Translate this page into:
Evidence-based global cardiovascular disease control priority interventions
This editorial is published on the occasion of World Heart Day - September 29, 2018.
*For correspondence: m-huffman@northwestern.edu
-
Received: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
World Heart Day serves as a reminder that cardiovascular disease remains the leading cause of global deaths. While most countries have experienced age-adjusted declines in cardiovascular disease-related mortality over the past 25 years, India's rate has remained static1. Nearly 55 million Indians are estimated to have cardiovascular disease, and in 2016, 62.5 million years of life were prematurely lost in India due to cardiovascular diseases1. Substantial State-level variations exist in the cardiovascular disease burden in India, including a nine-fold variation in the burden of ischaemic heart disease (highest burden State: Punjab, lowest burden State: Mizoram)1. To help global, national and regional policymakers compare potential interventions, the third edition of the Disease Control Priorities Project identified evidence-based disease control priorities and priority interventions, including cardiovascular diseases, based on evidence synthesis of effectiveness, cost-effectiveness and extended cost-effectiveness, which includes the influence of interventions on financial risk protection2. Here we aim to (i) describe 14 evidence-based global cardiovascular, respiratory and related disease control priority interventions, (ii) identify opportunities and challenges for adaptation, implementation and scaling of priority interventions in India, and (iii) outline research to catalyze improvements in cardiovascular health in India.
Evidence-based global cardiovascular disease control priority interventions
The essential package of 14 priority interventions (Table) developed through the third edition of the Disease Control Priorities Project accounts for not only disease burden and effectiveness but also affordability and feasibility in a low- or lower-middle-income country context, such as India2. The interventions can be on the fiscal, inter-sectoral, public health, or personalized health service level, stratified by community, primary health centre, first-level hospital and referral or specialized hospital levels. There is substantial overlap with the World Health Organization's Noncommunicable Diseases Best Buys3, but differences exist when cost-effectiveness data are limited (e.g. fruit and vegetable subsidies, medical management of atrial fibrillation). While these interventions are potentially cost-effective, they were not included as part of the essential package. Further, while these interventions are evidence based, governments will also consider relative affordability, political commitment, subnational or regional disease burden and long-term budget planning based on the optimistic premise of a growing, ageing population when determining which interventions would be most appropriate for implementation.
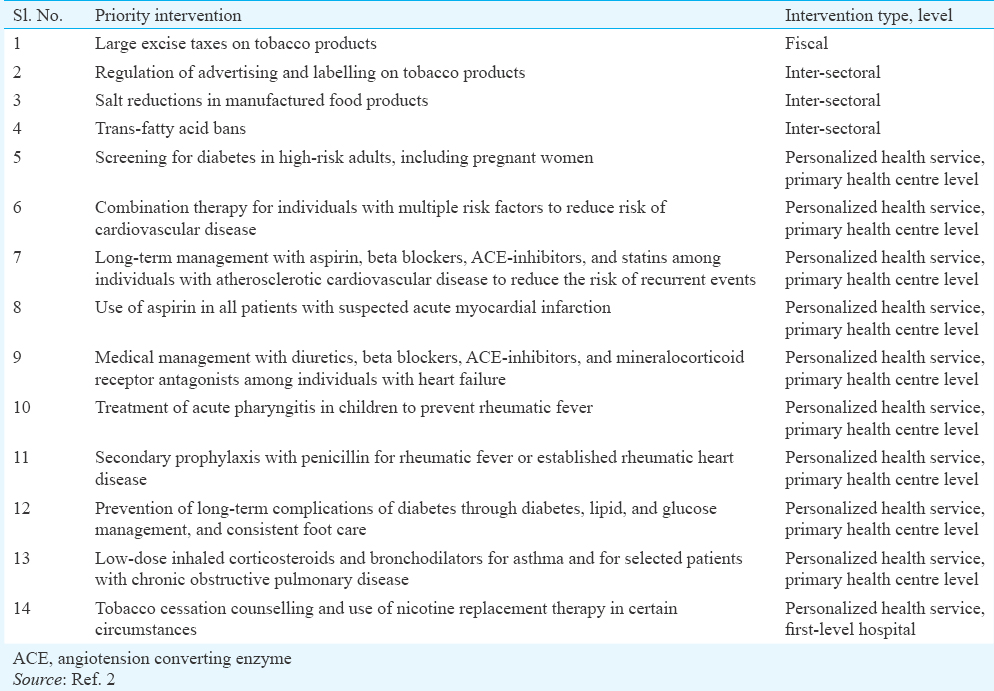
Fiscal and inter-sectoral interventions aim to reduce the burden of tobacco- and diet-related diseases, which are the leading causes of cardiovascular disease burden in India1. For example, tobacco taxes and regulation of advertising and labelling of tobacco products are components of the World Health Organization's and Framework Convention on Tobacco Control's MPOWER package. Further, reformulation of food products to reduce excessive sodium and eliminate artificial trans-fatty acids will be needed to reduce the burden of cardiovascular and related diseases. The May 2018 release of the World Health Organization's REPLACE package4 to eliminate artificial trans-fatty acids in the global food supply is a step that puts this goal into the broader global health spotlight.
