J Pathol. 2002;160:297-306.
- [Google Scholar]
- Adhesion molecule expression and ventricular remodeling in chronic rheumatic heart disease: a cause or effect in the disease progression – A pilot study. Cardiovasc Pathol. 2012;21:83-8.
- [Google Scholar]
- Ultrastructural pathological study of left ventricular myocardium in patients with isolated rheumatic mitral stenosis with normal or abnormal left ventricular function. Jpn Heart J. 1990;31:435-48.
- [Google Scholar]