Personalized health service level interventions are largely focused on the primary health centre level and include diabetes screening; combination therapy for cardiovascular disease prevention among individuals with or at high-risk for cardiovascular disease events; acute treatment with aspirin for acute myocardial infarction; antibiotics for acute pharyngitis, acute rheumatic fever or rheumatic heart disease secondary prevention and inhaled corticosteroids and bronchodilators for individuals with asthma and some individuals with chronic obstructive pulmonary disease. In the first-level hospital context, tobacco cessation counselling and nicotine replacement therapy in certain circumstances are also recommended.
Opportunities and challenges of priority interventions in India
In India, the opportunities and challenges for fiscal, inter-sectoral and personalized health service interventions exist in the wider socio-political context. For example, while tobacco remains the leading cause of preventable death in India5, the provision of large excise taxes requires political buy-in. Tobacco products sold in India are required to have pictorial warnings covering 85 per cent of the package based on the Cigarettes and Other Tobacco Products Act 20032, yet this labelling regulation has faced and withstood repeated legal challenges with its final implementation in April 2018. The provision of tobacco cessation counselling requires not only infrastructure to deliver such services, including call centres staffed by trained professionals, but also of sufficient size and linguistic diversity to match the needs of India's population. The availability and use of nicotine replacement therapy are limited by its exclusion from India's national essential medicines list6, despite being on the World Health Organization's Model List of Essential Medicines. Future expert panels may be receptive to adding nicotine replacement therapy to India's list.
Dietary regulation offers another avenue for reducing the burden of cardiovascular and related diseases, yet technical and socio-political challenges remain. For example, salt reduction strategies require consideration of iodine supplementation7, as well as historical considerations. Trans-fatty acid bans require upstream engagement and reformulation among not only food manufacturers but also oil manufacturers. In June 2018, the Food Safety and Standards Authority of India announced a target of less than two per cent trans-fatty acids in partially hydrogenated vegetable oils by 20222, and the draft regulations are under development. Dietary surveillance systems at the individual and food system levels, including related to sodium and trans-fatty acids, though remain in the development stage in India yet will be critically important for monitoring progress.
For treatment among individuals with or at high risk for developing atherosclerotic cardiovascular disease, combination therapy has been demonstrated to reduce the risk of cardiovascular events. When available, fixed-dose combination therapy is also recommended based on the improvements in adherence8 and health system efficiency gains. Despite the efficacy of medications including anti-platelets, statins and blood pressure lowering therapies in cardiovascular disease risk reduction, their long-term effectiveness can be limited by low persistence rates and relatively high costs. Individuals with heart failure face similar challenges though treatment with loop diuretics is commonly associated with symptomatic improvements that are more readily apparent to patients.
Treatment of acute myocardial infarction using aspirin is widely recommended and could even be administered at a primary health centre level. While modelling data demonstrate the cost-effectiveness of obtaining an electrocardiogram at the primary health centre level9, rapid referral to a hospital setting for reperfusion therapy is preferred. Once patients with an acute cardiovascular condition reach a hospital setting, strategies to promote high-quality, safe care remain under study10 and are imperative to improve overall health system performance.
Research to catalyze improvements in cardiovascular health
While implementation of evidence-based strategies will be an important strategy to reduce burden of cardiovascular diseases in India in the years ahead, future research will also be needed to catalyze improvements in cardiovascular health. On a fiscal level, further research developing, implementing and evaluating strategies for universal health coverage will be needed to ensure financial risk protection given the high rates of catastrophic health spending and distress financing associated with acute cardiovascular diseases11. On an inter-sectoral, policy-level, stronger evidence synthesis and health technology assessment research will improve evidence-informed policy-making. On a health system level, health management information system strengthening, coupled with robust risk factor and disease surveillance, will help India prioritize its interventions on national, State and local levels. Methods of task sharing, including through the use of traditional medical practitioners and practices, such as yoga, can also be studied. On a fundamental level, India can leverage the predilection for vascular disease that South Asians seem to face for discovery of new phenotypes and targets of intervention, though these will necessarily sit in the health system context. All areas will require a larger research workforce and sustainable funding mechanisms to build human resources and institutions in whom health research investments can be made. These pursuits should neither delay action, research, nor research training on broader levels yet should be considered mutually reinforcing.
India continues to face a disproportionate burden of cardiovascular disease compared with other countries around the world, yet priority targets and interventions have been developed to help improve the health and welfare of its people.
Financial support & sponsorship: The first author (MDH) received support from the National Heart, Lung, and Blood Institute, Bethesda, Maryland, USA for work related to this report (award R00HL107749). He also received support from the World Heart Federation to serve as senior programme advisor for the World Heart Federation's Emerging Leaders program, which is supported by unrestricted educational grants from Boehringer Ingelheim and Novartis with previous support by AstraZeneca and BUPA. He has also received support from the American Heart Association, Verily, and AstraZeneca for work unrelated to this manuscript. The last author (DP) received unrestricted education grants from Merck Sharp & Dohma (MSD), Eli Lilly, GlaxoSmithKline, Torrent and Sun Pharmaceuticals for primary care physician training programmes.
Conflicts of Interest: None.
References
- Cardiovascular diseases in India compared with the United States. J Am Coll Cardiol. 2018;72:79-95.
- [Google Scholar]
- Cardiovascular, respiratory, and related disorders: Key messages from Disease Control Priorities, 3rd edition. Lancet. 2018;391:1224-36.
- [Google Scholar]
- 2018. World Health Organization. Best buys and other interventions for prevention and control of noncommunicable diseases. Geneva: WHO; Available from: http://www.who.int/ncds/management/best-buys/en
- 2018. World Health Organization. REPLACE technical document. Geneva: WHO; Available from: http://www.who.int/nutrition/topics/replace-transfat
- Nations within a nation: variations in epidemiological transition across the states of India, 1990-2016 in the Global Burden of Disease Study. Lancet. 2017;390:2437-60.
- [Google Scholar]
- Availability, sales, and affordability of tobacco cessation medicines in Kerala, India. Circ Cardiovasc Qual Outcomes. 2017;10:pii: e004108.
- [Google Scholar]
- Dietary salt reduction and cardiovascular disease rates in India: A mathematical model. PLoS One. 2012;7:e44037.
- [Google Scholar]
- Fixed-dose combination therapy for the prevention of atherosclerotic cardiovascular diseases. Cochrane Database Syst Rev. 2017;3:CD009868.
- [Google Scholar]
- Pre-hospital ECG for acute coronary syndrome in urban India: A cost-effectiveness analysis. BMC Cardiovasc Disord. 2010;10:13.
- [Google Scholar]
- Effect of a quality improvement intervention on clinical outcomes in patients in India with acute myocardial infarction: The ACS QUIK randomized clinical trial. JAMA. 2018;319:567-78.
- [Google Scholar]
- A cross-sectional study of the microeconomic impact of cardiovascular disease hospitalization in four low- and middle-income countries. PLoS One. 2011;6:e20821.
- [Google Scholar]





